Pathology Chapter 14 up to page 665
advertisement

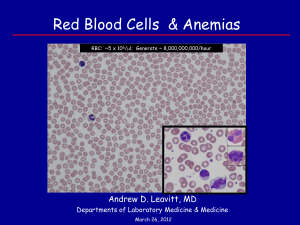
Pathology Chapter 14: Red Blood Cell and Bleeding Disorders (up to page 665) Anemia- decreased amount of RBCs in blood - - - - Anemia decreases the oxygen-carrying capacity of the blood, causing tissue hypoxia Page 640 Anemia is usually diagnosed by a reduction in the hematocrit (RBCs / blood volume) and the Hgb concentration o Both reflect the RBCs unless there’s fluid retention or dehydration in the plasma Other clues for anemia: o RBC size – normocytic, microcytic, or macrocytic o How much Hgb there is- can tell by the color; normochromic or hypochromic o Shape Usually, microcytic hypochromic anemias are caused by disorders of Hgb making o Usually iron deficiency Usually, macrocytic anemias are caused by problems with maturation of RBCs in bone marrow CBC tests used: o Mean Cell Volume (MCV) – average volume of RBCs o Mean Cell Hgb (MCH)- amount of Hgb per RBC o Mean Cell Hgb Concentration (MCHC)- average [Hgb] in a given volume of RBC o Red Cell Distribution Width (RCDW) o Page 641 Symptoms of anemia are: o Paleness o Weakness o Dyspnea on exertion from less oxygen in the blood o Hypoxia can cause fatty change in the liver, heart, and kidney Fatty change of the heart can cause heart failure The heart hypoxia will show up as angina pectoris o Acute blood loss and shock can lead to oliguria(decreased urine) or anuria(no urine) from kidney hypoperfusion o CNS hypoxia can cause headache, dimness of vision, and faintness Blood loss anemia: - Acute blood loss anemia o It’s effects are due to loss of intravascular volume, which if severe enough, can cause shock and death o The decreased oxygenation will trigger erythropoietin from the kidney, which will stimulate the proliferation of CFU-E progenitors in the bone marrow Takes about 5 days for these progeny to matures into released RBCs They’re released as reticulocytes o If there’s bleeding into the tissues, iron is recaptured o - If there’s blood loss, iron’s lost, and can cause iron deficiency, which will limit making more RBCs o If bleeding is enough to decrease blood pressure, adrenergic hormones will cause leukocytosis (increased WBCs) o As the bone marrow is told to release more and more RBCs, more reticulocytes enter circulation Reticulocytes are larger than normal RBCs (macrocytic) o Early recovery from the blood loss will be accompanied by thrombocytosis (↑ platelets) Chronic blood loss will cause anemia if the rate of loss is more than what the marrow can keep up with, or when they run out of iron Hemolytic anemia - caused by breakdown of RBCs - - - - Common features: o Premature destruction of RBCs and a shortened RBC life span o Increased erythropoietin levels causing erythropoiesis o Accumulation of Hgb degradation products RBCs are broken down in phagocytes, especially in the spleen, liver, and bone marrow Extravascular hemolysis – premature destruction of RBCs in phagocytes because the RBC is less deformible o Can lead to hyperplasia of phagocytes, causing splenomegaly RBCs need to be flexible in shape to navigate the spleen sinusoids If they’re not, they lyse, and macrophage clean them up o Main symptoms of extravascular hemolysis are anemia, splenomegaly, and jaundice o Splenectomy can help fix the symptoms Intravascular hemolysis will show anemia, hemoglobinemia, hemoglobinuria, hemosiderinuria, and jaundice o Intravascular hemolysis is more rare, and caused by insults from mechanical injury, complement, toxins, and pathogens o The large amount of free Hgb released from the RBCs are bound by haptoglobin, and the complex gets cleared by phagocytes o As this complex gets depleted, more and more free Hgb oxidizes into a brown colored methemoglobin o The kidneys try to recapture as much Hgb as possible, but some gets into the urine, making it red-brown o Iron can accumulate in the kidneys causing kidney hemosiderosis o All the Hgb breakdown leads to jaundice All hemolytic anemias will cause erythropoiesis, showing a lot of normoblast precursors Kinds of hemolytic anemias: - Hereditary spherocytosis (HS) o - Hereditary spherocytosis is caused by a problem in the structure of the RBC, making it sphere shaped, less flexible, and easily broken o The RBC membrane skeleton has spectrin proteins that give it its flexibility The mutation of hereditary spherocytosis affects spectrin binding in the membrane, taking away its flexibility o Being heterozygous for 2 bad alleles makes hereditary spherocytosis more severe o Young hereditary spherocytosis RBCs are normal in shape, but as they age, the membrane protein is missing, so there’s loss of membrane fragments, forcing the cell into a sphere shape o Removing the spleen helps stop the symptoms from too much RBC destruction that were causing anemia o The main symptoms of hereditary spherocytosis are anemia, splenomegaly, and jaundice Will also see normal things of other anemias, like reticulocytosis and hemosiderosis The spleen will be enlarged due to more phagocytes needed to clean up all the lysed RBCs o In most patients with hereditary spherocytosis, the RBCs will lyse in hypotonic solutions o The RBCs of hereditary spherocytosis will have an increased MCHC, due to dehydration of the RBC from losing potassium and water o Parvovirus, which infect and kill RBC progenitors, can make the anemia worse and cause aplastic crisis Glucose-6-phosphate dehydrogenase deficiency o Without enzymes from the hexose monophosphate shunt or glutathione metabolism, RBCs can’t protect themselves from oxidative injuries, which can lead to hemolysis o The most important of these enzymes is glucose-6-phosphate dehydrogenase G6PD reduces NADP to NADPH when it oxidizes glucose-6-phosphate That NADPH then helps convert oxidized glutathione into reduced glutathione Reduced glutathione protects from oxidative injury o G6PD deficiency is a recessive X-linked trait, which means males are more at risk Most cases are harmless The two to worry about are G6PD- and G6PD Mediterranean o G6PD deficiency causes misfolding of the enzyme, making it prone to destruction RBCs don’t have organelles to make any new proteins, so no more enzyme o Anything that causes oxidative stress can lead to episodes of hemolysis in G6PD deficiency Usually infections, which require free radicals from WBC to fight it off Many drugs can trigger oxidative stress too The most common food causing oxidative stress is fava bean The oxidative stress can cause both intravascular or extravascular hemolysis Exposure to oxidants denature membrane proteins, forming Heinz bodies, which are dark inclusions seen in the RBC - The Heinz bodies can damage the membrane and cause intravascular hemolysis Macrophage can take the Heinz bodies out of the membrane, leaving the RBC deformed The deformed cells easily rupture, and accumulate in the spleen for phagocytes o Episodes of acute hemolysis and G6PD deficiency are self-limited, since it will stop when younger cells with G6PD are all that’s left Sickle cell disease o Sickle cell disease is a common hereditary hemoglobinopathy that’s common in people in Africa o Hgb has 2 globin chains, each with a heme o Normal adults have α2β2 HbA, with small amounts of HbA2 α2δ2 and fetal HgF α2y2 o Sickle cell disease is a mutation in the β globin where valine replaces glutamate o 8-10% of African Americans are heterozygous for sickle cell, called sickle cell trait, which is mostly asymptomatic Helps with malaria o Homozygotes have sickle cell disease, where almost all their Hgb is is HbS o HbS RBCs change into the sickle shape when there’s a decrease in oxygen Long, needle-like shape So sickle cell happens in conditions like chronic hemolysis, occlusions or tissue damage o Factors that affect sickling: Presence of other types of Hgb In sickle cell trait, there’s still a lot of HbA, which prevents sickling unless hypoxia is really bad o HbF prevents it even more than HbA o HbSC disease – when there’s lots of HbC around with sickle cell trait, you get a milder form of sickle cell disease Mean cell Hgb concentration (MCHC) Higher the [HbS]more sickling Ex: intracellular dehydration Intracellular pH ↓pH will increase the protons, which decreases the affinity of Hgb for oxygen, which deoxygenates the HbS, causing sickling Time RBCs spend in certain areas Occlusion causes most sickling Usually, transit times are too short for enough piling up of deoxygenated HbS to occur Transit times are slow in the spleen and bone marrow Transit will slow through areas of inflammation o Every time a RBC sickles, it gets more and more dehydrated and more sickled o o o - How severe the hemolysis is depends on how many irreversibly sickled RBCs there are Sickled cells are fragile, and phagocytes come get them when they rupture Sickle cells also express more adhesion molecules than normal, making them sticky Inflammation upregulates adhesion molecules, which the sickle cells can stick to, causing occlusion, causing more hypoxia, causing more sickling, etc. o The bone marrow will be hyperplastic in sickle cell due to all the lost RBCs o At first spleen will enlarge in sickle cell, but eventually it will fail from infarct and atrophy, a process called autosplenectomy o Sickle cell disease causes hemolytic anemia with reticulocytosis, hyperbilirubinemia, and the presence of irreversibly sickled cells o Sickle cell can cause many kinds of crisis: Vaso-occlusive (aka pain) crisis- infarct causes hypoxia causing pain in that region It’s the most common crisis, and often happens in bone in children Acute chest syndrome happens in occlusion of the lungs, causing chest pain, and can be triggered by a pulmonary infection Sequestration crisis- spleen accumulates sickle RBCs and enlarges, decreasing blood volume, which can lead to shock Aplastic crisis – infection of RBC progenitors gets rid of the supply of RBCs, worsening the anemia o People with sickle cell will also be more prone to infection, due to their spleen being busy with all the RBCs o Treat sickle cell with an inhibitor of DNA making, like hydroxyurea, which can increase HbF, and act as an anti-inflammatory by inhibiting WBC making Thalassemias - disorders caused by mutations to making HbA o β-thalassemia is caused by deficiency in making the β globin, while α-thalassemias are caused by a deficiency in making the α chain Problems are from both the missing chain, and excess of the other chain Heterozygotes also seem to help with malaria o β-thalassemia Can either be a β0 mutation with no β globin, or a β+ mutation with not enough β chain Splice mutations are the most common cause of β+ thalassemia o Creates a new splice site in the intron, but the normal part remains, so some β-globin is still made Chain terminator mutations are the most common cause of β⁰ thalassemia Two ways impaired β globin synthesis can cause anemia: The deficit in HbA making causes hypochromic, microcytic RBCs that can’t carry as much oxygen o Also, α chains without a paired β chain precipitate, causing membrane damage, leading to apoptosis o Those that don’t die are still fragile and lyse easily Because of the continual stimulation for erythropoietin to get more RBCs out there to carry oxygen, the bone marrow makes tons of RBC precursors, which impairs bone growth and causes skeletal deformities Also, since erythropoiesis isn’t working right, hepcidin is suppressed and therefore can’t inhibit iron absorption, so tons of iron is absorbed People with any two of the mutated β alleles will have the more severe form of β-thalassemia called β-thalassemia major Heterozygotes with one normal β allele will have milder β-thalassemia minor aka β-thalassemia trait The thalassemias manifest 6-9 months after birth, when HbF switches to HbA β-thalassemia RBCs look microcytic and hypochromic Often may see “target cells” with the Hgb clustered in the middle Will see a “crew-cut “ appearance of face bones on x ray due to expansion of bone marrow eroding existing bone Spleen will be enlarged in β-thalassemia There will poorly hemoglobinized nucleated RBC precursors called normoblasts in the blood from “stress” erythropoiesis There can be hematopoiesis outside the bone marrow, usually in the liver or lymph nodes Almost all patients have hemosiderosis and secondary hemochromatosis, which are symptoms of iron overload In β-thalassemia major, growth is stunted and anemia will cause death at an early age β-thalassemia minor is usually asymptomatic with mild anemia if any β- thalassemia minor is more common α-thalassemias There’s normally four α chains, and how severe the thalassemia is depends on how many chains are missing Silent carrier state- one α chain is missing, asymptomatic α-thalassemia trait- two α chains are deleted o can happen from one normal parent and one parent with no α chains, or from two parents who each are in a silent carrier state o More likely a child will get it if one of the parents has no chains o α-thalassemia trait is similar to β-thalassemia trait, with small RBCs, little to no anemia, and no physical symptoms Hgb H disease- three α chains are deleted o Most common in Asians o - Since there’s barely any α chains, you get bundles of β chains called HbH o HbH has a huge affinity for oxygen, so it can’t deliver the oxygen well cause it won’t let go of it o HbH is also prone to oxidation, causing it to precipitate and occlude o Symptoms are moderate anemia similar to β-thalassemia intermedia Hydrops fetalis- no α chains are present, most severe o Excess y chains will then cluster in the fetus to form Hgb Barts, which have such a high affinity for oxygen that almost none is delivered to the tissues o Fetus will show pallor, edema, and hepatosplenomegaly, and is usually lethal in utero Page 652 The anemia in α-thalassemias is caused by a lack of Hgb, and the effects of excess unpaired chains that aren’t α chains In newborns with α-thalassemias, excess unpaired y chains form Hgb Barts In adults with α-thalassemias, excess unpaired β chains cause HbH β and y chains are more soluble and stable than α chains, so excess of them causes less severe hemolysis and erythropoiesis problems than the β thalassemias do Paroxysmal nocturnal hemoglobinuria o Caused by mutations to the enzyme PIGA, which is needed to make some cell surface proteins o Normally, proteins are anchored to the plasma membrane either by transmembrane proteins, or by glycophospholipidinositol (GPI) o In paroxysmal nocturnal hemoglobinuria, the GPI-linked proteins are deficient due to the mutation to the PIGA enzyme o The mutation happens in hemopoietic stem cells, so every blood cell from that stem cell has the mutation o The 3 proteins that are then deficient are proteins that regulate complement, called decay-accelerating factor, membrane inhibitor of reactive lysis, and C8 binding protein o RBCs missing these proteins are prone to lysis or injury from complement, causing intravascular hemolysis from the MAC complex o The reason the lysis is more common at night is the slight drop in pH during sleep, which enhances complement activity o The leading cause of death in people with paroxysmal nocturnal hemoglobinuria is thrombosis o The only cure for paroxysmal nocturnal hemoglobinuria is bone marrow transplant - - Immunohemolytic anemia - hemolytic anemias caused by antibodies that bind RBCs and destroy them o You test for antibodies using the direct Coombs antiglobulin test – patients blood is mixed with antibodies and you look for clumping o Immunohemolytic anemias are categorized by the antibody that causes the issue: Warm antibody type- most common form Usually the problem is IgG The IgG binds to the Fc receptor of phagocytes, causing the phagocytes to do “partial” phagocytosis on the RBC membrane, like in hereditary spherocytosis, forming a sphere shaped RBC that gets stuck in the spleen and removed 2 ways this can be caused by drugs: o Antigenic drugs- in this case, large doses of the drug leads to hemolysis a week later Includes penicillin and cephalosporins These drugs bind the RBCs, and antibodies come find the drug-bound RBC, and opsonize it for phagocytes leading to extravascular hemolysis o Tolerance-breaking drugs – these drugs cause the making of antibodies to RBC Rh antigens Ex: α-methyldopa, an antihypertensive Cold agglutinin type Caused by IgM’s that bind RBCs in cold temperatures Can happen after infections, but resolves itself and doesn’t cause too many problems It’s more of a problem in chronic cases involving a B cell cancer IgM will bind in colder places like distal phalanges, and attach complement, which will opsonize the RBC when it gets back to warm areas Can cause pallor and cyanosis Cold hemolysin type The hemolysins are IgG’s in cool peripheral parts of the body Complement is attached and opsonizes Hgb back in warm temps Hemolytic anemia from RBC trauma o Conditions that increase shearing forces in the blood will damage RBCs as they pass through, forming RBC fragments called schistocytes Anemias from decreased erythropoiesis: - Commonly caused by nutritional deficiencies or kidney problems Megaloblastic anemias o Happens when there’s a problem in DNA synthesis, causing the making of big RBCs o o o o o o o o Often caused by B12 or folate deficiency B12 and folate are coenzymes in the making of thymidine, a base in DNA Without them, you get mutated DNA that delays or blocks cell division The RBCs in megaloblastic anemias will be macrocytic and oval shaped The RBCs will lack the normal paleness in the center of the RBC, and may be hyperchromic But the MCHC won’t be elevated The # of reticulocytes will be low in megaloblastic anemias Neutrophils will also be larger in megaloblastic anemias Megaloblastic cells will be seen in all stages of RBC development Problems with DNA synthesis will cause giant metamyelocytes, and band forms of RBC precursors Growth factors in megaloblastic anemia will tell the marrow to make more RBCs, causing enlargement of the bone marrow, but then most of the RBCs made will undergo apoptosis before they even leave the marrow B12 deficiency anemias B12 is aka cobalamin Normally, people depend entirely on their diet for B12 Meats have plenty of B12, while plants don’t have much Parietal cells of the fundic mucosa secrete intrinsic factor, which is needed to absorb B12 B12 is released from food proteins by pepsin in the stomach, and then binds to another protein to the duodenum, where proteases release it to bind to intrinsic factor Intrinsic factor takes it to the ileum, and the B12 gets endocytosed The ileal cells attach B12 to a carrier protein called transcobalamin 2, which takes B12 to the liver, bone marrow, and other parts of the body B12 is used in two rxns in the body Methylcobalomin is a cofactor in converting homocysteine to methionine with methionine synthase o The methyl released from B12 in this rxn goes toward making tetrahydrofolate (FH4) o FH4 is crucial in making dTMP, a precursor to DNA o So B12 impairs DNA synthesis by preventing making of FH4 o Methionine also gives a carbon to the making of folate o So the anemia from a B12 deficiency is caused by deficient folate, and treatment with folate can help Methylmalonyl CoAsuccinyl CoA , needs B12 for its enzyme, methylmalonyl CoA mutase to work o Folate doesn’t affect this one o o This rxn is important in neurons, and block causes methylmalonyl CoA to accumulate, leading to more fat in the neurons and myelin breakdown Pernicious anemia – a megaloblastic anemia caused by autoimmunie gastritis, making it so that no intrinsic factor is made, and B12 can’t be absorbed Pernicious anemia usually happens in older people, since the liver can store enough extra B12 to last years The type 1 autoantibody blocks B12-intrinsic factor binding o Most common The type 2 autoantibody blocks binding of the complex to the ileum The type 3 autoantibody inhibit gastric proton pumps Although the autoantibodies are involved, the main problem is an autoreactive T cell response that causes the mucosa injury and triggers the autoantibodies Pernicious anemia can also be caused by achlorhydria and loss of pepsin secretion, making it so that B12 stays stuck to food and not absorbed On top of other normal characteristics of a megaloblastic anemia, pernicious anemia will show atrophic fundic glands that is replaced by goblet cells, & CNS lesions, especially demyelination in the spinal cord You diagnose pernicious anemia when there’s megaloblastic anemia, low B12, increased homocysteine and methlymalonic acid, and leukopenia (low WBCs) Folate anemias Folate deficiencies cause the megaloblastic anemias that are the same as those from B12 deficiencies, due to problems with DNA making FH4 derivatives are intermediates in transfers of one carbon units (like methyl groups) Processes that depend on FH4 transfer of one carbons are: Purine synthesis Homocysteinemethionine dTMP making – leads to DNA The major causes of folate deficiency are decreased intake, increased need, and problem in using it Humans depend entirely on their diet for folate, which is common in green vegetables, fruits, and animals Heating foods, like in boiling, steaming, or frying, will destroy most of the folate The body doesn’t store as much folate as it does B12, so deficiencies don’t take as long to be apparent Pregnancy, infancy, and hemolytic anemias can increase the demand for folate Alcoholics often have problems with absorbing and using folate - Chemotherapeutic drugs like methotrexate, can inhibit dihydrofolate reductase, causing less FH4 and therefore DNA synthesis Difference between folate deficient anemia and B12 is that folate will be deficient instead, and methylmaloninc acid concentrations will be normal Since folate can possibly make the neuronal problems of B12 deficiency worse, you need to rule that out before you treat with folate Iron deficiency anemia o Iron deficiency is the most common nutritional disorder in the world o About 20% of heme iron is absorbable in the diet, as opposed to nonheme iron, which is just 1% o 4/5 of functional iron is in Hgb in the body o Storage iron like ferritin and hemosiderin is about 1/5 of total body iron Good cause free iron is toxic o Iron in the body is recycled between functional and storage iron o Iron is transported by transferrin, which is made in the liver o RBC precursors have high affinity receptors for transferrin o Ferritin is stored in the cytoplasm parenchymal cells of the liver, and macrophage of the spleen and bone marrow o Normal body iron levels don’t use much hemosiderin, but hemosiderin is very common in iron overload o Plasma ferritin levels are derived from the storage pool of body iron, so its levels correlate with body iron stores Go up when there’s iron overload, etc. o Body iron balance is maintained by regulating absorption of dietary iron in the duodenum o Nonheme iron is mostly in the ferric (Fe3+) state, and needs reduced to ferrous (Fe2+) iron by ferrireducatases to be absorbed DMT1 carries the iron into the small intestine cell o Absorbed iron either gets transported in the blood, or stored Iron to be transported gets carried in the intestine by ferriportin, which leads to oxidation back to ferric iron, which is then carried into the blood by iron oxidases hephaestin and ceruloplasmin The iron then binds to transferrin, and goes to the RBC precursors in the bone marrow o Iron absorption is regulated by hepcidin, which is made in the liver in response to increased iron in the liver Hepcidin inhibits iron transfer from the small intestine by binding and degrading ferriportin So high levels of hepcidin will keep iron stuck in the small intestine as ferritin, until that area gets sloughed and excreted Failure in making RBCs will inhibit hepcidin, even if levels of iron are high, causing more absorption of iron o - - Iron deficiency can be caused by poor diet, problem absorbing, increased need, and chronic blood loss Blood loss is the most common cause of iron deficiency o Only 10-15% of daily iron ingested is absorbed o ALWAYS ASSUME IRON DEFICIENCY IS FROM GI BLOOD LOSS, UNTIL PROVEN OTHERWISE To not consider this could mean you’d miss GI cancer o Iron deficiency anemia causes microcytic, hypochromic anemia Iron deficiency will show an increase in bone marrow RBC precursors Iron deficiency will also show in the bone marrow no iron in macrophage to stain Normal RBCs have a central zone of pallor, that is enlarged in iron deficiency anemia Hgb and hematocrit will be decreased in iron deficiency anemia Serum iron and ferritin will be low, and plasma iron binding capacity will be high Anemia from chronic diseases o Most common cause of anemia in hospitalized patients o Causes decreased RBC proliferation and decreased iron usage o Often caused by infections, immune disorders, and cancers o This anemia happens in chronic systemic inflammation Inflammatory mediator Il-6 stimulates an increase in liver making of hepcidin Hepcidin reduces transfer of iron from the storage pool to developing RBCs So RBCs starve for iron, even though the body has plenty stored o Will show low serum iron, low iron-binding capacity, and tons of iron stored in macrophage o Erythropoietin levels are also low – we don’t know why o The way to tell the difference between anemia from chronic disease and iron deficiency anemia: If there’s high serum ferritin levels and stored iron in macrophage, with a low iron binding capacity, it’s not iron deficiency anemia Aplastic anemia – anemia from bone marrow aplasia (no bone marrow) o Happens in chronic hematopoietic failure and pancytopenia (low blood cells) Pancytopenia – includes anemia, neutropenia, and thrombocytopenia o Usually an autoimmune thing, but sometimes its hereditary or acquired o Most cases of aplastic anemia are from exposure to chemicals or drugs Ex: drugs like chemotherapeutics that cause marrow suppression o Viral infection, especially hepatitis can cause marrow aplasia o Radiation can destroy marrow, and cause aplastic anemia o Activated T cells can suppress hematopoietic stem cells Happens when the cells are infected or damaged o The anemia can cause weakness, pallor, and dyspnea o - Also, the deficient bone marrow can cause thrombocytopenia, leading to petechiae, and neutropenia, allowing easy infection o There’s NO splenomegaly in aplastic anemia Pure red cell aplasia- suppression of only RBC progenitors in the bone marrow o Usually caused by something autoimmune, or parvovirus (which is transient) Myelophthisic anemia – form of marrow failure where space-occupying lesions, like cancer, replace bone marrow Kidney damage or renal failure will cause anemia – due to no erythropoietin