Basal Cell Carcinoma
•
•
•
•
•
Presented by:
Bill V. Way, D.O.
AOCD Board Certified Dermatologist
Residency in US Army at Walter Reed
Consultant for Charlton Methodist Hosp for
past 19 years
Epidemiology and Etiology
•
•
•
•
•
Incidence US 500-1000 per 100,000
>400,000 new patients annually
Age usually over age 40
Sex Males >Females
Race rare in brown and black skinned pt
Diagnosis
• High index of suspicion
• Onset
• Prior treatment
Types of BCC
•
•
•
•
•
•
Supeficial BCC
Nodular BCC
Pigmented BCC
Cystic BCC
Sclerosing or Morpheaform BCC
Recurrent BCC
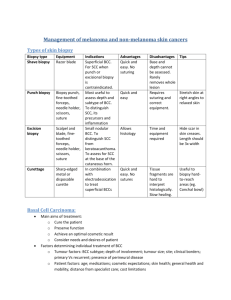
Biopsy
• Biopsy: Shave, Punch,Excision
• Specimen to reliable dermatopathologist or
pathologist
What to Biopsy
• Select a good representation of the lesion
for biopsy
• If small lesion, biopsy the entire lesion
• Final treatment code is dependent on actual
size of lesion at time of biopsy
• Get exact measurements of lesion, digital
photo if possible
When should you do a biopsy?
• If you are unsure of diagnosis of lesion and
have in the differential a skin cancer, basal
cell carcinoma, squamous cell carcinoma or
melanoma, then do a biopsy
• List your differential in the order which you
think the lesion is. Learn from your errors.
Methods of Biopsy
• Shave Biopsy: easiest and fastest
• Punch Biopsy: depth of lesion
• Excisional Biopsy: > time, > expense,
complete removal of tumor
• Incisional Biopsy: partial removal of tumor,
>time, > expense
Shave Biopsy
•
•
•
•
•
•
•
Xylocaine 2% with epi
1cc tuberculin syringe, 30g needle
Non-sterile gloves
#15 sterile blade Bard Parker
Specimen bottle, labeled correctly
Drysol solution
Bacitracin Ointment, Bandaid
Punch Biopsy
•
•
•
•
•
•
•
Xylocaine 2% with epi
1cc tuberculin syringe, 30g needle
Sterile gloves
Punch : 2mm, 3mm, 4mm, 6mm
Minor surgery tray, suture size for area
Specimen bottle labeled correctly
Bacitracin Ointment and bandaid
Excision or Incisional Biopsy
•
•
•
•
•
•
Xylocaine 2% with epi
3-5cc syringe, 30g needle, sterile gloves
#15 or #11 sterile blade, surgery tray
Suture for area, absorbable, non-absorbable
Specimen bottle labeled correctly
Bacitracin Ointment and sterile dressing
Treatment of BCC
•
•
•
•
•
•
•
Electrodesiccation and curettage
Excision
Cryosurgery
Moh’s Surgery
Radiation
5-Fluorouracil
Aldara (Imiquimod)
Electrodesiccation & Curettage
•
•
•
•
•
•
Hyfrecator
Curettes: 2mm, 3mm, 4mm
EDC times 3
Expect scar formation
85-90% cure rate
Check for Pacemaker, Defribralator
Excision
•
•
•
•
•
•
Adequate outline of tumor margin
Adequate margins 3-5mm
Surgery Tray, Hyfrecator
Suture: absorbable, non-absorbable
Tag tip, specimen labeled correctly
Pressure dressing, antibiotic ointment
Cryosurgery
Used only for superficial and small nodular
BCC
Not indicated for deeper BCC
High morbidity, very painful
Moh’s Surgery
• Can be used on all BCC
• Difficult lesions: sclerosing or recurrent, poorly
defined borders, tumors of nose, eyelids
• Recurrent lesions
• Lesions over 25mm dia
• 98% cure rate
• Expensive, > time
• Few Moh’s Surgeons, Dermatologist
Radiation therapy
•
•
•
•
For elderly pt who can not tolerate surgery
Useful for eyelids and lips
Requires several outpt visits
If used in young pt can lead to development
of SCC or recurrent BCC later in life at
same site
5-Fluorouracil
• Should not be used today
• Can destroy surface without affecting
deeper bcc cells
Prevention
•
•
•
•
•
Frequent skin examination q 3 months
Yearly by PCP or Dermatologist
Sunscreens SPF 15 or higher
Protective clothing, hats, sunglasses
Team approach: Patient, Family, Doctor
Remember
• Look at all the patient’s skin, especially the
sun exposed skin.
• Biopsy ?? Lesions
• Treat if trained and comfortable
• Otherwise refer to a more qualified
physician: Dermatologist, Moh’s Surgeon,
Plastic Surgeon
• Follow patients frequently
Thank you
• We look forward to future lectures and
having you each do rotations in
dermatology if possible.