pbl3 mx of melanoma and nonmelanoma - Ipswich-Year2
advertisement
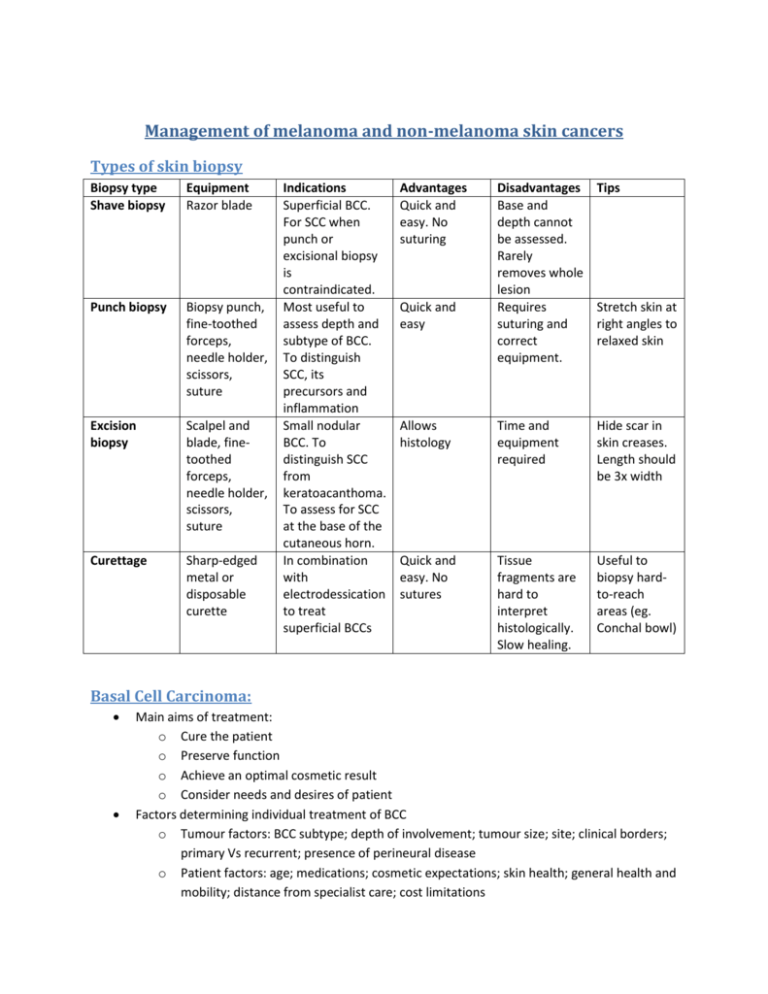
Management of melanoma and non-melanoma skin cancers Types of skin biopsy Biopsy type Shave biopsy Equipment Razor blade Punch biopsy Biopsy punch, fine-toothed forceps, needle holder, scissors, suture Excision biopsy Scalpel and blade, finetoothed forceps, needle holder, scissors, suture Curettage Sharp-edged metal or disposable curette Indications Superficial BCC. For SCC when punch or excisional biopsy is contraindicated. Most useful to assess depth and subtype of BCC. To distinguish SCC, its precursors and inflammation Small nodular BCC. To distinguish SCC from keratoacanthoma. To assess for SCC at the base of the cutaneous horn. In combination with electrodessication to treat superficial BCCs Advantages Quick and easy. No suturing Disadvantages Base and depth cannot be assessed. Rarely removes whole lesion Requires suturing and correct equipment. Tips Allows histology Time and equipment required Hide scar in skin creases. Length should be 3x width Quick and easy. No sutures Tissue fragments are hard to interpret histologically. Slow healing. Useful to biopsy hardto-reach areas (eg. Conchal bowl) Quick and easy Stretch skin at right angles to relaxed skin Basal Cell Carcinoma: Main aims of treatment: o Cure the patient o Preserve function o Achieve an optimal cosmetic result o Consider needs and desires of patient Factors determining individual treatment of BCC o Tumour factors: BCC subtype; depth of involvement; tumour size; site; clinical borders; primary Vs recurrent; presence of perineural disease o Patient factors: age; medications; cosmetic expectations; skin health; general health and mobility; distance from specialist care; cost limitations Options: o Standard surgical excision For nodular and sometimes superficial BCC 5-year cure rate: 90-98% for primary tumours Excision under local anaesthetic in an outpatient setting Pts should be referred if a flap or graft repair is required or the GP is not confident performing minor surgical procedures Send specimen for histology Take care in areas where nerves or other structures are involved Margin: 4mm lateral margin with inclusion of subcutaneous fat But for morphoeic and infiltrating tumours, use a 1cm lateral margins with subcutaneous fat being excised Advantages: definitive procedure; specimen for diagnosis and assessment of margins o Curettage and electrodessication For small, primary, superficial or nodular BCC with discrete borders Only use on trunk and limbs poor cosmetic result 96% cure if patients are selected appropriately 2-3 cycles of curettage under local anaesthetic (each cycle should be followed by electrodessication or diathermy at the base) Margin: 3-5mm Advantages: fewer bleeding problems in anticoagulated patients; quick and easy Disadvantages: electrical interference with pacemakers, if used on the legs of diabetic patients, wound can take up to 8 weeks to heal o Radiotherapy Used when surgery is contraindicated; or as palliation in advanced tumours 95% success with small BCCs, but recurrence can occur Advantages: painless; good early cosmetic result Disadvantages: multiple treatments are usually required, not recommended for patients under 60, poor long-term cosmetic results Curette biopsy can be useful to debulk the tumour o Moh’s surgery For high-risk BCC; or for those in a young patient with a cosmetically important site Performed under local anaesthetic by highly trained dermatologists Advantages: highest cure rates Disadvantages: training of specialist; expensive Send specimen for histological assessment o Imiquimod For superficial BCCs Excellent cosmetic results o o o o Disadvantages: protracted treatment (6 wks); unacceptably low cure rate for nodular BCC Must have breaks in treatment if the area is markedly inflamed reduces scarring Photodynamic therapy Superficial BCC; nodular BCC <2mm depth 1. Apply a photosensitizing cream (eg. 5-aminoevulinic acid or its methyl ester) 2. Occlude for 3-5 hours to allow absorption 3. Expose area to a light source of appropriate wavelength to form reactive oxygen species Usually 2 treatments 1-4 weeks apart has 90% response rates Excellent cosmetic results Disadvantages: painful, expensive Can minimize pain using a local anaesthetic Ideally the BCC should be debulked before treatment Cryotherapy Has limited use only small, low-risk superficial BCC on trunk or proximal limbs Must biopsy first and mark out BCC and margin before treatment Advantages: quick, easy Disadvantages: slow to heal; white scar; poor cure rate; cannot use on head and neck BCCs Laser Can be used for superficial BCC, but at considerable cost to the patient Local anaesthetic, wound heals by secondary intention Cytotoxic agents (eg. 5-fluorouracil) Topical, but with low cure rates Squamous Cell Carcinoma Aims of treatment o Complete eradication of the lesion o Preserve function o Best possible cosmetic outcome Options o Standard surgery Most primary SCCs 80-90% five-year success rate Margin: 4 or 10mm (for <2cm or >2cm diameter respectively) Advantages: specimen for assessment Disadvantages: must take care to avoid damaging other structures o Mohs’ surgery For large, recurrent or incompletely excised SCCs Disadvantages: expensive; time-consuming; extra training for dermatologists o o o o o o o Radiotherapy Only use when surgery is contraindicated or inappropriate OR if the SC is advanced (then use radiotherapy to complement surgery) Generally not for patients under 60 About 10 treatments over several weeks Advantages: non-invasive; can treat multiple lesions in one setting; painless Curettage and electrodessication For small, thin lesions on the trunk and limbs For solar keratoses, Bowen’s disease and keratoacanthomas, but not ideal for invasive SCCs Not for very thin skin (eg. eyelids and lips) 3-5mm margin with 2-3 cycles of curettage 95% cure rate Wound heals by secondary intention in 2-4 weeks Imiquimod For thin lesions (eg. solar keratoses, Bowen’s disease) Apply daily for 5 days per week over 6 weeks Very good cosmetic results Photodynamic therapy For thin lesions (eg. solar keratoses or Bowen’s disease) 80-90% cure Excellent for sites of poor wound healing (eg. lower legs) Good cosmetic results Cryotherapy For thin lesions (eg. solar keratoses or Bowen’s disease) Disadvantages: longer healing time, hypopigmented scar Lasers For thin (not invasive) SCCS 5-FU cream For diffuse solar keratoses on a large area Cream is applied nightly for 4 weeks Melanoma Initial biopsy o For suspected melanomas, the biopsy should be a complete excision to help prevent false negatives and to allow assessment of tumour thickness o It is generally better not to attempt a wide definitive margin at the time of initial excision and to avoid complex closure (eg. graft, flap) for excisional biopsy 2mm margin is optimal for initial biopsy followed by definitive excision Do not want to use skin grafts or flaps because this compromises closure for the definitive procedure Management and follow-up o Refer if: Difficult histopathology High risk primary melanoma Metastatic melanoma To evaluate other pigmented lesions Consider adjuvant protocols or research For specialised melanoma procedures Anxious patient o Evaluate patients’ risks for developing future melanomas o Be aware of atypical presentations of melanomas o Listen carefully to the concerns expressed by the patient about changing lesion(s) o Always examine the scalp, soles of feet and between the toes during a total-body skin examination o Ensure appropriate aids are used to diagnose melanomas dermoscopy, total body photography o Multidisciplinary care should incorporate a reassessment of histological evidence and fully explain the disease and treatment options to the patients. o Complete skin examination is essential and performed at least annually For palliative therapy, can use surgery, chemotherapy or radiation