Anaphylaxis - Plymouth Hospitals
advertisement

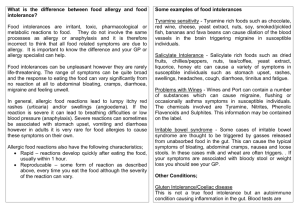
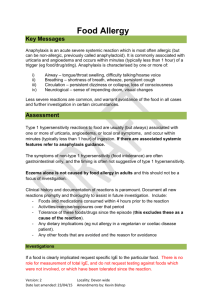
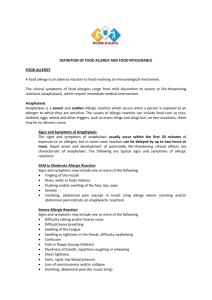
GP Guide to Anaphylaxis, Food Allergy and Food Intolerance The following is intended as a guide to the non-specialist management of anaphylaxis, food allergy and food intolerance. If the patient’s case falls outside of the stated criteria then a referral to the Peninsula Specialist Immunology and Allergy Service may be necessary for further assessment. Anaphylaxis Current NICE guidelines recommend that any patient who has experienced anaphylaxis to an unknown trigger should be referred to a specialist centre. If the causative trigger (eg a specific food) has been identified, referral may not be required as long as the patient has a clear emergency plan for future symptoms, as follows; Avoid specific identified trigger Education on symptom recognition in case of accidental exposure Knows to call 999 and use keyword ‘Anaphylaxis’ if develops severe allergic symptoms (difficulty breathing, dizziness) Self-injectable adrenaline (2 devices to be carried at all times) for use against anaphylactic symptoms (airway or cardiovascular compromise) if trigger unavoidable, ie not for drug reactions. Supply of long acting non-sedating antihistamines (eg, cetirizine 10mg) If anaphylaxis occurred to an identified drug trigger, primary and secondary care records should be updated with this information and the patient advised to wear a medical alert bracelet. A home supply of self-injectable adrenaline in this context is not required. If risk of subsequent anaphylaxis, and particularly if prescribing self -injectable adrenaline, ensure the patient is not on a non-cardioselective beta-blocker and that cardio-selective beta-blockers are changed to alternative medications if possible. Asthma care should be optimised. Any patient with a tendency to angioedema should avoid ACE-I. Food Allergy It is important to differentiate between food allergy and food intolerance. Food allergy can develop at any age although is more common in children and it can develop to any food, although some foods are more allergenic than others. Food allergy is characterised by a Type 1 Hypersensitivity reaction and therefore symptoms are rapid in onset and histamine mediated. Check the clinical history for foods and drinks ingested within 60 minutes of symptom onset and for the presence of typical immediate symptoms such as urticarial rash, angioedema, anaphylaxis and GI upset in context of the other symptoms. Multiple allergies can develop although this is less common. Any suspected food triggers would lead to similar symptoms after every exposure and symptoms would not be expected to occur unless exposure to that trigger had occurred, meaning that if the patient has eaten a suspected food SINCE the original episode without a problem, that food is excluded as the allergen. If the allergen is not easily identified on clinical history further investigation is recommended via referral to the Peninsula Specialist Immunology and Allergy Service, Derriford Hospital where skin prick testing and challenge testing can be considered. While waiting for the appointment the following actions are helpful; 1. Consider performing Specific IgE blood tests but only to foods specifically suspected from the history; there is no role for screening foods not implicated in the index reaction. However the presence of Specific IgE does not diagnose allergy and the results can often be difficult to interpret if the patient is atopic. 2. Prescribe self-injectable adrenaline if there has been any suggestion of airway or cardiovascular compromise during previous reactions (have a lower threshold for prescribing in asthmatics). If self-injectable adrenaline is prescribed (2 devices to be carried at all times), it is important the patient is taught how and when to use them (see above) 3. Optimise asthma care. Food Intolerance Food intolerance is a benign, although unpleasant, condition. Patients typically develop isolated and sometimes non-specific-gastrointestinal symptoms some hours after eating varied food groups. Patients will be able to tolerate small amounts of the foods and will find that the amount tolerated will vary day to day; this is the main differentiating factor from food allergy. No specific investigations are required and the mainstay of treatment is to exclude offending food groups. Reintroduction of those food groups periodically is useful as intolerance can resolve. It is essential that a patient maintain a balanced diet and if multiple exclusions are necessary the patient may benefit from a dietician review. The Peninsula Specialist Immunology and Allergy Service has a dedicated allergy-specialist dietician who accepts appropriate referrals; outside of this context there is little utility in a specialist allergy review unless Type 1 hypersensitivity to food has not been excluded (see above). Food allergy and food intolerance do not contribute to eczema in adults. Testing for food allergy (with specific IgE blood tests) without a supporting clinical history suggestive of type one hypersensitivity as described above will not be beneficial as the underlying pathology in eczema is not IgE mediated and results will be influenced by the underlying atopy.