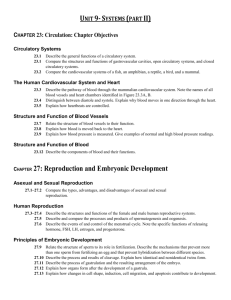
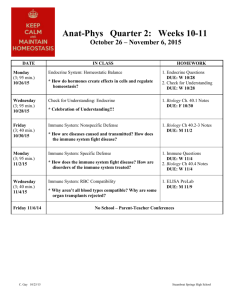
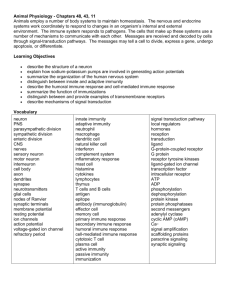
Pharmacology Ch 41 729-739 [4-20
advertisement
Pharmacology Ch 41 729-739 Principles of Inflammation and the Immune System Introduction – inflammation is a response to tissue injury and infection, characterized by rubor, calor, tumor, and dolor. -normal inflammatory response is acute and resolves after stimulus removal -the two pharmacologic strategies targeting immune diseases are: (1) modification of signaling mediators of inflammatory process, and (2) modification of underlying stimulus of inflammation Overview of the Immune System – distinguishes self from non-self -skin and other barrier tissues form first line of defense against infection, after which the body mounts an innate and adaptive response 1. Innate Response: stereotyped reactions of stimulus (histamine release, phagocytosis), that are non-specific and can process agent for adaptive immunity; first recognizer and activator of immune response 2. Adaptive Immunity: specific to offending agent (antibodies, T cells); creates a response to neutralize or kill agent -many cell types from 2 different progenitors: myeloid (innate) and lymphoid stem cells -adaptive immunity establishes memory for lifetime of individual Innate Immunity – cells are first responders to an offending agent; 3 tasks: 1. Defend against bacterial/parasitic infections by neutralization or phagocytosis 2. Phagocytosis initiates proteolytic digestion of microbial macromolecules to fragments that are displayed on MHC class II proteins on antigen presenting cells, which activate cells of adaptive immune system 3. Innate cells secrete cytokines that amply immune response -major cell types are granulocytes (neutrophils, eosinophils, and basophils), mast cells, and antigen-presenting cells (macrophages and dendritic cells) -Neutrophils - most abundant cell type specific for bacterial infection and are phagocytic as well as vesicular containing myeloperoxidase -Eosinophils – circulating granulocytes – PARASITE specific and secrete toxic substances -Basophils (circulating) and Mast cells (tissue resident) bind IgE, display IgE on cell surface, and maintain histamine-containing granules released when antigen binds IgE on cell. Important in allergic responses Antigen-Presenting Cells (APCs) – process macromolecules of invading agent and display its fragments on their surface to cells of adaptive immune system, and are important initiators of immune responses that provide costimulatory signals to T cells -Monocytes exit bloodstream and take up residence in tissues as macrophages -macrophages present antigenic fragments for T cells and are able to phagocytize and destroy pathogens themselves through enhancement by antibodies and complement -macrophages produce TNF-a to modify immune responses -Dendritic cells – APCs that are found in T cell areas of lymphoid tissue and are most important cells for initiating adaptive immune response Activation of the Innate Immune Response – Innate cells use common determinants present on many invading agents (lipopolysaccharide, etc…) and use patterns to initiate and phagocytize whole classes of infectious agents and not just one. (adaptive response specific for epitopes) -Innate immunity is a fast response, but same strength every time; whereas adaptive immunity is slower, but faster and more intense response the more times organism is exposed -Toll-like receptors mediate innate immunity by being able to bind to microbial components like lipopolysaccharide (LPS) expressed by gram-negative bacteria, mannans from fungi, and double stranded RNA expressed by viruses -10 TLRs are expressed in humans that are specific for different classes of ligands -TLR4 is specific for lipopolysaccharide -binding of TLR to their ligand initiates cascade that induces inflammatory cytokine expression to recruit other cells to site -Imiquimod may function as a TLR agonist Adaptive Immunity – there must be a mechanism to generate specific response to foreign antigen (regulated by major histocompatibility complex (MHC)), and adaptive immune cells must be able to distinguish self-antigens from non-self antigens Major Histocompatibility Complex – transmembrane protein that displays fragmented proteins on cell surface; exist as MHC class I and MHC class II -MHC Class I displays cytosolic proteins on ALL nucleated cells, and MHC-I on cells provides fingerprint for all proteins expressed within that cell (normally won’t be recognized by immune system unless it displays a foreign protein, such as that from a virus) -**MHC-class I is recognized by CD8+ T cells** -MHC Class II displays fragments derived from endocytic vesicles and are found mostly on antigen-presenting cells (macrophages/dendritic cells) -endocytic vesicles contain protein fragments from invaders after phagocytosis -**MHC-class II is recognized by CD4+ T cells** -these T cells stimulate APC to produce cytokines and chemokines to aid in T cell response against antigen -in general, MHC-I identifies infected cells whereas MHC-II identifies infectious agents Immune Diversity – somatic gene recombination and other processes account for generating the diversity needed to provide specific response against infection -recombination allows antibodies and T cell receptors to create variable regions, which can undergo somatic hypermutation to create additional diversity to recognize any structure Humoral and Cellular Immunity – B cells and T cells, respectively. Humoral response involves production of antibodies specific for an antigen which are secreted by plasma cells (differentiated B cells) and effective against extracellular infectious agents like bacteria -cellular response involves clonal expansion of T cells that recognize antigen and lyse them by blasting infectious agents with perforins and granzymes -each T cell evolves to recognize one specific MHC:antigen complex through its own T cell receptor (TCR). -T cells are divided into cytotoxic T cells (Tc) and helper T cells (Th) -Tc cells are the MEDIATORS of adaptive immunity and express CD8 receptor which recognizes a constant domain on MHC class I proteins; binds and secretes membrane-penetrating perforins and granzymes to kill the cell displaying the antigen -Th cells are the primary REGULATORS of adaptive immunity and express CD4 receptor which recognizes MHC class II proteins and binds it to activate the Th cell, which can differentiate into two different subtypes: Th1 and Th2 cells -Th1 Cell – produces IFN-g and IL-2, which influence CD8+ Tc cells and other CD4 cells -Th2 Cell – produce IL-4, IL-5, and IL-10 to enhance antibody production by B cells -Th2 cell is more often associated with autoimmunity -Th cells can mediate immunity by secreting cytokines that activate phagocytic cells -Th cell can differentiate into Th17 cell by stimulation from IL-23; Th17 produces IL-17 to recruit neutrophils and amplify immune response Tolerance and Costimulation – autoimmunity arises when diversity in variable regions allows T cell receptors to recognize self-antigens; two mechanisms for avoiding autoimmunity: 1. Clonal Deletion – T cells die during development when they express high-affinity receptors for self-antigens 2. Tolerance or anergy – cells of immune system undergo careful regulated series of steps during development to ensure that mature immune cells do not recognize self-antigens Costimulation – requirement for multiple signals ensures that single immune receptor does not activate a damaging immune reaction -signal 1 provides specificity, and signal 2 is permissive (appropriate inflammatory response is initiated) -if cell presents antigen without costimulatory signal, the cell undergoes anergy and will not respond to any further stimuli -For T cells, signal 1 is MHC:antigen:TCR interaction; signal 2 is CD28 on T cells with B7-1 (CD80) or B7-2 (CD86) on APCs -resting T cells present CD28 which can bind either CD80 or CD86 (not normally present on APCs unless increased by innate immune system during immune response) -lack of expression prevents inappropriate adaptive immune responses -upon receiving both signals, T cells express IL-2, undergo activation, and clonal expansion of Th cells for that epitope occur -Activated T cells eventually downregulate CD28 and upregulate CTLA-4, which binds CD80/CD86 with much higher affinity than CD28 to INHIBIT T cell proliferation -CD40 ligand (CD40L) – mediator of costimulation (active T cells express CD40L) which binds to CD40 receptor on APCs, B cells, and macrophages. -interaction of Th with CD40L on B cells promotes B cell activation, isotype switching, and affinity maturation -Interaction with macrophage CD40 promotes macrophages expression of CD80/86 for costimulation of T cells (positive feedback mechanism for Th and Tc cells) -hypothesized that blocking CD40-CD40L interaction would produce tolerance -Regulatory T cells – maintain peripheral tolerance and express CD4+/CD25+ Chemical Mediators of Inflammation – mediator of immune cell activity important for immunity Histamine – one initiator of inflammatory response is constitutively synthesized and stored in granules of mast cells and basophils, which migrate through tissues continually -any injury causes mast cells to release histamine into interstitium -histamine is vasoactive to dilate arterioles and venules, constrict veins, and contract endothelial cells Complement – serine proteases that are one of the first responses to injury; can be activated by antigen-antibody interactions (classical pathway), direct interactions with foreign bodies (alternative pathways),or by interactions with complex carbs (lectin pathway) -complement triggers inflammatory responses by 2 mechanisms: 1. cleavage products are potent stimulators of inflammation, for example: a. C3b is opsonin, C3a and C5a mediate leukocyte chemotaxis 2. Final step in complement activation is formation of membrane attack complex which causes pores in outer membrane of gram-negative bacteria leading to lysis Eicosanoids – metabolites of arachidonic acid (AA), a fatty acid component of phospholipids in inner leaflet of plasma membrane; inflammatory mediators release AA from membrane to cause a number of biochemical reactions to take place to create prostaglandins, leukotrienes, and others -some eicosanoids are proinflammatory, some are anti-inflammatory Cytokines – proteins that act in paracrine manner to regulate leukocyte activity. Interleukins are cytokines secreted by cells of hematopoietic lineage; IL-1 and TNF-a are 2 cytokines involved in acute inflammatory response -chemokines are a subset of cytokines that promote immune cell trafficking and localization to sites of inflammation -macrophage chemoattractant protein-1 (MCP-1) promotes monocyte transmigration and activation -granulocyte-monocyte colony stimulating factor (GM-CSF) and G-CSF are others The inflammatory response – inflammatory response typically happens in 4 phases: 1. vasculature around site of injury reacts to recruit cells of immune system 2. circulating immune cells migrate from vessels to injured tissues and neutralize threat 3. repair and tissue healing ensues 4. response is terminated Dilation of vessels – tissue injury causes localized inflammatory mediator release to dilate arterioles and venules to increase blood flow to site of injury causing redness and warmth -mediators also cause contraction of endothelial cells, leading to increased capillary permeability and development of exudate (interstitial fluid with protein content) -exudate develops into swelling Recruitment of Leukocytes – vascular permeability allows cells from blood to enter interstitium. Endothelial cells at site of injury express adhesion molecules that bind receptors on leukocytes, such as ICAMs which bind integrins on leukocytes, causing them to adhere and bind to other receptors that cause transmigration (diapedesis) into interstitium -neutrophils predominate early, monocytes after 24h Chemotaxis – once crossed into interstitium, cells migrate to specific site of injury through chemotaxis by mechanisms using N-formyl peptides from bacterial proteins or endogenous mediators such as C5a and leukotriene B4 (LTB4) Phagocytosis – at site of infection, neutrophils/macrophages are ready to perform after receiving one last signal. Foreign substances need to be coated by an opsonin, which is a molecular adaptor that coats foreign surfaces and signals leukocytes that these need to be attacked -opsonins consist of complement, antibodies, and collectins (plasma proteins that bind to microbial carbs) -interaction of phagocyte and opsonized particle caused engulfment and destruction Resolution – tissue repair and re-establishment of homeostasis are final events in acute inflammatory response, mediated by EGF, platelet-derived growth factor (PDGF), FGF2, TGF-B, IL-1, and TNF-a -these factors act on fibroblasts to cause healing and scar formation through angiogenesis and granulation tissue Chronic inflammation – pathologic state of continued and inappropriate response of immune system to an inflammatory stimulus; involved in autoimmune diseases; hallmark is presence of macrophages, which secrete collagenases and growth factors which initiate and maintain cycle of tissue injury and repair