does nbi bipolar turbt improve detection rate after wl turb?

DOES NBI BIPOLAR TURBT IMPROVE DETECTION RATE AFTER WL
TURB? PRELIMINARY EXPERIENCE IN A SINGLE CENTRE .
Roberto Giulianelli, Luca Albanesi, Francesco Attisani, Barbara Cristina
Gentile, Luca Mavilla, Gabriella Mirabile, Francesco Pisanti, Daniele
Baldoni , Francesca Pallante , Giorgio Vass elli , Manlio Schettini.
RUA - Roman Urological Association
Division of Urology - Nuova Villa Claudia - Rome - Italy
Statistical Centre – Rome - Italy
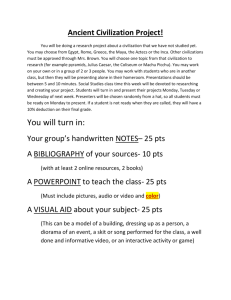
INTRODUCTION
TURBt is the standard initial therapy for superficial bladder neoplasms, but the high percentage of recurrence after surgery remains an unresolved problem. Recent studies suggested that the first TURBt may be incomplete in a significant number of cases. Up to 70% of patients with NMIBC will develop a recurrence after the TURBT. The aim of this study was to evaluate, after a
WL TURBt, the efficacy of identifying persistent bladder cancer on margins and bed of resection by comparing the predictive power of the white light visible lesions versus NBI .
MATERIALS AND METHODS
From June 2010 to April 2012, 797 consecutive patients, 423 male and 374 female, affected by primitives or recurrences or suspicious non-muscle invasive bladder tumours, underwent WL plus NBI cystoscopy following a WL
Bipolar Gyrus PK TURBT. The average follow-up was at 24 (16-38) months.
Indication of suitability for TURBt was provided on the basis of the EAU
Guideline 2010. All patients provided written informed consent prior to the study. All procedures were carried out initially by performing a cystoscopy with white light. The characterization of the sites, including the number, size and appearance of the neoplasms, were recorded on a topographic bladder map. Then a NBI cystoscopy was carried out to confirm what had been seen in the white light examination, and to report suspicious areas with NBI light.
These data, too, were recorded on the topographic bladder map. All endoscopic resections performed with a Gyrus PK scalpel, bipolar generator
(Olympus, Tokyo, Japan). Resection of each lesion was carried out with white light, whilst a resection of surgical margins was performed along with the bed of surgical resection using only NBI light. Istological specimens sent separately with a sequenced number identifying them.
All histopathological evaluations were performed by a single pathologist based on the 2004 WHO classification
RESULTS
A total of 797 patients were enrolled in this study. In our experience we observed an overall suspicious bladder lesions detection rate by 1572 bladder lesions. Of those, following WLTURBt, bladder neoplasms were 1051
(66,85%) thus 521 were negative (33,14%). Histological findings are shown in Table 1 below
Tab 1
PRIMITIVE RECURRENCE UNIFOCAL MULTIFOCAL < 3CM > 3 CM pTa pts (%) pT1 pts (%) pCIS pts (%) pT2 pts(%)
NO TUMOUR
(%)
PUNMPL (%)
LG (%)
HG (%)
NO TUMOUR
(%)
436 (63.93) 246 (36.07) 154 (22.58) 528 (77.42) 203 (29.77) 479 (70.23)
166 (66.40) 84 (33.60) 67 (26.80) 183 (73.20) 79 (31.60) 171 (68.40)
23 (76.67)
0
0
7 (23.33)
0
0
10 (33.33)
0
0
20 (66.67)
0
0
22 (73.33)
0
0
8 (26.67)
0
0
74 (83.15) 15 (16.85) 70 (78.65) 19 (21.35) 88 (98.88) 1 (1.12)
271 (57.58) 198 (42.22) 139 (29.64) 330 (70.36) 173 (36.89) 295 (63.11)
354 (71.81) 139 (28.19) 92 (18.66) 401 (81.34) 131 (26.57) 362 (73.43)
0 0 0 0 0 0
All the WL TURBt patients underwent another resection of the margins and the bed this time using NBI device. We found 521 persistent neoplasms
(33,1%). Tables 2, 3 and 4 show our results
Tab 2
NBI positive margins following TURBT
WL cisto pos
NBI cisto neg pTa pts (%) pT1 pts (%)
0
0 pCIS pts (%) 0 pT2 o oltre pts (%) 0
NO TUMOUR pts (%) 0
PUNPML pts (%)
LG pts (%)
0
0
HG pts (%) 0
NO TUMOUR pts (%) 0
UNIFOC pts (%)
MULTIFOC pts (%)
0
0
WL cisto pos
NBI cisto pos
261 (72,91)
35 (9,78)
54 (15,08)
1 (0,28)
7 (1,96)
174 (48,60)
176 (49,16)
1 (0,28)
23 (6,42)
335 (93,58)
WL cisto neg
NBI cisto pos
39 (47,56)
13 (15,85)
18 (21,85)
0
12 (14,63)
39 (47,56)
31 (37,80)
0
69 (73,17)
22 (26,83)
< 3 cm pts (%)
> 3 cm pts (%)
Primitive pts (%) 0
Recurrence pts (%) 0 total 0
0
0
Tab 3
NBI positive bed following TURBT pTa pts (%) pT1 pts (%) pCIS pts (%) pT2 o oltre pts (%)
WL cisto pos
NBI cisto neg
1(100)
NO TUMOUR pts (%)
PUNPML pts (%)
LG pts (%) 1(100)
HG pts (%)
NO TUMOUR pts (%)
UNIFOC pts (%) 1(100)
MULTIFOC pts (%)
< 3 cm pts (%)
> 3 cm pts (%)
Primitive pts (%)
1(100)
1(100)
Recurrence pts (%)
1
Tab 4
NBI positive margins
+ bed following
TURBT pTa pts (%) pT1 pts (%)
WL cisto pos
NBI cisto neg
0
0 pCIS pts (%) pT2 o oltre pts (%)
0
NO TUMOUR pts (%) 0
PUNPML pts (%)
LG pts (%)
0
0
HG pts (%) 0
NO TUMOUR pts (%) 0
UNIFOC pts (%) 0
61 (17,04)
297 (82,96)
247 (68,99)
111 (31,01)
358
WL cisto pos
NBI cisto pos
51 (27,13)
71(37,77)
0
16 (8,51)
50 (26,70)
0
31 (16,49)
107 (56,91)
50 (26,70)
18 (9,57)
170(90,43)
79(42,02)
109(57,98)
95(50,53)
93(49,47)
188
WL cisto pos
NBI cisto pos
46 (55,42)
34 (40,96)
2 (2,41)
1 (1,20)
0
18 (21,69)
64 (77,11)
1 (1,20)
3 (3,61)
68 (82,93)
14 (17,07)
51 (62,20)
31 (37,80)
82
WL cisto neg
NBI cisto pos
26(45,61)
21 (36,84)
2 (3,51)
7(12,28)
0
1 (1,75)
28 (49,12)
28 (49,12)
0
46(80,70)
11(19,30)
49(85,96)
8(14,04)
36(63,169
21(36,84)
57
WL cisto neg
NBI cisto pos
20 (46,51)
14 (32,56 )
4 (9,30)
0
5 (11,63)
15 (34,88)
23 (53,49)
0
35 (81,40)
MULTIFOC pts (%)
< 3 cm pts (%)
> 3 cm pts (%)
Primitive pts (%) 0
Recurrence pts (%) 0
0
0
0
80 (96,39)
12 (14,46)
71 (85,54)
55 (66,27)
28 (33,73)
8 (18,60)
36 (83,72)
7 (16,28)
27 (62,79)
16 (37,21)
Using NBI light after WL TURBt we identified 23 MIBC (4,41%): 7 of these neoplasms (1,31%) showed a negative WL but positive NBI cistoscopy
Statistical analysis showed in Table 5
Parametro DF Stima Errore standard
Chiquadro
Wald
Pr >
ChiQuadr
STATUS primitive 1
FOCALITY multifocal 1 fumatore_1 no pT1 no
CIS pTaLG pTaHG no no no
1
1
1
1
1
Using NBI after WL TURBt gave us the chance to identify patients affected by bladder primitive malignant lesions 80% more than those with recurrence lesions, by multifocal neoplasm 7 times more than those with unifocal, by < 3 cm tumour 3 times more than those with > 3 cm. Moreover
NBI device identify 8 times more CisHG and more than 3 times a pTaLG area invisible using WL TURBt.
DISCUSSION
NBI after WL TURBt enhances the possibilities to find persistent lesions in more than 30% of the cases: 440 (84,45%) positive border lesions, 126
(24,18%) positive bed lesions and 126 (24,18%) positive border and bed lesions together. Statistical analysis showed that NBI enhance significantly the possibilities to identify invisible WL lesions such as multifocal (p<0001), pCisHG (p<0001), primitive, < 3 cm (p<.0266) tumours.
.
Finally using NBI light after WL TURBt we identified 23 MIBC (4,41%): 7 of these neoplasms (1,31%) showed a negative WL but positive NBI cistoscopy.