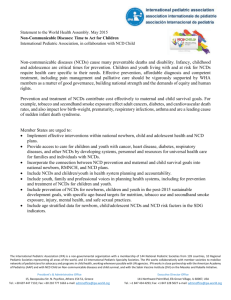
Non-communicable diseases and health information systems
advertisement

Non-communicable diseases and health information systems in the Pacific region Alan LopezHebe N Gouda, Nicola Hodge, Carla AbouZahr, Audrey Aumua, Robert Beaglehole, Colin Bell, Amanda Benson , Ruth Bonita, Mark Durand, Charles Gilks, Damian Hoy, Lene Mikkelesen, Bruce Neal, Tueila Percival, Rasika Rampatige, Graham Roberts, Boyd Swinburn and 1 Working Paper Series Number ?? March 2013 WORKING PAPER 2 About this series The Health Information Systems Knowledge Hub’s Working Paper Series is the principal means to disseminate the knowledge products developed by the hub as easily accessible resources that collectively form a lasting repository of the research findings and knowledge generated by the hub’s activities. Working papers are intended to stimulate debate and promote the adoption of best practice for health information systems in the region. The series focuses on a range of knowledge gaps, including new tools, methods and approaches, and raises and debates fundamental issues around the orientation, purpose and functioning of health information systems. Generally, working papers contain more detailed information than a journal article, are written in less academic language, and are intended to inform health system dialogue in and between countries and a range of development partners. Many working papers have accompanying products such as summaries, key points and action guides. The full range of documents, as well as other resources and tools, is available on the Health Information Systems Knowledge Hub website at www.uq.edu.au/hishub/publication-tools. This research has been funded by AusAID. The views represented are not necessarily those of AusAID or the Australian Government. Author details Hebe N Gouda, Nicola Hodge, Audrey Aumua, Charles Gilks, Lene Mikkelesen, Rasika Rampatige and Alan Lopez School of Population Health, University of Queensland Carla AbouZhar Independent consultant Robert Beaglehole, Ruth Bonita, Tueila Percival and Boyd Swinburn University of Auckland, New Zealand Colin Bell Western Pacific Regional Office, World Health Organisation Amanda Benson Nossal Institute for Global Health, University of Melbourne Mark Durand Pacific Island Health Officers Association Damian Hoy Secretariat of the Pacific Commission, Noumea Bruce Neal George Institute for Global Health and the University of Sydney Graham Roberts University of New South Wales 3 The authors would like to thank Neal Pierce for reading and commenting on the paper. Further thanks for contributions made by Michael Buttsworth, Taralina Gae'e-Atefi, Mark Power, Jillian Ridley, and Anna Rodney. © The University of Queensland 2013 Published by the Health Information Systems Knowledge Hub, School of Population Health, The University of Queensland Public Health Building, Herston Rd, Herston Qld 4006, Australia Please contact us for additional copies of this publication, or send us feedback: Email: hishub@sph.uq.edu.au Tel: +61 7 3346 4732 Fax: +61 7 3365 5442 www.uq.edu.au/hishub Edited by Econnect Communication Design by ?? 4 Contents Figures ..................................................................................................................................................... 6 Tables ...................................................................................................................................................... 7 Acronyms and abbreviations .................................................................................................................. 8 Summary ............................................................................................................................................... 10 1. Background ................................................................................................................................... 12 1.1 Introduction .......................................................................................................................... 12 1.2 Guiding values and principles underlying health information systems in the Pacific .......... 13 1.3 Strengthening health information systems for non-communicable diseases in the Pacific. 14 1.4 Priority interventions and interventions that work .............................................................. 16 2. The WHO global monitoring framework and the Pacific .................................................................. 17 2.1 Data availability..................................................................................................................... 17 2.2 Proposed targets and indicators for the Pacific .................................................................... 24 2.3 Prioritising targets and indicators ......................................................................................... 30 2.4 Trade, regulatory mechanisms and non-communicable diseases........................................ 32 2.5 Data sources.......................................................................................................................... 33 3. Capacity and coordination ................................................................................................................ 38 3.1 Building capacity for civil registration and vital statistics ..................................................... 38 3.2 Generating and managing data ............................................................................................ 38 3.3 Building analytical capacity ................................................................................................... 39 3.4 Building institutional capacity ............................................................................................... 40 3.5 Coordinating efforts .............................................................................................................. 40 4. Regional governance ......................................................................................................................... 42 4.1 The potential role of a regional non-communicable disease monitoring alliance ..................... 42 4.2 Translational research................................................................................................................. 43 5. Conclusion ......................................................................................................................................... 44 References ............................................................................................................................................ 46 5 Figures Figure 1 Strengthening a health information system to monitor and control non-communicable diseases in Pacific Island Countries and Territories....................................................................................................... 15 Figure 2 The three pillars of non-communicable disease (NCD) surveillance (Source: WHO) ............................. 25 Figure 3 Prioritisation of indicators and data sources .......................................................................................... 32 Figure 4 Population-based and institution-based data sources (Source: HMN 2008) ......................................... 34 Figure 5 High priority actions to improve and strengthen data sources .............................................................. 37 6 Tables Table 1 Pacific Island Countries reporting on non-communicable disease (NCD) indicators ............................... 19 Table 2 Year of survey and year of reports for three population surveys in Pacific Island Countries and Territories .................................................................................................................................................... 24 Table 3 Global monitoring framework targets and indicators for the prevention and control of noncommunicable diseases .............................................................................................................................. 26 7 Acronyms and abbreviations AusAID Australian Agency for International Development BAG Brisbane Accord Group CDC Centre for Disease Control CNMI Commonwealth of the Northern Mariana Islands CRVS civil registration and vital statistics CVD cardiovascular disease GHPS Global Health Professionals Survey GMF Global Monitoring Framework GSPS Global School Personnel Survey GSHS Global School-based Student Health Survey GTSS Global Tobacco Surveillance System GYTS Global Youth Tobacco Survey HIA health impact assessments HISHub Health Information System Knowledge Hub HIV/AIDS human immunodeficiency virus/acquired immunodeficiency syndrome HMN Health Metrics Network HPV human papillomavirus ICT information and communications technology INDEPTH International Network for the Demographic Evaluation of Populations and their Health IT information technology MDGs Millennium Development Goals NCD non-communicable disease NZAID New Zealand Aid Programme PAHO Pan-American Health Organization PBCR population-based cancer registries PEN package of essential non-communicable [disease interventions] PHIN Pacific Health Information Network PICTs Pacific Island Countries and Territories PNG Papua New Guinea SARA Service Availability and Readiness Assessment SPC Secretariat of the Pacific Community STEPS STEPwise Approach to Risk Factor Surveillance for NCDs UNAIDS Joint United Nations Programme on HIV/AIDS 8 UNESCO United Nations Educational, Scientific and Cultural Organization UNICEF United Nations Children’s Fund USAID United States Agency for International Development WHO World Health Organization WPRO World Health Organization – Pacific Region Office 9 Summary According to the Ninth Meeting of Ministers of Health for the Pacific Island Countries (WHO WPRO 2011), the Pacific region is in the midst of a non-communicable disease (NCD) epidemic which has reached crisis point. Urgent and deliberative action is necessary such as cardiovascular disease and stroke. The World Health Organization has developed the ‘Global action plan for the prevention and control of non-communicable diseases 2013–2020’ and ‘A comprehensive global monitoring framework including indicators and a set of voluntary global targets for the prevention and control of noncommunicable diseases’ (WHO 2012a). An expert panel was brought together by the Health Information Systems Knowledge Hub to assess the application of the WHO global monitoring framework to Pacific health information systems. The panel also considered the implications to health information systems in Pacific Island Countries and Territories of supporting national and health system responses to the NCD epidemic. In this working paper, we present the issues highlighted by the expert panel and set out recommendations for strengthening health information systems in the Pacific region. We endorse a hierarchical approach to applying the global monitoring framework NCD targets. Countries should focus efforts on interventions that are known to have large health impacts and that are feasible and cost-effective. To this end, we identify the parts of health information systems in the Pacific that require strengthening and capacity building. Strengthening national civil registration and vital statistics systems is crucial so that reliable mortality-by-cause data can be collected and used. Integrating NCD surveillance into health information systems is important to provide much- needed evidence on prevalence and trends in age- and sex-specific risk factors. Health information systems usually collect and compile data from national health systems, vital registration systems and population-based surveys. However, the severity of the NCD epidemic demands that these systems go beyond the traditional sources of information. Health information systems in the Pacific should incorporate information about trade regulations, national policies and implementation programs intended to control access, costs and the quality of potentially harmful products such as processed foods, as well as further limit access to tobacco and alcohol. To do this, the potential desirable outcomes of this response must be defined and tracked systematically to show what impact these measures have on individual jurisdictions and allow comparison between jurisdictions. In this paper, we also identify areas that should be incorporated into the health information systems mandate, including investigations into the incremental costs of surveillance activities and core policy interventions. Clarifying the direct and hidden costs and benefits associated with NCDs and interventions is likely to help advance the policy agenda surrounding NCDs. This working paper also recommends a structure for regional NCD governance that can harmonise monitoring, prevention and control efforts and coordinate capacity-building activities for Pacific Island Countries and Territories. 10 Key recommendations for Pacific Island Countries and Territories 1. Strengthen, as a matter of urgency, the civil registration systems and vital statistics in Pacific Island Countries and Territories (PICTs) to provide mortality by cause information which is essential for monitoring progress on NCDs. 2. Maintain focus on a few high-priority cost-effective interventions that bring the greatest health benefit to all people and surveillance should reflect these priorities. Targets and indicators of the global monitoring framework must be prioritised to suit the Pacific issues and capacities. Targeting tobacco use, unhealthy diets and an approach to treat those at high risk of cardiovascular diseases are the three top priorities and this should be reflected in prioritised surveillance actions. 3. Expand on the GMF to include accountability indicators of NCD risk factors. These include trade agreements and policies to regulate the prices. Access to tobacco, alcohol and unhealthy foods should be better monitored and PICTs should agree on a prioritised list of these upstream factors. 4. Integrate the STEPwise approach to risk factor surveillance for NCDs (STEPS) survey and the Global School-based Student Health Survey (GSHS) into the routine data collection systems. STEPS should be kept as simple as possible when incorporating modules on salt consumption and access to treatment to prevent heart attacks and strokes in high-risk groups. The age range for STEPS sampling should also be extended to 18 years and above to fill the gap currently left between STEPS and GSHS. This modified survey should be administered every five years in PICTs. Biological samples for the STEPS survey can be collected on alternate cycles. 5. Improve capacity in the Pacific, as a matter of urgency, by taking concerted and coordinated action to deal with human resource shortfalls which are a major impediment to strengthening health information. 6. Address the urgent need for research on the costs and benefits of interventions and monitoring different indicators. 7. Develop an external body under country ownership to strengthen surveillance activity in the Pacific region by: identifying gaps in country capacities, helping coordinate capacity building efforts, identifying research priorities, and providing technical support for data management, data analysis and knowledge dissemination. 11 1. Background 1.1 Introduction Non-communicable diseases (NCDs) are increasingly being recognised as a global issue which threatens economic development and imposes heavy financial costs on households. The resources available at national and regional levels are neither in proportion to the burden of NCDs, nor adequate to address the challenge (The World Bank 2012). Recent estimates taken from the WHO 2009 ‘Western Pacific regional action plan for the prevention and control of noncommunicable diseases (2014-2020)’ and Lozano et al. (2012) suggest that NCDs are leading causes of death in Pacific Island Countries and Territories (PICTs) and responsible for over 70 per cent of all deaths annually. Many of these deaths are preventable and share common risk factors. NCDs such as stroke and diabetes can result in many years of chronic illness and place a debilitating burden on families and health systems. Pacific health leaders have aptly described the NCD situation in the region as a ‘crisis’ and have issued a regional declaration of health emergency. The high-level meeting of the United Nations in 2011 addressed NCDs and raised them to a position of high priority on the global health agenda. The political declaration recognised NCDs as a ‘human, social and economic crisis requiring an urgent and comprehensive response’. The declaration calls for all member states to include NCDs in health planning processes and development agendas. In May 2012, the World Health Assembly set a goal to reduce the burden of premature mortality due to NCDs by 25 per cent by the year 2025. In May 2013, the World Health Assembly endorsed the final version of the World Health Organization (WHO) ‘Global action plan for the prevention and control of non-communicable diseases 2013–2020’ and the ‘Comprehensive global monitoring framework, indicators and targets for the prevention and control of NCDs’ (GMF). This represented consensus among member states on the purpose, methods, roles and responsibilities towards NCD monitoring, prevention and control. The GMF includes a set of nine voluntary time-bound targets and 25 indicators to track progress. It provides an important platform for political support to integrate NCDs into national health and development planning and monitoring. A regional NCD action plan has also been prepared. In addition to the indicators outlined in the GMF, it also proposes to monitor country performance by establishing national multi-sectoral action plans, reporting on the global targets and integrating NCDs into the United Nations Development Assistance Framework (WHO 2002). Collecting data to inform health planning and decision-making requires concerted and coordinated efforts. This poses challenges for many low-resource countries, such as PICTs, which struggle to develop and maintain health information systems with sufficient capacity to collect and analyse data and to effectively report on the health of their populations. Health information systems in the Pacific suffer from critical gaps and weaknesses. This is particularly true for NCDs which can often go undiagnosed, untreated and/or unreported. Surveys from which NCD data is attainable are often dated and much of what we know about NCD mortality in the Pacific is based on crude estimates. In February 2013, the Health Information Systems Knowledge Hub (HISHub) at the University of Queensland hosted a workshop bringing together an expert panel to discuss the key implications of the proposed NCD monitoring and control framework on health information systems and their strengthening in Pacific countries. The workshop reviewed the GMF and proposed priorities for the framework that aim to maximise the cost-effectiveness of the targets and indicators appropriate for the Pacific. In addition to this, the panel sought to identify key areas of applied research and regional governance that could enhance the implementation of the WHO framework and ultimately control or prevent NCDs. 12 1.2 Guiding values and principles underlying health information systems in the Pacific The expert panel defined the guiding values and principles that underlie health information systems in the Pacific (see Panel 1). The primary values that should support and permeate all work to strengthen health information systems in the Pacific are equity and country ownership. When possible, monitoring efforts should incorporate indicators of socio-economic status as a marker for inequalities in risk factor levels. With appropriate technical guidance, monitoring strategies should be developed and implemented by countries, and, to the greatest extent possible, integrated into existing systems. In addition to these values, at the centre of all NCD monitoring and health information system strengthening activities in the Pacific should be the following six guiding principles. The approaches taken must be informed by sound scientific evidence and best possible practice. To be useful in informing actions indicators should be clear and simple for easy interpretation. The development of monitoring strategies must consider logistical challenges and resource limitations to ensure that adopted approaches are feasible and sustainable. Developing sustainable systems of monitoring requires a concerted approach to integrating systems of data collection and collation and building local capacity dedicated to HIS and NCDs. Lastly, the approaches taken should be assessed and prioritised by their relevance to the region and by the impact that they can have on overall population health. The Pacific is in the midst of an NCD crisis, reaping the greatest impact with the limited resources at hand is essential. Panel 1: Values and principles to strengthen health information systems for non-communicable diseases (NCD) in the Pacific Values Equity – Monitoring strategies should be capable of detecting the social and gender-specific distribution of risk factors, impacts and services. Pacific ownership – Pacific ownership must be central to the choice of strategy and aim for sustainable systems of NCD monitoring and control. Principles Scientific rigour – Strategies to monitor NCDs in the Pacific must be guided by the best available evidence and supported by ongoing research to inform future improvements. Relevance – Strategies adopted to monitor NCDs must take into account the current health information system capacities and reflect the health priorities for the Pacific Island Countries and Territories. Simplicity – Indicators should be easy to collect and easy to understand. Feasibility – Monitoring strategies must take into account the practical and logistical challenges on the ground and be realistic and viable. Sustainability – NCD monitoring will require the collection of comparable data over time. Implemented strategies must, therefore, be adequately supported so that they can be maintained over long periods. Action focused – Indicators should lead to action. Particular focus should be on cost-effective actions which can have a high impact on improving population health. 13 1.3 Strengthening health information systems for non-communicable diseases in the Pacific Health information from PICTs is often incomplete, unreliable or lacking in quality (Finau 1994). Although most Pacific countries have some form of hospital/health service use data system, data quality is often poor, and there are no (or limited) computer-based linkages between data sources. This makes it impossible to effectively link and track patients’ morbidity and mortality as they move through the healthcare system (Ferguson et al. 2011). Due, in part, to out dated public health acts and legislation, existing data systems are focused on capturing data related to communicable diseases, with many countries required to report on infectious, dangerous and notifiable diseases. Substantial improvement and modification is required to strengthen data-gathering mechanisms for NCDs, including vital registration, cause-of-death statistics, population-based surveys and facilityinformation systems (Samb et al. 2010). National health information systems in the Pacific do not give its decision-makers enough information to determine the magnitude of their NCD problem or to address the needs for NCD prevention and control. Even though the case study below is not specifically related to NCDs, it highlights some of the fundamental issues experienced in PICTs. Case study: An example of how effective decisions are hampered by the quality of health statistics (Soakai & Wood 2012): Nauru prior to 2009 A request for the total number of births for Nauru produced four different figures from different sources. Two were from the birth and death registry, one from hospital records and one from the Nauru Bureau of Statistics. This outcome highlighted the following issues: 1. There is clear duplication of services in an already overburdened workforce. 2. Multiple sources of information can lead to inconsistencies which undermine the confidence of decision-makers seeking to use the data. 3. Inconsistencies in the majority of health statistics arise from each stage of the data collection method, analytical methods and reporting methods. 4. Data is often aggregated at a provincial or country level making it less useful for regional planning. 5. There is a lack of skilled staff for data collection and no clear standards are set to guide staff in writing reports. An effective surveillance framework needs to include information on major risk factors, outcomes (morbidity and cause-specific mortality), national-systems-response interventions and health system capacity (Alwan et al. 2010). We use the Health Metrics Network (HMN) Health Information System Framework to help summarise and illustrate where recommendations made by the expert panel apply to the components of a health information system (Figure 1). This HMN framework divides health information systems into three categories (inputs, processes and outputs) and six components (indicators, data sources, data management, information products, dissemination and use, and health information system resources). By conceptualising the needs of a strong health information system, the framework enables countries to effectively evaluate and ultimately improve their existing systems (WHO 2008). 14 Train policy analysts [Section 3.3] Share costs of monitoring to ensure country ownership [Section 3.5] Develop local capacity in public health law and advocacy [Section 3.4] Develop a ‘tool box’ of sample laws, regulations and policies that can be quickly adapted/adopted to needs of jurisdictions [Section 3.3] Coordinate efforts to build capacity to interpret, use and disseminate evidence [Section 4] Health information system resources Dissemination and use Indicators Components of a health information system Information products Data sources Data management Develop a coordinated set of training courses in report writing and packaging of evidence for different audiences [Section 3.3] Prioritise targets and indicators [Section 2.1] Develop upstream indicators [Section 2.3] Provide IT support and training [Section 3.2] Provide training in critical data analysis for civil registration and vital statistics data [Sections 3.3 and 4] Use external coordinating body [Section 4] Figure 1 Strengthening a health information system to monitor and control non-communicable diseases in Pacific Island Countries and Territories Strengthen civil registration and vital statistics and repackaging a mini STEPs survey [Section 2.2] Integrate data sources for upstream indicators into health information system [Section 2.3] Continually review the status of surveys to ensure that the data are used to inform policy [Section 4] 15 1.4 Priority interventions and interventions that work The WHO has worked with PICTs to develop response packages appropriate to a country’s resource base and founded on the WHO and World Economic Forum ‘best buys’ approach to preventing and controlling NCDs (World Economic Forum 2011). The most robust evidence for cost-effective interventions includes tobacco control as outlined in the Framework Convention on tobacco control, reducing population-wide salt consumption, harmful alcohol consumption and physical inactivity, as well as multi-drug treatment of individuals at high risk of heart attack and stroke with cost-effective and readily available drugs (Robinson & Hort 2011). The expert working group identified the following intervention areas as the highest priority. If appropriately applied, they will likely achieve the 25 by 25 goal (Bonita et al. 2013). Tobacco control Smoking rates are on the increase in many Pacific countries (Allen & Clarke 2007; WHO WPRO 2012b). Tobacco control is a highly cost-effective intervention for low- and middleincome countries and can be enforced through a number of mechanisms. These include increasing taxes on tobacco products; enforcing smoke-free workplaces; packaging and labelling of tobacco products with health warnings supported by public education; and banning tobacco advertising, promotion and sponsorship. The paucity of data in the Pacific on smoking and its consequences makes it difficult to assess the real size of the problem, but the range of prevalence rates in tobacco use in PICTs suggests that tobacco control strategies have a proven track record in the region (WHO WPRO 2012a). Reduced consumption of unhealthy diets All countries in the region report prevalence of raised blood pressure in over 20 per cent of the population and adult obesity is thought to be as high as 75 per cent (WHO WPRO 2012a). Food policies to improve diets have been shown to be a viable intervention strategy both in the Pacific and globally (Thow et al. 2010). Evidence on the benefits of reducing salt consumption and the effectiveness of interventions to reduce salt consumption is particularly strong (Bonita et al. 2013). In the Pacific, population-wide approaches to salt reduction through legislation at the national level have been shown to be cost-effective (Neal 2006). Strategies to reduce salt consumption levels include regulating food labelling; reducing salt, sugar and trans-fats content in processed and restaurant food; taxing processed food with high salt, sugar or trans-fats content; and subsidising healthy local produce. Total risk approach The total risk approach provides counselling and treatment with cost-effective and readily available drugs for individuals at high risk of heart attack and stroke. At the very minimum, those who have experienced a heart attack or stroke should be provided with drugs that lower blood pressure and blood lipids and often also anti-thrombotic agents. Providing these drugs in generic fixed-dose combination pills should also reduce costs and improve adherence. If and when resources are available, then similar strategies should be applied to people identified opportunistically as at high risk of cardiovascular disease (>30% over 10 years) based on their age, sex, blood pressure measurements and other self-reported risks. Interventions to reduce the consumption of alcohol and to reduce levels of physical inactivity are also crucial cost-effective approaches to NCD prevention and control and should not be neglected. Here we have simply identified those areas where PICTS should concentrate their efforts for the greatest impact on population health. 16 2. The WHO global monitoring framework and the Pacific 2.1 Data availability As noted, vital registration systems in the Pacific are weak. Although the legislation requiring deaths to be registered may exist in most PICTs, this does not necessarily translate into practice. However, it is likely that more data exist than expected, but most of these data have not been properly collated and therefore not available for analysis (Carter et al. 2012). Annual reports from the Pacific are typically poor quality, but they do present data on health facilities and health service performance and are often the sole outlet for facility-based data (Hodge 2012). Apart from routinely collected data, a series of standardised population-based surveys have been established in the Pacific over the last decade to identify NCD burden and the prevalence of NCD risk factors. For instance, five PICTs have to date been supported by the Secretariat of the Pacific Community (SPC) to conduct local demographic and health surveys which cover a broad range of subjects related to the health and nutritional status of a sample population and can provide valuable information on NCDs. Designed specifically for NCDs, the STEPwise Approach to Risk Factor Surveillance for NCDs (STEPS) is a standardised population-based survey which is usually administered to 25–64 year olds. STEPS assesses three levels of risk factor exposure: risk behaviour, physical measurement and blood samples. The underlying principle of STEPS is to establish a surveillance system that builds local capacity to collect comparable data on core measures of known risk factors. The STEPS survey is modular and designed to be flexible and adaptable to the specific needs and capabilities of different countries. The STEPS survey provides a complete package of tools and guidelines for implementing the survey and for data analysis, as well as comprehensive templates for writing-up reports and fact sheets. STEPS and its coverage in PICTs will be further discussed later in this working paper. The Global Tobacco Surveillance System (GTSS) was initiated in 1999 by the WHO and Centre for Disease Control (CDC) to assist countries to collect data on youth and adult tobacco use. The GTSS is made up of three surveys. The Global Youth Tobacco Survey (GYTS) collects information on adolescent’s knowledge and attitudes towards tobacco. The other two collect data from adults: the Global School Personnel Survey (GSPS) and the Global Health Professionals Survey (GHPS). In 2001, the WHO collaborated with the Joint United Nations Programme on HIV/AIDS (UNAIDS), the United Nations Educational, Scientific and Cultural Organization (UNESCO), and the United Nations Children’s Fund (UNICEF), and with technical assistance from the CDC, to develop the Global Schoolbased Student Health Survey (GSHS). The GSHS survey collects systematic information, using a scientific sample selection process and a self-administered questionnaire, from students on risk behaviours and protective factors. The GSHS is school based and captures students aged 13 to 15 years. Moves are underway to expand this to 17 years. 17 In preparation for the February NCD workshop, we carried out a preliminary literature review to assess the state of NCD monitoring in PICTs. We analysed six main sources of data for 16 countries1 representing country-driven reporting requirements, external reporting requirements, and reports from population-based surveys. Sources examined included: STEPS reports, demographic and health surveillance reports, as well as data that were available from GSPS and GYTS. We also collected results from annual reports and Millenium Development Goal (MDG) reports. Routine health information from ministries of health, NCD surveys run by ministries of health, and STEPS surveys are the usual sources of these data. We compared information in these reports with indicators required for reporting in the WHO GMF. 1 Cook Islands, Commonwealth of the Northern Mariana Islands (CNMI), Fiji, Federated States of Micronesia, Kiribati, Nauru, Niue, Palau, Papua New Guinea (PNG), Tonga, Tuvalu, Tokelau, Samoa, Solomon Islands, Vanuatu 18 Table 1 Pacific Island Countries reporting on non-communicable disease (NCD) indicators Country Indicator Cook Islands CNMI Fiji FSM Kiribati Marshall Islands Nauru Niue Palau PNG Tonga Tuvalu Tokelau Samoa Solomon Islands Vanuatu Outcomes (mortality and morbidity) Cancer incidence by type Premature mortality Risk factors Alcohol consumption Energy intake from saturated fatty acids Consumption of fruit and vegetables Overweight and obesity Physical inactivity Raised blood glucose Raised blood pressure Raised total cholesterol Salt intake 19 Country Indicator Cook Islands CNMI Fiji FSM Kiribati Marshall Islands Nauru Niue Palau PNG Tonga Tuvalu Tokelau Samoa Solomon Islands Vanuatu Current tobacco smoking Current tobacco smoking in adolescents National Health Response Cervical cancer screening Drug therapy for heart attacks and stroke NCD medicines and technology Access to palliative care2 Policies on partially hydrogenated vegetable oils 2 Policies on food marketing2 Vaccination for HPV and HBV 2 Not currently available from standard health information sources but recommendations of how such information might be collected and organised can be found in Section 2.4. HPV – human papillomavirus, HBV – hepatitus B virus 20 Country Indicator Cook Islands CNMI Fiji FSM Kiribati Marshall Islands Nauru Niue Palau PNG Tonga Tuvalu Tokelau Samoa Solomon Islands Vanuatu Other NCD indicators Per cent of primary healthcare services with PEN* Admission rate for NCDs Amputation rate for diabetic sepsis Patients registered at NCD clinics Patients screened for high risk of cardiovascular disease (CVD) NCD healthcare expenditure Adults aged 25+ ever diagnosed with diabetes, hypertension, CVD or rheumatic heart disease Adults aged 25+ ever diagnosed with diabetes or hypertension by wealth 21 Country Indicator Cook Islands CNMI Fiji FSM Kiribati Marshall Islands Nauru Niue Palau PNG Tonga Tuvalu Tokelau Samoa Solomon Islands Vanuatu Per cent of children (<5) who are overweight Routine reporting Annual report *PEN – package of essential non-communicable [disease interventions] Population-based surveys STEPs report Demographic and Health Survey Global School Personnel Survey Global School-based Student Health Survey Millennium Development Goals reporting 22 As demonstrated in Table 1, reports from population-based surveys are the primary data source for indicators relating to behavioural risk factors and most countries had data on these. Cook Islands, Fiji, Kiribati and Samoa were the only countries that regularly report on health outcomes (cancer incidence and cause of death) in their annual reports; however, three-quarters of countries did not have this information. No countries had data on indicators relating to health system response in any of the four sources reviewed. Where data is available, it is often obtainable from more than one data source. For example, the prevalence of adult tobacco smoking is collected by STEPS surveys and often also by demographic and health surveys and by GSPS. This can lead to conflicting values due to different methods and unnecessary duplication of effort. Opportunities to coordinate these surveys need to be seized to ensure coherence and compatibility in definitions and methods and that implementation is as efficient as possible. Although a number of countries had NCD strategic plans, proposed indicators were heavily focused on health system inputs and outputs. As of November 2012, no monitoring or evaluation reports had been developed on implementation of the strategies. Furthermore, there is not much data and capacity to define and track the upstream determinants of these NCD indicators, such as government policies and industry actions, is limited. The extent to which settings that need to be targeted are actually reached by the programs and to which they are able to take the necessary actions should be monitored and reviewed. This will require concerted leadership and systems of accountability. This is not an exhaustive review of the data available from PICTs; however, it is clear from our review that it will take substantial efforts to integrate NCD indicators and monitoring into routine reporting in PICTs. Countries such as Papua New Guinea (PNG), Tuvalu, Commonwealth of the Northern Mariana Islands and Palau have no data available at this time (though PNG’s STEPS report will be published soon) on NCD risk factors. Only four countries out of the 16 presented here have accessible data on mortality by cause and cancer mortality. If available, the data are often very old, and, where STEPS surveys are conducted, the information is often several years old before a report is published. This significantly reduces the usefulness of the evidence for policy purposes (Table 2). 23 Table 2 Year of survey and year of reports for three population surveys in Pacific Island Countries and Territories (2002 2012) Country STEPwise Approach to Risk Factor Surveillance for NCDs Demographic and Health Survey Year of survey Year of survey Year of report Global School-based Student Health Survey Year of report Year of survey FSM (Pohnpei) 2002 2008 - - - Fiji 2002 2002 - - 2005 Marshall Islands 2002 2007 2007 2008 - Samoa 2002 Pending publication 2009 2010 2007 Cook Islands 2004 2011 - - 2008 Nauru 2004 2007 2007 2009 - Tonga 2004 2012 - - 2010 Tokelau 2005 2007 - - - FSM (Chuuk) 2006 2012 - - - Solomon islands 2006 2010 2007 2009 2008 Niue 2011 Pending publication - - - Vanuatu 2011 Pending publication - - 2007 Kiribati 2004–2006 2009 2009 2010 - Papua New Guinea 2007 Pending publication 2006 2009 2007 Tuvalu - - 2007 2009 2005 FSM – Federated States of Micronesia 2.2 Proposed targets and indicators for the Pacific Given the demonstrated difficulty in collecting and presenting timely data in the PICTs, future plans for NCD monitoring and control must recognise the challenges and limitations experienced by these countries. Targets and indicators must therefore be selected based on their feasibility and potential health impact for populations. The targets and indicators of the WHO GMF are categorised into one of the three pillars of the NCD surveillance system: mortality and morbidity outcomes, risk factors (both upstream and downstream) and national systems responses (Figure 2). NCD surveillance system Outcomes: mortality/morbidity 24 Figure 2 The three pillars of non-communicable disease (NCD) surveillance (Source: WHO) In Table 3 we present the 9 proposed targets, the 15 indicators associated with them and the 8 additional indicators. We provide some information on current data sources, data sources that could potentially be pursued and some of the issues and limitations identified associated with the target or indicator. In the first instance, some of the targets and indicators proposed will clearly not be feasible for the Pacific. The infrastructure to collect cancer incidence by type of cancer, for example, simply does not exist in most PICTs. Likewise, the same could be said of the target of ’80 per cent availability of affordable basic technologies and essential medicines to prevent heart attacks and strokes’. Monitoring progress towards an unrealistic target will likely result in wasted time and resources, where there are none to spare. 25 Table 3 Global monitoring framework targets and indicators for the prevention and control of non-communicable diseases Target Mortality and morbidity 1) Reduce premature mortality from NCDs by 25% Indicator Potential data sources Issues and limitations 1. Unconditional probability of dying between ages 30 and 70 years from cardiovascular disease (CVD), cancer, diabetes or chronic respiratory diseases Collected from vital registration systems or sample registration systems using verbal autopsies Top 10 causes of mortality (no ages), absolute number, not using International Classification of Disease codes Many civil registration and vital statistics systems in the region are very weak and need strengthening. 2. Cancer incidence by type of cancer per 100 000 population Collecting cancer prevalence, not disaggregated by cancer type, absolute number Most PICTs do not have adequate cancer registries to collect a reliable estimate of cancer incidence. Risk factors Behavioural risk factors 2) At least 10% relative reduction in overall consumption of alcohol (including hazardous and harmful drinking) 1. Total (recorded and unrecorded) alcohol per capita (15+ years old) consumption within a calendar year in litres of pure alcohol 2. Age-standardised prevalence of heavy episodic drinking among (adolescents and adults) as appropriate, within the national context 3. Alcohol-related morbidity and mortality among adolescents and adults, as appropriate within the national context Government statistics based on national sales, data from alcohol industry, UN statistics, FAO, expert opinion on unrecorded alcohol consumption eSTEPS data 25 to 64 years, amount consumed in past 12 months, number of drinks per day GSHS can be used to collect alcohol consumption for adolescents For example: data from hospital admissions for road traffic accidents could be useful Measurement is difficult. Harmful drinking is often conducted using alcohol that is not obtained legally. Also, alcohol consumption by tourists in some areas may complicate measurements. May need to collect data from the alcohol industry and the conflicting interests may cause problems. 26 Target 3) 10% relative reduction in prevalence of insufficient physical activity 4) 30% reduction in mean population intake of salt with aim of achieving recommended level of less than five grams per day 5) 30% reduction in prevalence of current tobacco smoking Indicator Potential data sources Issues and limitations 1. Age-standardised prevalence of insufficiently active adults aged 18+ years (defined as less than 150 minutes of moderate intensity activity per week or equivalent) eSTEPS data 25 to 64 years, using metabolic energy GSHS can be used to collect physical inactivity for adolescents. The appropriate interventions for Pacific Islands are not clear and have not been adequately considered. 2. Prevalence of insufficiently physically active adolescents defined as less than 60 minutes of moderate to vigorous intensity activity daily 1. Age-standardised mean population intake of salt (sodium chloride) per day in grams in adults aged 18+ years A salt module has been developed and can be added to STEPS. 24-hour urine collection is difficult to achieve. The potential of spot urine specimens should be considered. eSTEPS data 25 to 64 years, absolute number and proportion; considering adding younger age groups to fill gap between STEPS and GYTS GYTS report on 13 to 15 years, absolute number and proportion This target is probably not ambitious enough and instead we should be aiming for the lowest levels currently observed. Self-reported in eSTEPS eSTEPS data 25 to 64 years, absolute number and proportion, raised/diabetes defined as >=6.1 mmol/L can be gathered during alternate rounds of the survey Reporting on prevalence of diabetes – definition of ‘raise blood glucose’ is not included, not agestandardised, mostly absolute numbers, new cases diagnosed at clinics 1. Age-standardised prevalence of current tobacco smoking among persons aged 15+ years 2. Prevalence of current tobacco use among adolescents Biological risk factors 6) Halt the rise in diabetes and obesity 1. Age-standardised prevalence of raised blood glucose/diabetes among adults aged 18+ years (defined as fasting plasma glucose value >= 7.0mmol/L (126mg.dl) or on medication for raised blood glucose) 2. Age-standardised prevalence of overweight and obesity in adults aged 18+ years (defined as body mass index (BMI) greater than 25kg/m for overweight or 30kg/m for obesity) Recommend that the measure be refined as mean fasting plasma glucose. Indicators of diabetes prevalence based upon HbA1c may be easier (but more costly) to obtain especially if done using dried blood spot techniques. 27 Target 7) 25% relative reduction in the prevalence of raised blood pressure or contain the prevalence of raised blood pressure according to national circumstances Indicator 3. Prevalence of overweight and obesity in adolescents (defined according to the WHO Growth Reference: overweight – one standard deviation BMI for age and sex, and obese – two standard deviations BMI for age and sex) Age-standardised prevalence of raised blood pressure among adults aged 18+ years (defined as systolic blood pressure >= 140mmHg and/or diastolic blood pressure >=90mmHg) Potential data sources Issues and limitations School-based health surveys STEPS data 25 to 64 years, absolute number and proportion Current reporting practices: measuring hypertension, not raised blood pressure (not defined), not age standardised, mostly absolute numbers, new cases diagnosed at clinics STEPS data 25 to 64 years, absolute number and proportion, defines high as >=5.2 mmol/l (2002 STEPS) National surveys Feasiblity of blood sampling – may be eased by dried blood spot techniques if these can be validated Additional indicators Cholesterol Age-standardised prevalence of raised total cholesterol among adults aged 18+ years (defined as total cholesterol >=5.0mmol/L or 190mg/dl Fat intake Age-standardised mean proportion of total energy intake from saturated fatty acids and polyunsaturated fatty acids in adults aged 18+ years Fruit and vegetable intake Age-standardised prevalence of adult (aged 18+ years) population consuming less than five total servings (400g) of fruit and vegetables per day National systems responses 8) At least 50% of eligible people receive drug therapy and counselling (including glycaemic control) to prevent heart attacks and strokes Proportion of eligible persons (defined as aged 40 years and over with a 10-year cardiovascular risk greater than or equal to 30% including those with existing CVD) receiving drug therapy and counselling to prevent heart attacks and strokes STEPS data 25 to 64 years, absolute number and proportion per category Treatment module can be added to eSTEPS Will require 24-hour diet recall surveys and food composition databases to get a good estimate. 24hour recall could be added to STEPS but adds a significant amount of time to data collection and detracts from the quick and easy flow of key information. Will require 24-hour diet recall surveys and food composition databases to get a good estimate. Appropriate CVD Risk Charts would need to be made available at clinic settings. Some training in the use of risk charts would be required. Drug regimens would need to be determined. Drugs would need to be accessible and affordable. Are these targets realistic in PICTs? 28 Target 9) 80% availability of affordable basic technologies and essential medicines to prevent heart attacks and strokes Indicator Potential data sources Availability and affordability of generic essential NCD medicine and basic technologies in both public and private facilities WHO/Health Action International surveys on medicine availability and pricing from SARA surveys. Information Management Systems have some data from high- income countries. Issues and limitations Additional indicators Palliative care Access to palliative care assessed by morphine-equivalent consumption of strong opioid analgesics (excluding methadone) per death from cancer Cervical cancer Proportion of women between the ages of 30 and 49 screened for cervical cancer at least once, or more often, and for lower and higher age groups according to programs and policies Trans-fat elimination Adoption of national policies that virtually eliminate partially hydrogenated vegetable oils in the food supply and replace with polyunsaturated fatty acids Marketing foods to children Policies to reduce the impact on children of marketing of foods high in saturated fats, trans-fatty acids, free sugars or salt Vaccination against cancer-causing infections Vaccination against cancer causing infections: human papillomavirus (HPV) and hepatitis B virus FAO GYTS PICTs SARA UN WHO International Narcotics Control Board reports on consumption of narcotics, and WHO reports on estimates of cancer deaths. A screening module could be added to the STEPS instrument. No major issues but not likely to be a priority in PICTs. WHO NCD Country Capacity Survey Trans fat is not required by most food labelling regulations and monitoring strategies are mostly absent. WHO NCD Country Capacity Survey; country reporting back to the World Health Assembly Political will to implement is the key challenge and metrics to better understand and address this issue would be helpful. Recommended indicators have included: number of girls aged 15 in target population who have received three doses of HPV vaccine/total number of 15 year old girls in target population *100 danger of another population survey of a target group – better to measure through number of vaccines given as numerator and population aged 15 as the denominator. Surveys conducted to monitor national immunisation program coverage The validity of self-reported screening in PICTs has not been tested. Food and Agriculture Organization Global Youth Tobacco Survey Pacific Island Countries and Territories Service Availability and Readiness Assessment United Nations World Health Organization 29 2.3 Prioritising targets and indicators Targets agreed upon by member states play a crucial role in driving change and provide clear markers and expectations that can potentially be used to develop systems of accountability. If countries choose to pursue the cost-effective interventions outlined earlier that are likely to provide the greatest impact for Pacific populations, the targets and indicators that are monitored should be selected to reflect local issues and capture the changes expected from their implementation. In this section we outline and prioritise these key targets and indicators for PICTs (Figure 3). This is not to suggest that the rest of the targets and indicators are irrelevant. Rather, that countries should ensure the mechanisms for the prioritised targets and indicators are well established before investing time and resources in the others. A few priority targets stand out above the rest, in order of importance: at the population level, reducing or eliminating tobacco use and reducing population salt consumption to reduce blood pressure are key. At the individual level, treating people who are at high risk of heart attacks and stroke will also have a great health impact. Due to the harm these risks are known to inflict upon populations, the relatively large attributable burden, and the cost-effectiveness of interventions designed to combat them, low- and middle-income countries like the PICTs should begin by concentrating their efforts on these three targets. As resources allow, other targets and indicators should be prioritised accordingly. Mortality and morbidity outcomes Priority 1: Mortality by cause is an essential indicator for NCD monitoring. Although cause-specific mortality may not be very sensitive to changes over time, population-level information on this indicator can be very useful for detecting inequalities between genders, socio-economic and ethnic groups. Comprehensive data on mortality by cause can help track inequalities in the population and help to target services and interventions to help those most in need. Cancer incidence has been proposed as a measure of morbidity outcomes. Ideally, data for this indicator would be obtained from cancer registries that collect and classify all new cases of cancer. Most PICTs, however, do not have functional cancer registries or sophisticated cancer reporting systems (Moore et al. 2008). For most PICTs, setting cancer incidence as an indicator will not be feasible or realistic and therefore is not recommended in the short term. The starting point should be strengthening collection of hospital-based cancer data. Risk factors Priority 2: Getting people to stop smoking should be a priority for PICTs. Even where tobacco does not appear to be the leading cause of death in a country, tobacco is a contributing cause for a large number of diseases. A number of effective interventions exist to prevent the uptake and to promote the cessation of smoking. A focus on tobacco control is likely to save costs and have large health benefits in the long term. In fact, the importance of this risk factor makes the GMF target of ‘30 per cent relative reduction in tobacco use in persons aged 15+ years’ appear insufficiently ambitious. A more ambitious goal for PICTs is a Smokefree Pacific by 2025, where less than five per cent of adults smoke. Two indicators for this target have been agreed upon: 1. the prevalence of tobacco use among adolescents 2. age-standardised prevalence of current tobacco use among persons aged 18+ years. The prevalence of tobacco use must be monitored. The WHO STEPS survey provides a convenient tool to collect the data. Generally, the STEPS survey is given to 25 to 64 year olds. Countries may choose to extend the lower end of this age range to 18, for example, in order to capture the 30 prevalence of tobacco use among a younger cohort. Tobacco use among adolescents can be obtained from school surveys like GSHS. Priority 3: Reducing salt consumption should be the next priority for PICTs. The target set is a ‘30 per cent reduction in mean population intake of salt/sodium’, and moving towards a goal of five grams per day (WHO 2012b). There are tried, tested and cost-effective approaches that can reduce salt consumption at a population level. These preventive strategies cost a fraction of what a country could potentially spend on managing hypertension. This makes salt reduction a high priority for highburden countries (Webster 2009). One indicator has been agreed upon: Age-standardised mean intake of salt (sodium chloride) per day in grams in persons aged 18+ years. Salt consumption can be measured using a risk factor survey such as STEPS. Questions about people’s knowledge, attitudes and behaviours related to salt consumption have been developed and can be easily included. The collection of dietary survey data from a subset will provide additional quantitative insights into salt consumption levels. Biochemical measurements of urine samples in a subset has been done in Samoa and the Cook Islands and is an option for countries considering second-round STEPs surveys. Reducing sugar and trans fats consumption is also crucial, but monitoring strategies, such as 24-hour dietary recall, would be very challenging to implement. Once Pacific countries have established mechanisms for monitoring these high-priority areas, attention should then turn to other important risk factors, namely, a broader reduction in unhealthy diets, physical inactivity, harmful alcohol consumption, raised blood pressure, diabetes and obesity. National systems responses Two targets have been proposed that fall under the national systems responses pillar of the GMF. These are: 1) at least 50 per cent of eligible people receive drug therapy and counselling (including glycaemic control) to prevent heart attacks and strokes, and 2) an 80 per cent availability of the affordable basic technologies and essential medicines, including generics, required to treat major NCDs in both public and private facilities. Priority 4: It is crucial that there is sufficient information so that interventions aimed at preventing and controlling NCDs can be evaluated, and that countries and researchers can learn what works and what does not. The targets and indicators that fall under the national systems responses pillar of the framework do not sufficiently reflect the interventions identified. A comprehensive and effective NCD prevention strategy must use population approaches as well as one that targets individuals at high risk of cardiovascular disease (CVD). This latter approach is clinically oriented and aims to treat those identified by their cardiovascular risk profile. The strength of this approach is that it recognises the multiple causes of CVD and the relationships between risk factors and their effects. The first of the two targets proposed for the national systems responses could be monitored by the addition of a treatment module to the STEPS instrument, similar to that found in the WHO STEPwise approach to stroke surveillance. The latter target, as mentioned in Table 3, will pose a very large challenge for PICTs. It will require opportunistic screening at all visits to a clinic by staff trained to assess overall risk and to refer those at high risk of CVD for treatment. Lastly, targets on the reduction in the consumption of sugar and trans fats have not been included in the GMF, but are potential goals for policy-level interventions. It is critical that Pacific countries over the next years report on the impact of changes made at the policy level and better understand if and how laws and policies are implemented on the ground. To do this, PICTs will need to come to a consensus on which policies need to be monitored, the most suitable upstream factors and indicators to track them. The next section discusses in greater detail what we refer to here as ‘upstream factors’. 31 Highest priority DATA SOURCES CRVS STEPS Mortality due to NCDs Smoking prevalence Salt intake History of heart attack or stroke Drug therapy and counselling GSHS SARA Tobacco use prevalence among adolescents Essential NCD medicines availability Overweight/obesity prevalence in adolescents Hepatitis B vaccine availability Alcohol consumption among adolescents HPV vaccine availability Access to palliative care Cervical cancer screening Alcohol consumption among adults Overweight/obesity prevalence CRVS – civil registration and vital statistics GSHS – Global School-based Student Health Survey HPV – human papillomavirus NCD – non-communicable disease SARA – Service Availability and Responsiveness Assessment Survey STEPS – STEPwise Approach to Risk Factor Surveillance for NCDs Figure 3 Prioritisation of indicators and data sources 2.4 Trade, regulatory mechanisms and non-communicable diseases ‘If the UN High-Level Meeting leads to more concerted effort by international and domestic actors to consider interdependencies, and challenge long-established debates over what is in the national interest, then it can be judged a success’ (Chand 2012) Globally, attention has begun to turn towards the social determinants of NCDs and upstream factors. As shown by the recent subregional workshop ‘Trade and NCDs in the Pacific’, this is also true for the Pacific region. Access to certain foods and products and the trade agreements that provide them are increasingly recognised as driving forces in the NCD epidemic (Moodie et al. 2013; Thow et al. 2010, 2011,). This is particularly true in PICTs, where rapid economic development, urbanisation, and small but growing population sizes make these countries particularly dependent on imported foods. In turn, trade agreements and taxation set food prices that restrict, guide and force people's choices 32 and can eventually lead to malnutrition, as well as obesity and diabetes in the same population (Basu et al. 2013). In the Pacific, agreements with the WHO are related to changes in the population’s dietary habits through many levels of complexity. Regional trade agreements, such as the Pacific Island Country Trade Agreement and the Pacific Agreement on Closer Economic Relations, often relax the very measures that are intended to protect people’s health (Rayner et al. 2006). Countries will have to balance the need for economic development by broadening Pacific markets and trade liberation with the protection of the health of their populations, and do so equitably (Fa’alili-Fidow et al. 2011). It will also be necessary for countries to identify and evaluate the most feasible and effective policies for their context (Snowdon et al. 2010). Capturing the impact of these interventions will be key to ongoing developments in NCD prevention in the region, as well as globally. The WHO GMF includes only two indicators to monitor issues at this level. The first of these falls within the risk factor (or exposures) pillar (Figure 2) and monitors ‘policies to reduce the impact on children of marketing of foods and non-alcoholic beverages high in saturated fats, trans fatty acids, free sugars, or salt’. The second one fits in the national systems responses and monitors the ‘adoption of national policies that limit saturated fatty acids and virtually eliminate partially hydrogenated vegetable oils in the food supply, as appropriate, within the national context and national programmes’. These indicators do adequately assess and monitor the impact of complex upstream factors affecting NCD burden. Innovative indicators are urgently needed to track policies at the national and international level, in addition to the intermediate factors already tracking the progress and implementation of policies on the ground. In the first instance, countries should focus monitoring on a small number of comparable indicators which should reflect the priorities identified for the region. These indicators could include not just the presence of policies and legislation, but the availability of products and where these products are easily accessed and, for equity purposes, by whom. For example, two core registries could be established as follows. A registry of national regulations controlling food supply issues, including information on: o regulations controlling levels of salt, sugar, fat and energy in foods o relevant taxation policies (e.g. fat or sugar taxes) o relevant planning policies (e.g. locations and density of fast-food outlets) o national voluntary codes of practice relating to food supply issues (e.g. the cost of alcohol and harmful foods). A registry of the extent to which mandatory or voluntary initiatives such as these are implemented by those required to take action, be they food manufacturers, food retailers or government departments. These indicators may be obtainable from health impact assessments which are discussed in more detail in the next section. A better understanding of the challenges and opportunities associated with collecting, analysing and interpreting this data will evolve and with this knowledge this area of research can and should expand. There is a ripe opportunity for PICTs to develop innovative approaches to surveillance and lead the world in this emergent area of research. 2.5 Data sources Over the next five years, obtaining health information for NCD monitoring and control in the Pacific should focus on data that can be retrieved from civil registration and vital statistics (CRVS), STEPS and GSHS. Strengthening national civil registration systems, conducting population surveys and improving data collection systems at the primary health care level are essential for sustainable monitoring and evaluation. This will ensure that health data is balanced by being sourced from both population and institutional levels (Figure 4). 33 Figure 4 Population-based and institution-based data sources (Source: HMN 2008) Civil registration and vital statistics Over the last few years, Pacific countries have taken significant strides to strengthen their CRVS systems. Ongoing work devoted to improving CRVS, supported by initiatives like the Pacific Vital Statistics Action Plan, the Brisbane Accord Group (both discussed in more detail in the following section) and the Health Information System Knowledge Hub (HISHub), has a key role in monitoring deaths due to NCDs and must continue to be supported. Training and capacity building are necessary at a number of key levels in a CRVS and these will differ according to country needs. HISHub has worked with PICTs to assess their health information systems and to develop strategies for strengthening them (Mikkeleson 2012). The quality of cause-of-death data and the medical certification of deaths are key areas of concern and therefore the HISHub has been building capacity to analyse cause-of-death data and assess its quality. The HISHub also developed a handbook on how to correctly complete death certificates and has worked closely with clinicians across the Pacific region to develop and improve these often neglected skills. Where medical certification is not possible and CRVS systems are either weak or absent, verbal autopsies are crucial for monitoring causes of deaths in Pacific populations. A verbal autopsy consists of a structured interview between a trained health worker and usually a relative or caretaker of the deceased. It garners information about the signs and symptoms experienced prior to death. This information is then analysed to ascertain the most likely cause of death. The wide application of verbal autopsies is a viable and desirable option for improving the current state of knowledge surrounding patterns of death in the region (Figure 5). Risk factor surveillance Risk factor surveillance provides information on the distribution of risk-factor levels in a population, and changes can be assessed through repeated cross-sectional studies or in panels. Implementation of risk-factor surveillance based on STEPS provides a simple, cost-effective and sustainable tool. STEPS is made up of three ‘steps’: 1. conducting a questionnaire 2. making simple physical measurements 3. collecting blood samples for assessment. At each step, there are three levels of information: core items (mandatory), expanded items (only if relevant) and optional items (added to reflect local circumstances). Extra modules with contextspecific questions can be added. The three steps do not all have to be administered, although for face- to-face interviews, it is advised that both Step 1 (self-reports) and Step 2 (measures of BMI and 34 blood pressure using automated devices) are done at the same time. Step 3 (biochemical measures) add considerably to the cost and complexity of the survey. The flexibility of STEPS means countries are often tempted to use the most expanded version of the survey. This can add substantial cost and time to data collection and may lead to an impression that the survey is too difficult or unsustainable. Instead, a core STEPS survey focusing on the priorities identified for PICTs should be promoted in the first instance. This core STEPS could collect a minimum set of indicators (Step 1 and Step 2) every three to five years. Blood samples (Step 3) and the estimation of salt consumption could be performed every other survey round and/or on a subsample (Figure 5). Most importantly, to be sustainable and effective, STEPS and GSHS surveillance must be institutionalised as part of a HIS and integrated into all health systems in PICTs. This means that countries take ownership of the full framework and that national health systems are held accountable for their completion and reporting. Other surveys Many surveillance systems and surveys are run through agencies in the Pacific, such as the demographic and health surveillance systems mentioned earlier. Research institutions in various countries have developed a number of disease-specific and population-specific surveys. Ongoing health initiatives in the Pacific need to be examined to determine what might be useful for better understanding the NCD situation in each country. However beyond this, countries must also develop national survey plans with support from the WHO and SPC. This will enable coordination of the work in-country to prevent doubling of effort and confusion between results from different sources. It will also ensure that the right information is being collected at the right time using standardised definitions of key variables. These plans should be broadly concerned with all aspects of health and not just NCDs or infectious diseases. The Pacific Public Health Surveillance Network, for example, is the key framework for public health monitoring in the region and focuses on the surveillance of communicable diseases. Where capacity allows, extending the remit of the network to include NCDs could help streamline processes. The WHO in collaboration with the United States Agency for International Development (USAID) developed the Service Availability and Readiness Assessment (SARA) survey methodology to fill gaps in measuring progress in health system strengthening. The SARA survey requires health facility visits where data is collected using key informant interviews and observation of key items. The survey can either be carried out as a sample or a census. The objective of the SARA survey is to generate regular data on service delivery, the availability of key human and infrastructure resources, availability of basic equipment, basic amenities, essential medicines, and diagnostic capacities, and on the readiness of health facilities to provide basic health-care interventions. Clearly there are a number of surveillance and research initiatives that can and do play central roles in NCD monitoring and control. Having said this, surveys are not enough. Countries should not be distracted from developing quality routine data systems because they have successfully implemented surveys. Primary healthcare data Health systems needs to be reoriented to a primary health care approach to effectively respond to the increasing burden of NCDs: this is especially true in resource-limited settings such as the Pacific, where treatment costs at the secondary and tertiary level rapidly escalate (Waqanivalu 2011). The WHO ‘Package of essential non-communicable (PEN) disease interventions for primary health care in low-resource settings’ is a recent initiative aimed at strengthening primary healthcare (WHO 2010). A ‘basket of essential services’ has been designed as part of the package, along with a number of protocols for clinical diagnosis and treatment, and various indicators on risk factors that should be 35 collected at each consultation. These risk factors, which include smoking history, waist circumference, history of diabetes, and others, represent a significant data source for NCD monitoring and control. Linking this information to secondary, tertiary and national-level data systems is important for clinical care, but also for predicting future demand and allocating resources. Better use of such primary healthcare data would also reduce reliance on costly surveys. Primary health facilities, as well as being the first point of contact with the health system, are also the only point of contact for many people living in rural and remote communities. They face long distances to travel to secondary and tertiary care facilities. Furthermore, outreach activities are often coordinated and implemented at the primary care level. Strengthening data collection, analysis and dissemination at the primary level is therefore critical for gaining a better understanding of the burden of disease among isolated communities. It is important to note, however, that such primary data will lack representation from those who do not make it to clinic, resulting in a biased dataset. This is particularly significant in light of concerns around equity and the need to ensure that those who are most in need are identified. NCDs are chronic conditions and represent a significant challenge to health services. As opposed to acute conditions, most NCDs require lifelong interaction with health services, be it for routine checkups or ongoing medication for disease management. The ability to track patients over time and between health facilities is of vital importance for NCD monitoring and control, and is an area severely in need of investment. In PICTs, patient files are mostly kept in hard-copy logbooks or health cards at the primary care facility and there are no processes to link this information to higher levels. In effect, when a patient presents at a secondary clinic or tertiary hospital, they have no recorded history on file. Although a small number of Pacific countries have implemented a system of national patient identifier numbers, these numbers are often only assigned at secondary or tertiary health facilities, and many challenges remain in ensuring patients are not duplicated in the system. Hospital-based disease registers Results from hospital-based disease registers are of limited value for estimating disease burden. Hospital patients do not represent the whole population and are likely to be a biased sample. However, hospital registers can be used as starting points for building capacity for community-based disease surveillance and to expand using more complex data collection when possible (WHO 2012a). Upstream factors Data describing national policies and the practices of key industries influencing NCDs are mostly absent and have not traditionally been part of health information systems. As noted earlier, a registry of data on policies and policy implementation is recommended. An established method for assessing the broader impact of policies across different sectors and settings is to employ health impact assessments (HIAs). HIAs use quantitative and qualitative techniques to synthesise evidence to inform public policy. Bringing together these types of data in PICTs will require coordination and cooperation within and between sectors. Not only different sectors within a country’s government, but also non-governmental organisations collecting data in-country and other international organisations that collate data from sources such as the United Nations Food and Agricultural Organization (Basu et al. 2013). 36 Data source Civil registration and vital statistics Immediate action necessary Training doctors in death certification Widen the use of verbal autopsies Simplify surveys to collect the minimum number of data points STEPS + GSHS Integrate the STEPS and GSHS surveys into routine health information system activity Build analytical capacity and confidence to write reports and disseminate messages Figure 5 High priority actions to improve and strengthen data sources 37 3. Capacity and coordination 3.1 Building capacity for civil registration and vital statistics Mortality by cause is of central importance to understanding NCD epidemiology and changes over time. The Brisbane Accord Group (BAG) developed the ‘Pacific Vital Statistics Action Plan (2011– 2014)’ with the aim to improve vital registration in the region. The group was established in 2010 as an initiative of the HISHub and SPC. BAG has worked with its partners3 to provide continuous strategic and technical support to countries around vital statistics improvements, and deliver a more coordinated response from partner agencies. Employing the WHO Vital Statistics Comprehensive Assessment tool, BAG works closely with countries to assess their collection and reporting systems for births, deaths and causes of death. BAG then assists these countries with the development of a country-specific vital statistics improvement plan. Critical to the success of BAG has been country engagement through the Pacific Statistics Steering Committee and country commitment to report on progress against their country-specific plans to the Pacific Ministers of Health. The Pacific Health Information Network (PHIN) aims to support health outcomes and systems by improving the quality, and strengthening the use of, health information. Outcomes and achievements of the Brisbane Accord Group as of February 2013 Ten countries are engaged in medical certification training with their doctors. Two countries are updating their curriculum for medical students on correct certification practices and procedures. Four countries are implementing policy changes to adopt the WHO International Cause-of-Death Certificate. Six countries are participating in the region’s first Civil Registration and Vital Statistics Short Course. Three countries representatives are completing analytical and reporting writing attachments with SPC for vital statistics data. Two countries are producing a comprehensive vital statistics report. Representatives from the areas of statistics, civil registration and health have attended a number of in-country meetings hosted by members of the Brisbane Accord. Group. 3.2 Generating and managing data A number of initiatives to consolidate data from the numerous surveillance activities ongoing in the Pacific and globally have been developed or are in development. For example, the Pan-America Health Organisation (PAHO) has developed the Virtual Health Library for NCDs and supports countries to strengthen health information systems to monitor NCDs by providing guidance, tools and training. PAHO has prepared a summary of NCD indicators from the Americas. The SPC has also integrated data from countries in the region on all priority communicable and non-communicable diseases on their central database ‘PRISM’. This kind of work can help stimulate inter-country discussions and comparisons, forms a baseline for the future, and helps countries to make a stronger case for aid and support (Hospedales et al. 2012). 3 WHO, UNICEF, Australia Bureau of Statistics, PHIN, Queensland University of Technology, Fiji National University, United Nations Population Fund, University of New South Wales 38 Research institutes have a growing number of data-generating projects in PICTs. The SPC has played a central role in NCD surveillance and operational research, hosting a recent meeting in Noumea (6 to 8 February 2013). The Pacific Research Centre for the Prevention of Obesity and NCDs, for example, is a collaboration between the Fiji School of Medicine and Deakin University and is engaged in field research in the Pacific on NCDs, and the George Institute for Global Health has been supporting salt reduction strategies for the region (Webster 2009). 3.3 Building analytical capacity STEPS has been in operation in the PICTs since 2000, but the process of analysis and producing reports has often suffered extended delays. In part these delays can be explained by the original paper-based format of the survey (the Personal Digital Assistant-based eSTEPS Survey has resulted in much quicker turnaround). Conducting surveys on paper forms adds several steps to the process, including quality checks in the field, transport of forms to an office, data entry and data cleaning. The latter two steps are particularly vulnerable to weak information technology (IT) infrastructure and depend on technical know-how. Often, however, the delays in producing STEPS reports are due to a lack of in-country capacity to prepare such documents. A number of initiatives already exist to help develop the analytical capacities of health information system professionals in PICTs. A STEPS analysis training package is provided by the WHO along with a comprehensive template to facilitate report production. Also available is ANACoD, a toolkit designed by HISHub to help build competencies in the analysis of cause-of-death data. Despite these efforts, there is a noted lack of committed and adequately skilled professionals in most PICTs confident to complete the tasks. Where they do exist, those trained are often individuals tasked with a number of responsibilities in the ministry and not dedicated to any particular project, such as NCDs. Consequently, data is often analysed off site by epidemiologists located outside the country and as such, a country's sense of data ownership is threatened. Workforce development is a ‘multifaceted approach which addresses the range of factors impacting on the ability of the workforce to function with maximum effectiveness’ (Smith 2011). It is more than just the education and training of individual workers: enhancing capacity needs to be broad and comprehensive and have a systems focus. It needs to include government policies and strategies; organisational structures, systems and culture; and knowledge, skills and experience. To meet the increasing demand for information to measure performance against national priorities and policies, there is an urgent need to increase data analysis skills. However, those analysing the data may come from different backgrounds and may require diverse skills to handle a range of data types and analyses. Effectively, the analytical skills required cover the following 10 key areas of health information. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Census Modelling, estimates and projections Population and household surveys Behavioural surveillance Surveillance and response systems Health research Continuous monitoring of births and deaths, with certification of cause of death National health accounts, financial and management information Service-generated data Packaging and dissemination of evidence for policy Furthermore, the Pacific suffers from a severe paucity of human resources skilled in policy analysis and public health law. These skills will be necessary for the translation of evidence to action through knowledge dissemination and advocacy. Courses could be run to build specific skills in this area, 39 similar to those initiatives run for health information systems. For example, the Fiji National University provides a short course in health information systems. It is designed to help professionals from PICTs gain a better understanding of these systems and master the tools, and from that knowledge strengthen the systems in their home countries. Another useful initiative would be to develop a toolbox of sample laws, regulations and policies that can be quickly adapted and/or adopted to the needs of jurisdictions. 3.4 Building institutional capacity Institutional capacity and workforce development are important strategic action points in NCD monitoring and control. This is especially true in the Pacific, as countries are faced with major issues in relation to workforce (training, retention, coverage etc.). However, it is vital to focus on upgrading institutions (rather than people), as people move between roles/organisations and countries. By supporting institutions and the structures that affect performance and outcomes, we can ensure there will be enough skilled workers for the future. The skills and competencies required for a well-performing health information system have not been clearly defined and are not fully appreciated. Limited literature exists on the matter and that which does points to a lack of specialised health information system staff in developing countries. General health workers, who have not been trained in such matters, are often expected to fulfil health information system needs. Related to this, HISHub has recently conducted a study (unpublished) which employed an expert panel to develop a framework of core health information system competencies necessary for general health workers in developing countries. This toolkit will soon be available and can be used to help identify the training needs and professional development programs in different contexts (Whittaker, Mares & Rodney 2013). 3.5 Coordinating efforts A number of organisations and partners are involved in capacity building for NCDs in the Pacific, including PHIN, WHO, SPC, various universities and institutes, as well as government institutions. Due to the absence of any overarching guidance or framework, however, much of the implementation has been fragmented. At a regional level, one of the first actions should be a mapping exercise to outline activities that are underway or planned by countries and organisations. This could be carried out by a regional body, such as PHIN, or a regional governance structure. To ensure a systems approach, it is important that broad health information system skills are developed, rather than taking a narrower focus on NCDs. As such, the strategies proposed in the PHIN ‘Regional Health Information System Strategic Plan (2012-2017)‘ are applicable for NCD capacity building. The strategies include: improving existing pre-service and in-service training for health information system personnel developing regional curriculum for training in health information system, such as (but not limited to) data management, biostatistics, coding, medical record management, and information and communications technology (ICT) reviewing the roles and functions of health information units within ministries of health, such as duties and responsibilities. For these strategies, emphasis should be placed on developing capacity in medical records management, death certification, clinical coding, analysis and interpretation, presentation and dissemination, and how to use information in evidence-based decision-making. These areas are crucial in any response to the NCD epidemic. 40 A significant increase in financial and technical support is necessary for health information systems to fill gaps in the data. Pacific countries have often relied on external funding to cover most of the cost of setting up and implementing surveys and surveillance systems. For these to be sustainable, cost sharing must be encouraged and country ownership of the data as well as the processes involved in surveillance must be developed. Panel 2: Essential areas of capacity building for non-communicable disease surveillance and control To develop skills in data analysis and interpretation by developing toolkits and hands-on training courses. To build confidence in writing and in producing reports and fact sheets for informing policy and for public health advocacy. To develop capacity in the area of public health law and advocacy. To improve country ownership, encourage cost sharing between countries and agencies for monitoring activities. 41 4. Regional governance 4.1 The potential role of a regional non-communicable disease monitoring alliance Over the last decade, the Millennium Development Goals (MDGs) have demonstrated that simple and achievable targets can successfully galvanise the world to respond in a time of need. The MDGs, however, dealt largely with health issues for which, it could be argued; there was relative ease in gaining support. HIV/AIDS and mother and child health are problems that affect younger individuals and their impact on families and society are striking. The burden that NCDs inflict, on the other hand, is more insidious in nature. NCDs are still often perceived to be diseases of the old, the rich or of those who ‘choose’ unhealthy lifestyles. Given this, voluntary targets and indicators are commendable but how are we to ensure that countries are putting in the effort to protect their populations from the NCD epidemic? The WHO GMF is not itself sufficient to provide accountability for this (Beaglehole, Bonita & Horton 2013). PICTs would undoubtedly benefit from a regional governance structure with a remit to include strengthening surveillance efforts and building local capacity for NCD surveillance. This structure could be tasked with helping countries to track progress towards the prioritised GMF targets and should be entrusted by PICTs to uphold a regional accountability framework. Governance requires that actors work together to hold each other accountable. It will be important to agree what it is countries are accountable for, who in those countries is held accountable and what the consequences of failing to uphold those responsibilities are. The approach developed and fostered by the BAG initiative provides an established model of demonstrated effective collaboration between countries and regional actors, such as the WHO, SPC and local universities and research institutions, towards the attainment of a specific set of goals. The BAG first worked closely with Pacific countries to help them conduct self-assessments of their CRVS systems and to develop country-level improvement plans. This allowed partner agencies to focus their support on the needs identified in the plans. This country-led approach recognises the importance of understanding the existing processes and structures in order to ensure real and sustained improvements. A regional NCD alliance, as described in Panel 3, will likely benefit from a similar approach to country engagement, capacity building and a deliberative and strategic coordination of efforts. Panel 3: Recommended roles and functions of a regional alliance for governance Work directly with PICTs and reflect the opinions on the ground in those countries. Encourage all PICT members of the alliance to cost share, that is, to buy into the initiative by helping to fund activities. Assist countries identify gaps and resource needs and help mobilise resources for PICTs for NCDs (e.g. funding, external expertise). Provide a specialised technical resource for PICTs on NCD monitoring which would include the coordination of data sources, assistance in analyses and dissemination of evidence. Help develop a coordinated approach to building in-country capacity in analytical skills and advocacy. Develop resource kits in partnership with countries to help strengthen health information systems. Develop tools to encourage collaboration between sectors and integration of NCD data collection into national information systems. Coordinate training in NCD epidemiology specialising in areas relevant to local needs, such as CRVS and STEPS data analysis and interpretation. Coordinate specialised training in knowledge translation and public health law. 42 Stimulate applied and translational research on NCDs in the Pacific. Provide data management expertise and/or act as a data repository. Crucially, no systems of data collection or processing outside the existing systems in PICTs should be developed. The key would be to strengthen the health information system of countries by guiding investments, building confidence in analysing data and its translation to law and policy, and incorporating a coordinated approach to surveillance and evaluation that best fits each country's needs. Strengthening existing systems, rather than building parallel ones, has the potential to benefit not just NCDs but all aspects of population health and wellbeing. It is important to recognise that NCDs are one of many health concerns in PICTs and efforts to strengthen systems to control NCDs should also aid health systems in general. Data management is also an area that demands immediate attention. Information technology capacity is limited in many PICTs and countries have voiced a need for a data repository for NCD surveillance data. A potential role for an external body like an NCD alliance could be to act as such a repository, housing an accessible database and coordinating the dissemination of analytical tools to help countries produce reports and policy briefs. Furthermore, the governance of harmful products such as alcohol, sugary drinks and food high in salt and trans fats must be strengthened. This may be beyond the powers of ministries of health and even individual countries, particularly smaller countries such as those in the Pacific. Working together, PICTs, along with partners such as the SPC and WHO, can form an alliance to help support actions taken to regulate the industry and trade of harmful products. Tobacco control in wealthy countries represents a great success in public health and these initiatives provide a useful template for other NCD risk factors. Past experience suggests that it is particularly useful to have a small group of devoted people committed to working with the state to restrict access to tobacco products. The alliance could help to develop these working groups and to build their capacity for advocacy. 4.2 Translational research In dealing with NCDs, Pacific countries face very big challenges with often very limited resources. They will have to make a number of difficult decisions about NCD monitoring and control strategies. Evaluation of interventions, policies and programs is critical to inform investments in NCDs and to ensure that strategies and programs are being implemented as intended, and are having the desired impact. Ministries of health also need to know how much it costs to run programs, the incremental costs to monitor them and what aspects of their systems need the most investment. There is very limited cost information by disease type (e.g. communicable versus non-communicable diseases) available from Pacific countries (Rayner et al. 2006). Some key areas of research that need to be pursued to strengthen health information systems in PICTs and to aid in the decisions they need to make are: costing measurement including national surveillance, surveys and ongoing program evaluation to improve budgeting decisions. Countries need to know the incremental costs of monitoring each added indicator. assessing human resources for health information systems, the skill mix available and the identifying capacity-building needs and opportunities determining the impact of measurement and data on policy and program decision-making, and the best ways to report and present data for greatest influence. A governance structure as outlined would be well placed to guide and support this research, identifying in the first instance the priority areas and coordinating the appropriate actions for obtaining the most useful information to guide action. 43 5. Conclusion The WHO Global Monitoring Framework has been designed to provide guidance for countries on how they should best respond to the challenges posed by NCDs. The recommendations outlined in this working paper, however, are intended to help PICTs get the most out of this framework by focusing on the most relevant and cost-effective strategies. Four key recommendations are presented here: Recommendation 1. PICTs should focus on making strong and sustained commitments towards a limited number of realistic targets, rather than 9 voluntary targets and 25 indicators. We have prioritised the targets according to the available scientific evidence on cost-effectiveness of interventions and the feasibility of PICTs to implement such programs. This will ensure the most cost-effective return in health outcomes. To reach the most important goal of a 25 per cent reduction in premature mortality from NCDs, we have identified three priority targets for intervention: i. reduce smoking ii. reduce the consumption of unhealthy diets iii. treat those at high risk of heart attack and stroke. Recommendation 2. Monitoring progress towards the main goal and the three priority targets must be kept as simple as possible and efforts must be integrated into existing health information systems. Continued strengthening of vital registration systems reporting mortality by cause is essential for all health monitoring. Indicators to monitor risk factors and treatments can be collected using GSHS surveys and a modified version of STEPS, which includes modules to measure salt consumption and the coverage of treatments to prevent heart attacks and stroke. These population surveys must also be integrated into health information systems and implemented regularly. A STEPS survey with a minimum number of questions would ideally be implemented at least every five years and biological samples collected on alternate rounds. Recommendation 3. Monitoring should track changes on the international trade, policy and policy implementation levels. The GMF fails to provide strong guidance on monitoring upstream factors. There has been an implicit assumption that NCDs result from lifestyle choices. Trade and market regulations and the exposure to marketing have only recently been recognised as drivers of the global NCD epidemic. Without these indicators, it will be difficult to grasp the full picture of how and where policy interventions do or don’t work. Recommendation 4. Develop a multilateral external governing body empowered to oversee country progress on NCD surveillance efforts and equipped to provide technical support. The GMF lacks a suitable accountability mechanism. Here we recommend that the key to the strategic success of NCD control in the Pacific region is country engagement at every step, the harmonisation of efforts and the clarification of the roles of the many actors already involved. Complementary efforts must be made a priority to ensure that health information is collected and disseminated in a timely fashion so as to allow for appropriate actions to be taken. A crucial caveat, however. Although there is recognised benefit in having a coordinating body that sits regionally, it is essential that actions taken to develop NCD monitoring and surveillance sit within existing country systems of data collection. Strengthening health information systems through strategic- and evidence-based capacity building and enhancing country ownership will ensure sustainable change for PICTs. Likewise, the health information system response to the 44 NCD crisis must also be embedded in broader health system development. The quality of healthcare services and the collection of quality information are inseparable. Countries cannot have one without the other and thus efforts to improve one must be designed to also advance the other. Countries need to provide coordinated actions in NCD prevention and treatment and this will not be possible without quality information to guide plans and decisions. Experts and institutions engaged in health activities and research in the region must prepare to support health ministers to identify their information needs and strengthen their information systems. This will entail fostering collaborations with other sectors and crucially, seeking the support and commitment from the Heads of State. Nonetheless, it is important to have realistic expectations of the impact of measures taken today on the health of populations in the future. What can a Pacific Island Country or Territory expect from all this activity? What will they have to show for it in 2020? The recommendations set out in this working paper have been carefully considered to represent the most pressing issues in the region, to exploit the most rigorous and up-to-date scientific evidence and to reflect what PICTs can do with the available resources. If these recommendations are followed by PICTs, the data and information they generate will undoubtedly place PICTs in a far better position to manage and control NCDs in their populations. By 2020, if countries commit to strengthening their civil registration systems and have succeeded in improving information on mortality by cause, ministries of health will be able to a cost-effectively direct interventions to highrisk populations and vulnerable groups. Better information will be available on risk factor prevalence and upstream factors, such as trade regulation and national policies. This will provide researchers and ministries with a better understanding of what measures work and what actions need to be taken to help keep their populations healthy and limit the burdens experienced from NCDs. 45 References Allen, M & Clarke, D 2007, ‘Reducing tobacco-related harm in the Pacific’, Health Promotion in the Pacific, vol. 14, no. 2, pp. 115–118. Alwan, A, MacLean, D, Riley L, d’Espaignet, E, Mathers, C, Stevens, G & Bettcher, D 2010, ‘Monitoring and surveillance of chronic non-communicable diseases: progress and capacity in high-burden countries’, The Lancet, vol. 376, no. 9755, pp. 1861–1868. Basu, S, Yoffe, P, Hills, N & Lustig, RH 2013, ‘The relationship of sugar to population-level diabetes prevalence: an econometric analysis of repeated cross-sectional data’, PLoS One, vol. 8, no. 2, e57873. Beaglehole, R, Bonita, R & Horton, R 2013, ’Independent global accountability for NCDs’. The Lancet, vol. 381, no. 9867, pp. 602–605. Bonita, R, Magnusson, R, Bovet, P, Zhao, D, Malta, DC, Geneu, R, Suh, I, Thankappan, KR, McKee, M, Hospedales, J, de Courten, M, Capewell, S & Beaglehole, R 2013, ‘Country actions to meet UN commitments on non-communciable diseases: a stepwise approach’, The Lancet,16-25. Carter, KL, Rao, C, Lopez, A & Taylor, R 2012, ‘Mortality and cause of death and analysis systems in seven Pacific island countries’, BMC Public Health, vol. 12, pp. 436–444 Chand, S 2012, Silent Killer, economic opportunity: rethinking non-communicable diseases, Chatham House, London. Fa’alili-Fidow, J 2011, ‘Ensuring economic, health and social well-being for Papua New Guinea through trade’, Asia-Pacific Journal of Public Health, vol. 23, no. 1, pp. 79–85. Ferguson, T, Tulloch-Reid, M, Cunningham-Myrie, C, Davidson-Sadler, T, Copeland, S, Lewis-Fuller, E & Wilks R 2011, ‘Chronic disease in the Caribbean: Strategies to respond to the public health challenge in the region. What can we learn from Jamaica’s experience?’, West Indian Medical Journal, vol. 60, no. 4, pp. 397–411. Finau, SA 1994, ‘National health information systems in the Pacific Islands: In search of a future’, Health Policy and Planning, vol. 9, no. 2, pp. 161–170. Hodge, N 2012, ‘Annual reports in the Pacific: transforming data into information and knowledge’, Pacific Health Dialog, vol. 18, no. 1, pp. 207–214. Hospedales, C, Barcelo, A, Luciani, S, Legetic, B, Ordunez, P Blanco, A 2012, ‘NCD prevention and control in Latin America and the Caribbean. A regional approach to policy and program development’, Global Heart, vol. 7, no. 1, pp. 73–81. Lozano, R, Naghavi, M, Foreman, K, Lim, S, Shibuya, K, Aboyans, V, Abraham, J, Adair, T, Aggarwal, R, Ahn, SY, Alvarado, M, Anderson, HR, Anderson, LM, Andrews, KG, Atkinson, C, Baddour, LM, BarkerCollo, S, Bartels, DH, Bell, ML, Benjamin, EJ, Bennett, D, Bhalla, K, Bikbov, B, Bin, Abdulhak, A, Birbeck, G, Blyth, F, Bolliger, I, Boufous, S, Bucello, C, Burch, M, Burney, P, Carapetis, J, Chen, H, Chou, D, Chugh, SS, Coffeng, LE, Colan, SD, Colquhoun, S, Colson, KE, Condon, J, Connor, MD, Cooper, LT, Corriere, M, Cortinovis, M, de Vaccaro, KC, Couser, W, Cowie, BC, Criqui, MH, Cross, M, Dabhadkar, KC, Dahodwala, N, De Leo, D, Degenhardt, L, Delossantos, A, Denenberg, J, Des Jarlais, DC, Dharmaratne, SD, Dorsey, ER, Driscoll, T, Duber, H, Ebel, B, Erwin, PJ, Espindola, P, Ezzati, M, Feigin, V, Flaxman, AD, Forouzanfar, MH, Fowkes, FG, Franklin, R, Fransen, M, Freeman, MK, Gabriel, SE, Gakidou, E, Gaspari, F, Gillum, RF, Gonzalez-Medina, D, Halasa, YA, Haring, D, Harrison, JE, Havmoeller, R, Hay, RJ, Hoen, B, Hotez, PJ, Hoy, D, Jacobsen, KH, James, SL, Jasrasaria, R, Jayaraman, S, Johns, N, Karthikeyan, G, Kassebaum, N, Keren, A, Khoo, JP, Knowlton, LM, Kobusingye, O, Koranteng, A, Krishnamurthi, R, Lipnick, M, Lipshultz, SE, Ohno, SL, Mabweijano, J, MacIntyre, MF, 46 Mallinger, L, March, L, Marks, GB, Marks, R, Matsumori, A, Matzopoulos, R, Mayosi, BM, McAnulty, JH, McDermott, MM, McGrath, J, Mensah, GA, Merriman, TR, Michaud C, Miller, M, Miller, TR, Mock, C, Mocumbi, AO, Mokdad, AA, Moran, A, Mulholland, K, Nair, MN, Naldi, L, Narayan, KM, Nasseri, K, Norman, P, O'Donnell, M, Omer, SB, Ortblad, K, Osborne, R, Ozgediz, D, Pahari, B, Pandian, JD, Rivero, AP, Padilla, RP, Perez-Ruiz, F, Perico, N, Phillips, D, Pierce, K, Pope, CA 3rd, Porrini, E, Pourmalek, F, Raju, M, Ranganathan, D, Rehm, JT, Rein, DB, Remuzzi, G, Rivara, FP, Roberts, T, De León, FR, Rosenfeld, LC, Rushton, L, Sacco, RL, Salomon, JA, Sampson, U, Sanman, E, Schwebel, DC, Segui-Gomez, M, Shepard, DS, Singh, D, Singleton, J, Sliwa, K, Smith, E, Steer, A, Taylor, JA, Thomas, B, Tleyjeh, IM, Towbin, JA, Truelsen, T, Undurraga, EA, Venketasubramanian, N, Vijayakumar, L, Vos,T, Wagner, GR, Wang, M, Wang, W, Watt, K, Weinstock, MA, Weintraub, R, Wilkinson, JD, Woolf, AD, Wulf, S, Yeh, PH, Yip, P, Zabetian, A, Zheng, ZJ, Lopez, AD, Murray, CJ, AlMazroa, MA & Memish, ZA 2012, ‘Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010’, The Lancet, vol. 380, pp. 2095–128. Mikkeleson, L 2012, ‘Improving civil registration and vital statistics systems: lessons learnt from the application of health information tools in Asia and the Pacific’, HISHub Working Paper Number 24, School of Population Health, The University of Queensland. Moodie, R, Stuckler, D, Monteiro, C, Sheron, N, Neal, B, Thamarangsi, T, Lincoln, P & Casswell, S 2013, ‘Profits and pandemics: prevention of harmful effects of tobacco, alcohol and ultra-processed food and drink industries’, The Lancet 39-48. Moore, MA, Shin, HR, Curado, MP & Sobue, T 2008, ‘Establishment of an Asian Cancer Registry Network - problems and perspectives’, Asian Pacific Journal of Cancer Prevention, vol. 9, no. 4, pp. 815–832. Neal, B 2006, ‘The effectiveness and costs of population interventions to reduce salt consumption’, background paper to the WHO Forum and Technical meeting ‘Reducing salt intake in populations’, 5–7 October 2006, Paris, France. Pacific Food Security Framework 2013, viewed 28 May 2013, <http://www.foodsecurepacific.org>. Pacific Vital Statistics Action Plan (2011–2014) 2013, viewed 16 January 2013, <http://www.uq.edu.au/hishub/docs/VITAL-STATS-OUTLINE-FINAL.pdf>. Rayner, G, Hawkes, C, Lang, T & Bello W 2006, ‘ Trade liberalization and the diet transition: a public health response’, Health Promotion International, vol. 21, suppl. 1, pp. 67–74. Robinson, H & Hort, K 2011, Non-communicable diseases and health systems reform in low- and middle-income countries, The Nossal Institute for Global Health: The University of Melbourne, Australia. Samb, B, Desai, N, Nishtar, S, Mendis, S, Bekedam, H, Wright, A, Hsu, J, Martiniuk, A, Celletti, F, Patel, K, Adshead, F, McKee, M, Evans, T, Alwan, A & Etienne, C 2010, Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries’, The Lancet, vol. 376, no. 9754, pp. 1785–1797. Smith, N 2011, Working in Health Promoting Ways: Newsletter number three. Department of Health and Human Services Tasmania. Snowdon, W, Lawrence, M, Schultz, J, Vivili, P & Swinburn, B 2010, ‘Evidence-informed process to identify policies that will promote a healthy food environment in the Pacific’, Public Health Nutr., vol. 13, no. 6, pp. 886–892. Soakai, TS & Wood, M 2012, ‘Improving HIS for better health policy and planning’, Pacific Health Dialog, vol. 18, pp. 161–163. 47 The World Bank 2012, The economic costs of non-communicable diseases in the Pacific Islands: A rapid stocktake of the situation in Samoa, Tonga and Vanuatu. Final report, November 2012. Thow, AM, Heywood, P, Schultz, J, Quested, C, Jan, S & Colagiuri, S 2011, ‘Trade and the nutrition transition: strengthening policy for health in the Pacific’, Ecology of Food and Nutrition, vol. 50, pp. 18–42. Thow, AM, Jan, S, Leeder, S & Swinburn, B 2010, ‘The effect of fiscal policy on diet, obesity and chronic disease: a systematic review’, Bulletin of the World Health Organization, vol. 88, pp. 609– 614. Waqanivalu T 2011, ‘NCD prevention and control through primary care in PICs’, (unpublished paper). Webster, J 2009, ‘Salt reduction in the Western Pacific region: strategies for action’ (draft report), The George Institute for international Health, Sydney. Whittaker, M, Mares, RE & Rodney, A 2013, ‘Mapping health information system competencies for health workers in low- and middle-income countries’, Health Information Systems Knowledge Hub, School of Population Health, University of Queensland (unpublished working paper). WHO see World Health Organization World Economic Forum 2011, From burden to "best buys": reducing the economic impact of noncommunicable diseases in low- and middle-income countries, World Economic Forum, Geneva. World Health Organization 2002, The world health report 2002: Reducing risks to health, promoting healthy life, WHO, Geneva. ——2008, Framework and standards for country health information systems, 2008 Health Metrics Network, 2nd edn, WHO, Geneva. ——2009, Western Pacific regional action plan for the prevention and control of non-communicable diseases (2014-2020), WHO, Geneva. ——2010, Package of essential non communicable (PEN) disease interventions for primary health care in low-resource settings, WHO, Geneva. ——2012a, A comprehensive global monitoring framework including indicators and a set of voluntary global targets for the prevention and control of noncommunicable diseases, Second WHO Discussion Paper, WHO, Geneva. ——2012b, Guideline: Sodium intake for adults and children, WHO, Geneva. WHO WPRO see World Health Organization Western Pacific Region World Health Organization Western Pacific Region 2011, Ninth Meeting of Ministers of Health for the Pacific Island Countries, Information Bulletin No.1, 12 May 2011, viewed 6 January 2013, <http://www2.wpro.who.int/internet/resources.ashx/PIC/2011/IB1.pdf>. ——2012a, Non-communicable diseases in the Western Pacific Region: A profile, WHO, Geneva. ——2012b, Tobacco Free Initiative viewed 12 March 2012, <http://www.wpro.who.int/tobacco/en/index.html>. 48