Single-blinded, randomized preliminary study evaluating the effect
advertisement

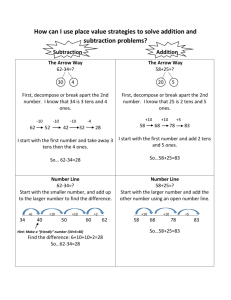
Single-blinded, randomized preliminary study evaluating the effect of transcutaneous electrical nerve stimulation on postoperative pain in patients with Colles' fracture Chou-Shin Lee1,2,MD, MS, Dian-Yue Lee3,MD, Jiann-Shyan Her4,MD, MS, Wen-Ling Liao2,5, Dr.PH and Ching-Liang Hsieh2,6,7*, MD, Ph.D. Department of Surgery, Yuanli Lee’s General Hospital, Lee’s Medical Corporation, Miaoli, Taiwan 1 2 Graduate Institute of Integrated Medicine, College of Chinese Medicine, China Medical University, Taichung, Taiwan 3 Department of Surgery, Dajia Lee’s General Hospital, Lee’s Medical Corporation, Taichung, Taiwan 4 Department of Ophthalmology, Nantou Hospital, Ministry of Health and Welfare, Nantou, Taiwan. 5 Center for Personalized Medicine, China Medical University Hospital, Taichung, Taiwan 6 Department of Chinese Medicine, China Medical University Hospital, Taichung, Taiwan 7 Research Center for Chinese Medicine and Acupuncture, China Medical University, Taichung, Taiwan *Corresponding author: Prof. Ching-Liang Hsieh, Graduate Institute of Integrated Medicine, College of Chinese Medicine, Graduate, China Medical University, 91 Hsueh-Shih Road, Taichung 40402, Taiwan. Tel: +886-4-22063366 (ext. 3500) Fax: +886-4-22037690 E-mail address: clhsieh@mail.cmuh.org.tw Running title: Transcutaneous electrical nerve stimulation treats postoperative pain Keywords: Transcutaneous electrical nerve stimulation; Postoperative pain; Colles' fracture 1 Abstract Objective: Transcutaneous electrical nerve stimulation (TENS) has been widely used for pain relief; however, the effect remains controversial. We hypothesized that TENS can relieve acute pain. Therefore, we designed a single-blinded, randomized, controlled preliminary study on postoperative pain in patients with Colles' fracture. Methods: In total, 36 patients were assigned to a real TENS or sham TENS group (18 patients in each group). TENS (50 Hz, 15 minutes/day) was applied near the Quchi (LI11) and Waiguan (TE5) surfaces of the operative side continuously 5 days after surgical treatment. Results: The visual analog scale (VAS) scores did not differ significantly between the real and sham TENS groups before the TENS period, from the first to fifth day after surgical treatment (all p > 0.05), whereas the VAS scores were lower for the real TENS group than for the sham TENS group in the post-TENS period, on the first, third, fourth, and fifth days after surgical treatment (all p ≦ 0.01). Conclusion: TENS might be valuable as a treatment of postoperative pain but clinicians and researchers should know that it is no different than a treatment with placebo. Especially, since this form of treatment and sham treatment has a great chance of working under the mechanism of the placebo effect due to its single-blindedness. 2 Introduction Colles' fracture, a distal forearm fracture, results from a fall in the position of an outstretched hand. The bone mineral density of patients below the mean value for their age has been reported to be suggestive of a close relationship with osteoporosis.1 The incidence of Colles' fractures is 1.7 per 1000 person-years in men and 7.3 per 1000 person-years in women in Europe,2 whereas that of distal forearm fracture is 9.0 per 10000 person-years in men and 36.8 per 10000 person-years in women aged 35 years and older in Britain, and a progressive increase is observed in women after perimenopause.3 Colles' fracture induced by low-energy injuries is most common in elderly people with osteoporosis and in postmenopausal women because of falling, whereas high-energy injuries result from traffic accidents or sport injuries in young adults.4,5 Colles' fracture is a closed fracture without displacement and can be treated with closed reduction cast fixation within 4–6 weeks.6-7 However, the treatment of the displaced fracture requires surgical operations such as open or closed reduction and fixation with implants.8,9 Although nonsteroidal analgesic drugs can be used to relieve postoperative pain, these drugs may induce side effects such as peptic ulcers and perforation and bleeding of the gastrointestinal tracat.10-12 Cyclooxygenase-2 (COX-2) inhibitor has been reported to reduce the aforementioned side effects; however, COX-2 inhibitors such as rofecoxil are associated with cardiovascular toxicity including the 3 induction of myocardial infarction or instability of blood pressure.13 Although opioids are often effective in pain relief, they have side effects such as nausea, vomiting, and respiratory depression.14 Therefore, we were interested in investigating alternative treatment methods that may reduce postoperative pain or the incidence of side effects induced by analgesic drugs. Transcutaneous electrical nerve stimulation (TENS) is a pain control method that involves applying electrical stimulation to the skin. Although TENS has been widely used to treat chronic pain or acute postoperative pain because it is a noninvasive and easy-to-use modality, the efficacy remains unclear.15 Therefore, this study designed a preliminary randomized controlled trial to investigate the effect of TENS on postoperative pain in patients with Colles' fracture. Materials and Methods Subjects Patients who were suffering from closed displaced Colles' fracture and required surgical treatment were recruited from the department of surgery, Yuanli Lee's General Hospital, Lee's Medical Corporation, Miaoli county, Taiwan, between June 16, 2009 and June 15, 2011. The protocol of the trial was approved by the institutional 4 review board of China Medical University hospital, Taichung city, Taiwan (IRM: DMR98-IRB-102), and written informed consent was obtained from all the participants before the trial.The trial procedures complied with the ethical principles dictated in the Declaration of Helsinki. The inclusion criteria in the present study were as follows: 1) age ranging from 20 to 80 years; 2) female or male; 3) no patient-controlled analgesia (PCA) experience; and 4) the subject or their legal representatives should have signed the informed consent. The exclusion criteria were as follows: 1) open Colles' fracture; 2) neurovascular injuries; 3) pregnancy or lactation; 4) severe arrhythmia or the use of heart pacemaker equipment; 5) epilepsy history; 6) severe medical disease such as uraemia, decompensated liver cirrhosis, and cancer; 7) psychosis unable to cooperate; and 7) TENS experience. Design and randomization This study was a single-blinded randomized controlled preliminary study. The randomization was obtained using computer-generated codes. Patients were randomly assigned to the real or sham TENS group by using the closed envelope technique. Sample size 5 The sample size was calculated according to our preliminary study, with at least 17 patients in each group if a 95% confidence interval with a power of 85% was used for the analysis. We hypothesized that the dropout rate was 5% because the trial was for only 5 days and the subjects were inpatients; therefore, the trial required 18 patients. Procedure of the trial and groupings The patients underwent surgical treatment under general anesthetics and they were sent to the recovery room after the completion of the surgical treatment. All the patients received an intravenous administration of keto (30 mg) as one type of nonsteroidal anti-inflammatory drug (NSAID), after which they were sent back to the ward if vital signs were stable and consciousness was clear. The TENS treatment started 4–6 hours after the patient was sent to the ward. The patients were randomly divided into a real or sham TENS group after the completion of the surgical treatment on the basis of the following: 1) real TENS group, the adhesive electrodes of the TENS were placed near the Quchi (LI11) and Waiguan (TE5) surfaces of the operative side. The TENS (TENS stimulator, HC-0501, Hometech, Taiwan) had a frequency of 50 Hz, and the intensity of stimulus was just enough to induce a visual muscle twitch of 15-minute duration each time per day and continuously for 5 days; and 2) sham TENS group, the method was identical to that of 6 the real TENS group; however, no electrical stimulus was applied. The position of electrodes was based on the principle of selection of adjacent and local points in traditional Chinese medicine (TCM) (Figure 1). Assessment All the patients routinely received oral cataflam (75 mg per day) as one type of NSAID. In addition, if the patients could not tolerate the pain, another intravenous administration of keto or another cataflam was given. The visual analog scale (VAS) scores, heart rate (HR), and blood pressure (BP) were assessed before TENS (before the TENS period) and 5 minutes after completion of the TENS treatment (post-TENS period) every day for 5 days continuously during admission. Total dose of PCA (morphine 40 mg, keto 60 mg, and butyrophenonel 2.5 mg were added to normal saline to produce 80 mL), number of times of vomiting, and total use of cataflam were recorded for 5 days after the surgical treatment. The assessment was performed by a well-trained experienced nurse who was blind to the groups. Primary outcome measures were VAS scores and the total dose of PCA. Secondary outcome measures were the total dose of cataflam and the total number of times of vomiting. 7 Statistical analysis All the baseline data of patients, VAS scores, BP and HR, total dose, number of times of PCA administration and the first time PCA administration was required, total dose of NSAID, number of times of nausea and vomiting, and number of patients were analyzed using independent t tests. The VAS scores from pre- and post- operation between real TENS group and sham TENS group for 5 days continuously during TENS admission was analyzed using a repeated measure ANOVA with two within factors, day and pre/post time and one between subjects factor, treatment group. We defined p < 0.05 to represent significant differences in this study. Results Basic characteristic data In total, 101 patients had closed displaced Colles' fracture and underwent surgical treatment. Sixty-five patients were excluded because of the following reasons: 1) 15 patients were older than 80 years, and 8 patients were younger than 20 years; 2) 12 patients refused to participate in the trial; 3) 8 patients had severe medical disorders; 4) 9 patients refused PAC use; and 5) 13 patients experienced TENS. Therefore, in total, 36 patients were included in the trial and they were randomly assigned to the sham 8 (18 patients) or real TENS group (18 patients). All the patients completed the trial (Figure 2). Basic characteristic data included age, body weight, body height, body mass index, HR, BP, and VAS scores before and after surgical treatment, which did not differ significantly between the groups (all p > 0.05; Table 1). Effect of TENS on primary and secondary outcomes A repeated measure ANOVA was conducted to compared the VAS scores from pre- and post- operation identity between real TENS group and sham TENS group across five time periods (from the first to fifth days). There was a significant interaction between pre/post time and treatment group (p < 0.001). The VAS scores did not differ significantly between the real and sham TENS groups before the TENS period, from the first to fifth day after the surgical treatment (the estimated mean VAS (SE) were 3.79 (0.20) and 3.67 (0.20) for sham TENS group and real TENS group, respectively, p = 0.66). After TENS, there was no significant interaction between treatment group and time (Wilks’ Lamdba = 0.809, F = 1.831, p = 0.148). There was a significant main effect for time (Wilks’ Lamdba = 0.238, F = 24.755, p < 0.001, partial Eta squared = 0.762), with both group of treatment showing a decrease in VAS scores across the five time points (the firth to fifth days). The main effect of 9 comparing the two groups of treatment was significant (F = 11.243, p = 0.002, partial Eta squared = 0.248), suggesting there was a significant difference in VAS score between real TENS group and sham TENS group (Figure 3). The total dose of PCA did not differ significantly between the groups for 5 days after surgical operation (p > 0.05; Table 2). Secondary outcomes including the total number of keto injections, total dose of cataflam, and total number of times of vomiting did not differ significantly between the two groups for 5 days after the surgical treatment (all p > 0.05; Table 2). Discussion The results of this study indicate that the VAS scores were lower in the real TENS group than in the sham TENS group during the post-TENS period, whereas the scores were similar for the two groups during the pre-TENS period after the surgical treatment in patients with Colles' fracture. In addition, the total dose of PCA, total number of keto injections, total dose of cataflam, and number of times of vomiting did not differ significantly between the real and sham TENS groups. Therefore, we suggest that TENS can reduce postoperative pain immediately; however, this effect of TENS is transient and cannot be maintained for 24 hours. In addition, TENS 10 treatment could not reduce the total dose of PCA, keto injection, and cataflam and the number of times of vomiting. However, the results could not exclude the placebo effect of TENS treatment due to the present study was a single-blinded design easily produced a bias. Numerous studies have considered TENS a noninvasive method of analgesia, such as for pain relief in the first stage of labor,16 for reducing operative pain in patients with laparoscopic sterilization,17 for reducing the demand of postoperative opioid in patients with spinal surgery,18 and for reducing analgesics of postoperative pain.19 In sum, the aforementioned reports conclude that TENS reduces pain, mainly acute pain, especially postoperative pain. This conclusion is consistent with the results of this study. By contrast, several reports have indicated that TENS cannot significantly provide relief from chronic pain.17,20,21 Several researchers have suggested that the reducing pain mechanism of TENS is possibly mediated through the increase in endorphins or reduction in the release of substance P.22-24 Electroacupuncture increases the concentration of β-endophin in the blood and brain in the mouse cancer pain model.24 Moreover, electroacupuncture increases the β-endophin levels and reduces cortisol levels in plasma in patients with osteoarthritis.22 The rapid catabolism of endorphins may explain the transient effect of TENS on pain relief.25,26 According to the theory of gate control, pain relief may be achieved by inhibiting the nociceptive 11 C-fiber through the stimulation of the afferent A-fiber in the dorsal column of the spinal cord.27 We assume that the inhibition of the nociceptive C-fiber requires continuous TENS stimulation to evoke the activity of the afferent A-fiber. Therefore, the effect of pain relief decreases or even disappears when TENS stimulation is stopped. This suggestion may partly explain the results of this study. This study has several limitations: 1) the sample size was extremely small; 2) the duration of TENS stimulation was short; 3) TENS can be set at a frequency of only 50 Hz, and the other parameters, such as intensity and the duration of stimulus, possibly affect the analgesic effect of TENS.19,28,29 Therefore, ways of stimulating the pain-relieving effect of TENS must be studied further. In conclusion, TENS might be valuable as a treatment of postoperative pain but clinicians and researchers should know that it is no different than a treatment with placebo. Especially, since this form of treatment and sham treatment has a great chance of working under the mechanism of the placebo effect due to its single-blindedness. Acknowledgments This study was supported by China Medical University under the Aim for Top University Plan of the Ministry of Education, Taiwan, and the Taiwan Ministry of 12 Health and Welfare Clinical Trial and Research Center of Excellence (MOHW104-TDU-B-212-113002). Contributors C-SL performed the experiment and wrote the paper; D-YL participated in the experiment and discussion; J-SH participated in the discussion; L-WL performed the statistical analysis; and C-LH participated in the discussion and design and revised the document. Competing interests None declared. 13 Reference 1. Wigderowitz CA, Rowley DI, Mole PA, Paterson CR, Abel EW. Bone mineral density of the radius in patients with Colles' fracture. J Bone Joint Surg Br 2000; 82: 87-89. 2. Silman AJ. Risk factors for Colles' fracture in men and women: results from the European Prospective Osteoporosis Study. Osteoporos Int 2003;14: 213-218. 3. O'Neill TW, Cooper C, Finn JD, Lunt M, Purdie D, Reid DM, Rowe R, Woolf AD, Wallace WA, UK Colles' Fracture Study Group. Incidence of distal forearm fracture in British men and women. Osteoporos Int 2001;12: 555-558. 4. Sakai A, Oshige T, Zenke Y, Suzuki M, Yamanaka Y, Nakamura T. Association of bone mineral density with deformity of the distal radius in low-energy Colles' fractures in Japanese women above 50 years of age. J Hand Surg Am 2008;33: 820-826. 5. Wigderowitz CA, Cunningham T, Rowley DI, Mole PA, Paterson CR. Peripheral bone mineral density in patients with distal radial fractures. J Bone Joint Surg Br 2003; 85: 423-425. 6. Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am 2000; 25: 19-28. 14 7. O'Connor D, Mullett H, Doyle M, Mofidi A, Kutty S, O'Sullivan M. Minimally displaced Colles' fractures: a prospective randomized trial of treatment with a wrist splint or a plaster cast. J Hand Surg Br 2003; 28: 50-53. 8. Wei DH, Raizman NM, Bottino CJ, Jobin CM, Strauch RJ, Rosenwasser MP. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate. A prospective randomized trial. J Bone Joint Surg Am 2009; 91: 1568-1577. 9. Kamano M, Koshimune M, Toyama M, Kazuki K. Palmar plating system for Colles' fractures--a preliminary report. J Hand Surg Am 2005;30: 750-755. 10. Al Mofleh IA, Al Rashed RS. Nonsteroidal, antiinflammatory drug-induced gastrointestinal injuries and related adverse reactions: epidemiology, pathogenesis and management. Saudi J Gastroenterol 2007;13:107-113. 11. Hernandez-Diaz S, Rodriguez LA. Association between nonsteroidal anti-inflammatory drugs and upper gastrointestinal tract bleeding/perforation: an overview of epidemiologic studies published in the 1990s. Arch Intern Med 2000;160: 2093-2099. 12. Wong VW, Chan FK. Cyclooxygenase-2 inhibitors in patients with high gastrointestinal risk: are we there yet? J Gastroenterol 2009; 44 Suppl 19: 53-56. 15 13. Dajani EZ, Islam K. Cardiovascular and gastrointestinal toxicity of selective cyclo-oxygenase-2 inhibitors in man. J Physiol Pharmacol 2008; 59 Suppl 2: 117-133. 14. Kehler H and Holte K, Effect of postoperative analysis on surgical outcome. British Journal of Anesthesia 2001; 67: 62-72. 15. Sluka KA and Walsh D. Transcutaneous electrical nerve stimulation: basic science mechanisms and clinical effectiveness. J Pain 2003; 4: 109-121. 16. Chao AS, Chao A, Wang TH, Chang YC, Peng HH, Chang SD, Chao A, Chang CJ, Lai CH. Pain relief by applying transcutaneous electrical nerve stimulation (TENS) on acupuncture points during the first stage of labor: a randomized double-blind placebo-controlled trial. Pain 2007;127: 214-220. 17. Desantana JM, Sluka KA, Lauretti GR. High and low frequency TENS reduce postoperative pain intensity after laparoscopic tubal ligation: a randomized controlled trial. Clin J Pain 2009; 25:12-19. 18. Unterrainer AF, Friedrich C, Krenn MH, Piotrowski WP, Golaszewski SM, Hitzl W. Postoperative and preincisional electrical nerve stimulation TENS reduce postoperative opioid requirement after major spinal surgery. J Neurosurg Anesthesiol 2010; 22:1-5. 16 19. Bjordal JM, Johnson MI, Ljunggreen AE. Transcutaneous electrical nerve stimulation (TENS) can reduce postoperative analgesic consumption. A meta-analysis with assessment of optimal treatment parameters for postoperative pain. Eur J Pain 2003;7:181-188. 20 Dubinsky RM, Miyasaki J. Assessment: efficacy of transcutaneous electric nerve stimulation in the treatment of pain in neurologic disorders (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2010; 74:173-176. 21. Deyo RA, Walsh NE, Martin DC, Schoenfeld LS, Ramamurthy S. A controlled trial of transcutaneous electrical nerve stimulation (TENS) and exercise for chronic low back pain. N Engl J Med 1990; 322:1627-1634. 22. Ahsin S, Saleem S, Bhatti AM, Iles RK, Aslam M. Clinical and endocrinological changes after electro-acupuncture treatment in patients with osteoarthritis of the knee. Pain 2009;147: 60-66. 23. Clement-Jones V ML, Tomlin S, Besser G, Rees L, Wen H. Increased beta-endorphin but not met-enkephalin levels in human cerebrospinal fluid after acupuncture for recurrent pain. Lancet 1980; 8201: 946–949. 24. Lee HJ, Lee JH, Lee EO, Lee HJ, Kim KH, Lee KS, Lee CH, Nam DW, Kim SH, Lee HJ, Ahh KS. Substance P and beta endorphin mediate electroacupuncture 17 induced analgesic activity in mouse cancer pain model. Acupunct Electrother Res 2009; 34: 27-40. 25. Pezalla PD, Lis M, Seidah NG, Chretien M. Lipotropin, melanotropin and endorphin: in vivo catabolism and entry into cerebrospinal fluid. Can J Neurol Sci 1978;5:183-188. 26. Reid RL, Hoff JD, Yen SS, Li CH. Effects of exogenous beta h-endorphin on pituitary hormone secretion and its disappearance rate in normal human subjects. J Clin Endocrinol Metab 1981; 52:1179-1184. 27. Garrison DW, Foreman RD. Decreased activity of spontaneous and noxiously evoked dorsal horn cells during transcutaneous electrical nerve stimulation (TENS). Pain 1994;58:309-315. 28 Chen CC, Johnson MI. An investigation into the hypoalgesic effects of high- and low-frequency transcutaneous electrical nerve stimulation (TENS) on experimentally-induced blunt pressure pain in healthy human participants. J Pain 2010; 11: 53-61. 29. Chesterton LS, Foster NE, Wright CC, Baxter GD, Barlas P. Effects of TENS frequency, intensity and stimulation site parameter manipulation on pressure pain thresholds in healthy human subjects. Pain 2003;106:73-80. 18 Legends Fig. 1 Two adhesive electrodes placed at the dorsal site of the wrists (near TE5) and lateral epicondyle of the elbows (near LI11). In the real TENS group, the patients received high-frequency (50 Hz) electrical stimulation for 15 minutes per day during 5 days of hospitalization. In the sham TENS group, no electrical stimulation was applied. Fig. 2 Flowchart Fig. 3 The effect of TENS on visual analog scale (VAS) scores. The VAS scores of the two groups did not differ significantly before TENS treatment; however, the VAS scores of two groups differed significantly (p = 0.002) after TENS treatment. Also, a significant time effect was observed (p < 0.001). 19 Table 1. Characteristics of the patients belonging to the real and sham TENS groups Age Body weight Body height Body mass index Systolic BP Diastolic BP Heart rate VAS(b) VAS(p) Real TENS Sham TENS p-value 53.9±13.0 60.5±9.0 157.4±6.8 24.3±2.71 139.9±13.1 83.4±14.7 78.8±9.7 8.67±0.91 5.56±0.92* 57.1±16.2 62.7±10.9 156.8±8.4 25.4±3.52 145.3±33.0 83.56±13.1 83.28±13.2 8.72±1.23 5.44±1.29* 0.529 0.519 0.829 0.325 0.543 0.972 0.251 0.878 0.786 The data are represented as mean ± standard deviation. Real TENS: patients received real TENS; Sham TENS: patients did not receive electrical stimulation from the TENS device; BP: blood pressure; VAS(b): score on the visual analog scale (VAS) presurgery; VAS(p): score on the VAS postsurgery; *p < 0.05 compared to VAS(b) for the same patient group. Table 2. Effect of TENS on postoperative pain in patients with Colles' fracture PCA (ml) Keto (times) Cataflam (tablets) Vomiting (times) Vomiting (number) Real TENS 27.1±10.8 2.2±1.5 16.6±2.1 0.22±0.5 Sham TENS 30.4±14.1 1.8±1.4 17.1±2.8 0.39±0.9 3 (16.7) 4 (22.2) p-value 0.446 0.367 0.546 0.489 1.000 Data are represented as mean ± standard deviation or number (%). Real TENS: patients received real TENS; Sham TENS: patients did not receive electrical stimulation from the TENS device; PCA: total dose of patient-controlled analgesia; Keto: total number of intravenous injections of Keto; Cataflam; total tablets of Cataflam; Vomiting (times): total incidences of vomiting in the patient group; Vomiting (number): number of patients in the group who vomited. 20