Chemical Agents – Gases
advertisement

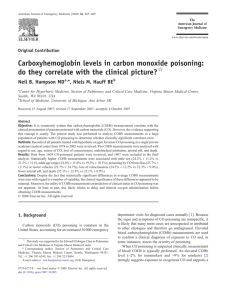
Chemical Agents:Dust Gases Metals & their Fumes Solvents Organic inorganic Sugarcane Silica Hay Coal Asbestos Chemicals Acid Alkalis Organic Irritants Primary Affecting Site of Absorption OR Asphyxiants Drugs Like (Heart of Total Hazards) Secondary Anaesthetic Solvents Secondary Ether Chloroform to absorption Benzene gives Systemic Toluene effects Simple Chemical Water Water Soluble Insoluble (Readily) ( Slightly Soluble) CO2 Methane, Hydrogen Aniline Hydrocarbon CO H2S HCN =================================================================================== GASES Carbon Monoxide (CO) TWA 8Hrs. = 50ppm TLV = 58 mg/M³ Characteristics:- Colourless, Odourless, non-irritant gas, which is slightly soluble in water & burns in air with bright blue red flame. It is the most widely encountered toxic gas in industry, commonly resulting from incomplete combustion of Carbonious Material. Most common operations of CO By-product Concentration 1) Blast Furnace Gas:- 20-25% CO. 2) Coal & Coke Oven Gas:- 7-16% CO. 3) Petrol & LPG:- 1-10% CO. 4) Diesel Engine Exhaust:- 0.1-0.5% CO. Mechanism of Action:1) It is a chronic Asphyxiant, because it combines with Hb, with an affinity 200-300 times more than that of Oxygen, to form Carboxy Haemoglobin COHb. CO also increases the Oxygen affinity of HB & causes the O₂ Dissociation Curve to shift to Left, by impending the release of O₂ to the tissues. 2) CO exerts a direct action by combining when other Haem containing Protein in the cells like Cytochrome Oxydase, Myoglobin, Cytochrome P₄₅₀. Interaction with Cytochrome Oxydase results in Mitochondrial Dysfunction & if it prolongs, impairment of Oxidative Mechanism. 3) Alternative Hypothesis:- CO damages Mitochondria by provoking the the release of free Nitric Oxide. 4) CNS Injury may also be due to Re-oxygenation injury as a result of production of potentially reduced Oxygen Spaces (Radicals), which in turn can oxidize Essential Proteins & Nucleic Acids & induce Brain Lipid Paroxydation. Blood CO Levels:1) Normal Subject:- Less than 1% 2) Occasional Smokers:- 5-6% 3) Heavy Smokers:- More than 10% Detection of CO in Air:- Previously they used to use Detector Tube. In Ditector Tube the colour changes & gives indication of CO Concentration. Now a days Electronic CO detectors, Dedicated CO Detectors are available. How to Calculate Atmospheric CO Exposure:% of COHb = K X % CO in Air X Minutes of Exposure Here K is a Constant = 3 for an individual at rest 5 for Sedentary Action 8 for Light Job 11 for Heavy Job. A less unknown hazard arises from the use of Methylene Chloride (Dichloro Methane), a widely used solvent, used in paint & warmish removal. Methylene Chloride is readily absorbed through Skin & Lungs, & Metabolized in Liver. CO is an important metabolite of Methylene Chloride & forms COHb. So it is Entoxification in the body. Clinical Features of CO Toxicity:Cherry Red Colour of Face & Skin:- “When You are Red You are Dead” . % of COHb Effects 1 2.5 – 4 % Decreased Short Term Maximal Exercise Duration in young healthy person. 2 Upto 5.1 % Decrease Exercise Duration further & there will be Chest Pain on Exertion, in patients with IHD. 3 Upto 20 % Equivocal Effects on Visual Perception. Motor & Sensory Motor Performance & Neuro behavioural Changes. 4 Upto 33 % 1) Decreased Oxygen Consumption with short term strenuous exercise. 2) Throbbing Headache. 5 Upto 50 % Dizziness, Nausea, Weakness & Collapse. 6 More than Unconscious & Death. 50% Diagnosis:- 1) Biochemical:- a) COHb level in Heparinized Blood Sample measured by CO_Oxymetere or by Spectrometer. b) In Post Martem by blood Gas Chromatographic Analysis is a preferred method, because of breakdown of Hb after death. 2) Clinically:- There is no diagnostic symptom complex. So the diagnosis is missed easily. The Clinical Presentation may vary widely with Vomiting, Headache, Malaise, Weakness, Fatigue, Chest Pain, Palpitation, Dyspnoea etc. Without adequate treatment 10 – 30% patients with severe toxicity may develop late neuro psychiatric manifestations within 3 to 240 days after exposure. Treatment of Acute Effect:- Without treatment Half life of CO is 4 Hours. 1) 100% Oxygene 2) Hyperbaric Oxygen at 2.5 Atm or more pressure:- Normal Atmospheric Pressure is 100 KPa. Hyperbaric is given at 252 KPa. The patient might rupture Alveoli or Tympanic Membrane. Hyperbaric Oxygen Therapy at 2.5 ATM Pressure Reduces the Half Life of COHb to 20 minutes. It also increases the amount of Oxygen dissolved in the blood to a concentration sufficient to meet the needs of the body, even without functioning haemoglobin percentage. It is sufficient to meet the tissue need of oxygen. Conditions for Hyperbaric Oxygen Therapy:1) Pregnant Woman 2) History of Unconsciousness. 3) Neurological & Psychiatric Symptoms. 4) If there are Cardiac Complications. 5) COHb is above 10%. Now a days in most of the Western Countries and Australia they start Hyperbaric treatment at COHb level above 25%. Late Effects:- They are due to 1) release of CO that was attached to Myoglobin and 2) Permanent CNS Damage A) Neuro Psychiatric Symptoms:- They may develop 2-3 weeks after. 1) Parkinsonism. 2) Visual Impairment. 3) Personality Changes:- Seen in 30% of cases like Irritability, Verbal Impairment, Verbal Aggressiveness, Violence, Impulsiveness, Moodiness. 4) Memory Impairment in 40% Cases. 5) Depression & Suicidal Thoughts. Mechanismof Neuro Psychiatric Symptoms:- Symptoms are mainly due to Anoxia and Specific Cytotoxic action of CO. That causes Necrosis of Globus Pallidus. It is a common lesion and may also be seen in Basal Ganglia, Hippocampus & White Matters. Diagnostic Tests for Neuro Psychiatric Symptoms:1) MRI 2) CAT (Computerized Axial Tomography) Scan 3) PET (Positron Emission Tomography) Scan. B) Cardiovascular System:- 1) Angina Pectoris 2) ECG Changes after Light or Moderate Exercise. C) Reproductive System:- 1) Low Birth Weight Babies to Pregnant Woman. 2) IUFD:- Intra Uterine Foetal Death. 3) Neurological abnormalities in Live Births.