Situational Judgement and WMS Curriculum
advertisement

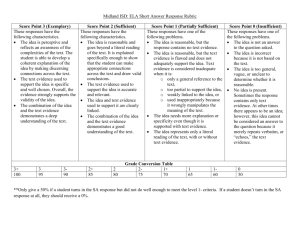
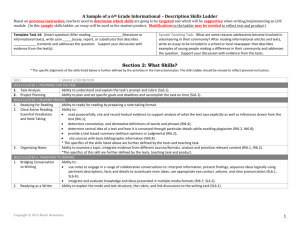
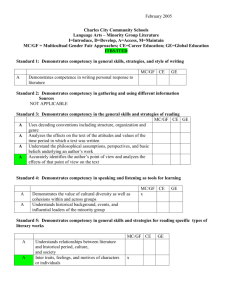
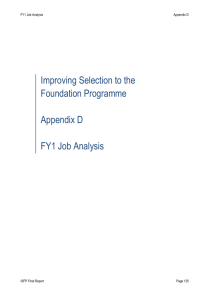
2012 Situational Judgement and WMS Curriculum By Frances Varian Third Year Medical Student 20/04/2012 Contents 1. Introduction ………………………………………………………………………………………………… 2 2. Summary and Recommendations ..………………………………………………………….…… 2 3. Advantages and Disadvantages of SJTs……………………………..…………..………. ………. 3 4. Recommendations for Present Curriculum ……………………………………………………… 4 5. Recommendations for New Curriculum……………………………………………………………. 5 6. Conclusion ……………………………………………………………………………………………………… 7 7. References ……………………………………………………………………………………………………… 7 8. Appendix A: the SJT domains………………………………………………………………………….....8 9. Appendix B: Phase II Student Handbook…..………………………………………………………12 10. Appendix C: Phase I Situational Judgement material………………………………………..24 1 1. Introduction As of 2013, the SJT has replaced the ‘white-space’ application process as the preferred method of assessment into the UK Foundation programme. This comprises 50% of the total application, with the other 50% from academic achievement. SJTs are a type of psychological aptitude test also known as ‘professional dilemmas’. Foundation applicants are presented with a variety of hypothetical situations likely to be encountered on the job. Accompanying each situation are multiple ways to respond to the scenario. The test taker is then asked to make judgements about the possible courses of action; either ranking five responses from most appropriate to least appropriate, or by choosing the three most suitable choices from a list of eight options. Answers are then marked according to a pre-determined scoring key. SJT selection in postgraduate medical training was introduced nationally in 2007 for short-listing candidates at stage 2 of GP recruitment. Here, three ‘non-clinical’ domains: empathy, integrity and coping with pressure, are considered in combination with a clinical problem-solving test. So far, these methods have proved widely successful (Work Psychology Group 2009). This report looks at what opportunities are presented by the introduction of SJTs for the WMS curriculum – both in its current form and for the revised 2013 curriculum. 2. Summary of Recommendations Key points about Situational Judgement Tests (SJT) for curriculum review: SJT domains pin down behaviours outlined by Tomorrow’s Doctors SJTs are a valid way of assessing Non-Technical Skills (NTS) NTS are weighted of equal importance to academic achievement in the Foundation Programme selection process NTS are areas where students can struggle and should be supported as such SJTs are a useful way to reiterate the importance of NTS to students SJTs give an opportunity to evaluate how well we are preparing students for practice What the SJT can do for WMS in a wider context: Highlight to the GMC where we are additionally teaching and assessing NTS Target key areas of assessment within the horizontal teaching themes Offer a proven way to assess (formatively) students’ knowledge of NTS 2 Provide material for personal tutors and clinical educational supervisors to actively engage with their students beyond a pastoral role. Opportunity to promote to prospective applicants how effectively we prepare students for practice. Recommendations: Use the SJTs as a mechanism for evaluating key learning points on professionalism, for example managing own health and challenging prior knowledge Use the SJT to draw out professional values from the perspective of the medical student, potentially introducing a system for recording and reflecting on mistakes Use case-based learning to consider prioritisation in more detail; for example, listing investigations in order of urgency Consider actors for scenarios beyond patient relationships: angry relative, distressed colleague Encourage students to communicate and work together as a multi-disciplinary team through scripted group-based scenarios Utilise personal tutors to encourage discussions concerning NTS Concentrate a few sessions on explaining diagnosis and management to relatives Ask FY1’s to feed into the case work to recall what they would manage in a particular scenario, who they would call for help and when. This will engage students in understanding the limitations of the FY1 role. 3. Advantages and Disadvantages of SJTs The increasing popularity of SJTs are attributable to the wealth of research supporting this selection method. The advantages of which include (Weekly & Ployhart 2005; De Meijer & Born 2009): Validity akin to cognitive ability testing Face validity – ie relevant to the job. This is useful for candidates as well as employers to provide a realistic preview of the proposed role. Incremental validity of selection above cognitive and personality testing Unique, multidimensional assessment of performance not captured by other methods Less adverse impact on ethnic minority groups Easier to score than other types of assessment such as the situational interview and hence, can be implemented into large-scale testing programmes 3 However, as with any selection process there are drawbacks. In terms of SJT, the disadvantages include: Variety of performance predictors: unclear as to what they actually measure Multidimensional: difficulties developing scenarios to measure one particular construct Assumes past behaviour can predict future response to a similar situation Debate over whether they are ‘fakable’ Designing an effective selection system requires thorough analysis of the knowledge, skills, attitudes and personal qualities needed to be successful in that role. With respect to foundation selection, the ISFP (Improving Selection to Foundation Programme) developed nine domains of assessment for UKFPO (United Kingdom Foundation Programme Office) application (Patterson et al 2010): Commitment to Professionalism Learning and Professional Development Working effectively as part of a team Patient Focus Problem solving and decision-making Self-awareness and insight Coping with pressure Organisation and planning Effective communication These domains are discussed in detail in Appendix A. In order to get around the debate concerning ‘fakability’ of SJT (Nguyen, Biderman & McDaniel 2005), the ISFP have introduced answers to ‘should’ rather than what you ‘would’ do, assuming that intentions are related to knowledge. More implicitly than this, they use the SJT to measure those ‘non-technical skills’ (NTS) expected of a junior doctor. 4. Recommendations for Present Curriculum WMS can further develop students’ non-technical skills through situational judgement. Given my involvement in the integration of SJT material into the current curriculum, my experiences as a student and through my participation in the student support committee and curriculum review meetings, the following material has been developed for integration: 4 Phase II: - Student workbook (Appendix B): incorporating reading list, interviews with FY1s to carry out (1 per block), observations to carry out, own scenarios to collect (2 per block) to be discussed with clinical educational supervisor (CES) - (Collected examples could then be used to feed in to the early years.) - 4 teaching sessions to be delivered by CES: 1 per block in senior rotation - Students to work through online SJT examples in Acute, Obs and Gynae, Child Health and Medicine blocks. Phase I: - Reworked ‘Becoming a Professional’ section of clinical skills 2 handbook to incorporate SJT domains and scenarios. These scenarios are all challenges a medical student may encounter on the wards and loosely cover each domain. - Scenarios to be discussed with their personal tutor group before the answers go up online (Appendix C). 5. Recommendations for New Curriculum Commitment to Professionalism: Although professionalism is a horizontal theme in which values and ethics features heavily, there are other aspects less well-approached. Owning up to mistakes is something that medical students should be doing. I think there should be a system for recording and reflecting when students make mistakes as this is what you have to do in practice. Also, responsibility for health is something that the personal tutors can draw out. I feel the tutoring system is presently there for ‘struggling’ students when really students should recognise their limitations before they get to that stage. Relating examples such as this within an SJT-style scenario should draw out such learning points as part of professionalism. Finally, learning to challenge knowledge and speak up is definitely something that could be better drawn out, particularly in the early years. The SJT can utilise these issues and get students engaging in the values now rather than values they think they need in four years’ time. I think the message of the ‘professional medical student’ is key to bring out. Coping with pressure: I have to be honest and I don’t think this is taught well in the current curriculum. Whilst students manage the pressure of a heavy workload, the pressures of multitasking and prioritising required on the wards are very different. There is a real opportunity to 5 work on this through case-based teaching; investigations and management should be put into context. I think this is something that should be brought into the complex, advanced cases in year two. Consider having a list of investigations for different patients and ask student to prioritise them: e.g. you are on a respiratory ward with x,y, and z, how do you proceed? Another source of pressure comes from difficult patients and colleagues. In this respect the SJT can be useful for discussion as well as assessment. I would also suggest WMS consider actors presenting as an angry relative or distressed colleague. This would be a great way of preparing students for life on the wards beyond patient relationships. Effective communication: I think communication – particularly with patients – is very well taught at Warwick. Record-keeping is also mentioned, however it would be good for students to practice filling in the forms they need eg death certificate. What I feel could be brought out more is negotiating with colleagues. As mentioned, an actor could be brought in to do this. You should also consider having a ‘script’ with a profile for each part. One example might be a patient complaint. In groups you could have one person playing a difficult colleague, the other a doctor and one the patient. You can therefore practice relaying difficult information from the patient to your colleague diplomatically. Teamwork and communication are integral to your job as a doctor, yet the difficulties associated with this have yet to be properly addressed. Organisation and Planning: prioritisation is something that can be incorporated into coping with pressure. There are also various techniques that students can use to prioritise their workload and perhaps this theory is something that the personal tutors could work on with the students together with an SJT scenario? Patient focus: I feel this is the domain that is best approached at Warwick. What perhaps is not as clear however is the amount of focus on patient’s relatives. From interviews on the wards, it is clear that most complaints come from relatives, as do breaches of confidentiality. I think it would be important to concentrate some sessions around explaining diagnosis and management to relatives – either because the patient cannot consent, or because they have asked you to explain it. Again these issues can be drawn out using SJT examples. Problem-solving: This is about taking initiative and seeking help. What I feel could be better at Warwick is drawing out what you would deal with yourself as an FY1 and what you would realistically call for help with. It would be nice to have a greater sense of your limitations before you start the role. This could easily be drawn out in case-based discussion alongside clinical 6 knowledge. Knowing the expectations of an FY1 in each scenario would be useful. You could quite feasibly ask a group of FY1’s to feed into your case work and have them say what they would and wouldn’t do for the steps in management and when they would call for help. Self-awareness and Insight: Reflection has already been mentioned to be included in the eportfolio. Beyond this, ‘boundaries and limitations’ are part of self-awareness and this is more difficult to teach. Nevertheless, understanding roughly where the limits of an FY1 lie will give students valuable insight into the role they will be doing. This also builds into teamwork and knowing your roles and responsibilities. Bringing in this information earlier will mean that students look out for it more on the wards because they have greater awareness of the NTS they need as well as the clinical skills. Teamwork: I have mentioned this in communication but I really think there could be more emphasis on teamwork in the curriculum. The personal tutors can really be utilised in this respect, drawing upon discussions about difficult or struggling colleagues. See Appendix C as examples of this from the current phase I material. 6. Conclusion SJT are a fantastic and fun way to get students engaged in NTS. We should however, in all cases, make these skills EXPLICIT to students. Students like to know the fundamentals behind their learning in juxtaposition to the expectations of an FY1. Ultimately it’s about preparing medical students for a job and the SJT really adds value in that respect. 7. References De Meijer, L.A.L. & Born, M. Ph (2009). The situational judgement test: Advantages and disadvantages. In M. Born, C.D. Foxcroft & R. Butter (Eds.), Online Readings in Testing and Assessment, International Test Commission available from: http://www.intestcom.org/Publications/ORTA.php Ngyen, N.T. Biderman, M.D. McDaniel, M.A. “Effects of Response Instructions on Faking a Situational Judgement Test” Int. J. of Selection and Assessment. Vol 13 (4): 250-260 Patterson, F. et al (2010) Improving Selection to Foundation Programme Final Report Appendix D: FY1 Job Analysis. Work Psychology Group and University of Cambridge; pp 126-240 Weekly, JA and Ployhart, R.E. (2005) Situational judgment tests: theory, measurement and application. Lawrence Erlbaum Assoc Inc, New York. 7 Work Psychology Group (2009) Evaluation of situational judgement tests to select postgraduate trainees: validation studies in two specialties [pdf] available from: http://www.workpsychologygroup.com/assets/Library/Library-SJTs-to-select-postgrauatetrainees-AMEE.pdf Frances Varian 19/04/2012 f.l.varian@warwick.ac.uk 8 Appendix A The domain descriptors: definition of the attributes and behaviours expected of an FY1. 1. Commitment to Professionalism Definition Behaviours Displays honesty, integrity and awareness of confidentiality & ethical issues. Is trustworthy and reliable. Demonstrates commitment and enthusiasm for role. Willing to challenge unacceptable behaviour or behaviour that threatens patient safety, when appropriate. Takes responsibility for own actions. Is punctual Takes responsibility for own actions/ work Owns up to mistakes Takes responsibility for own health and well‐being Demonstrates commitment to and enthusiasm/motivation for role Understands/is aware of the responsibility of the role of being a doctor Is reliable Displays honesty towards others (colleagues and patients) Trustworthy Identifies/challenges unacceptable/ unsafe behaviour/situations when appropriate (colleague/organisational issues) Challenges others knowledge where appropriate Understands/demonstrates awareness of ethical issues, including confidentiality 2. Coping with Pressure Definition Capability to work under pressure and remain resilient. Demonstrates ability to adapt to changing circumstances and manage uncertainty. Remains calm when faced with confrontation. Develops and employs appropriate coping strategies and demonstrates judgement under pressure. Behaviours Remains calm and in control of situations Manages uncertainty/ambiguity Effectively deals with outcomes of mistakes/decisions Exhibits flexibility/adaptability when dealing with changing circumstance or issues Employs effective coping mechanisms for dealing with stress/emotions Demonstrates good judgement under pressure Does not give up easily Deals appropriately with confrontational/difficult situations (colleagues/patients) Seeks support when faced with stress/pressure 3. Effective Communication Definition Actively and clearly engages patients and colleagues in equal/open dialogue. Demonstrates active listening. Communicates verbal and written information concisely and with Behaviours General Listens effectively Ensures surroundings are appropriate when communicating Understands/responds to non-verbal cues Uses non‐verbal communication effectively 9 clarity. Adapts style of communication according to individual needs and context. Able to negotiate with colleagues & patients effectively. With Patients Uses language that is understood by patients/relatives and free from medical jargon Demonstrates sensitive use of language Communicates information to patients clearly and concisely Adjusts style of communication according to patient’s/relative’s needs Adjusts how much information to provide according to patient’s/relative’s needs Provides information to patients and keeps them updated Readily answers patient’s and relative’s questions Ensures has all the relevant information before communicating to patients/colleagues Asks questions/seeks clarification to gain more information /understanding about the patient Finds out patient’s/relative’s level of knowledge/understanding Allows patients/relatives to ask questions/uses silence effectively Checks patient’s/relative’s understanding Summarises information/reflects back to patients to clarify their own understanding With colleagues Asks questions of colleagues to gain more information Provides/summarises information accurately and concisely to colleagues Provides only relevant information to colleagues Keeps colleagues informed/updated (about patients and about where they will be) Is able to negotiate/use diplomacy Knows exactly what are asking for and why Is assertive where necessary Adapts style of communication according to need and situation Clarifies information to check their own understanding Written Displays high standards of written communication Uses concise and clear written communication Has legible handwriting 4. Learning and Professional Development Definition Behaviours Demonstrates desire and enthusiasm for continued learning, takes responsibility for own development. Willing to learn from others and from experience. Is open and accepting of feedback. Demonstrates a desire and enthusiasm to learn and improve Is willing to learn from others Keeps up to date with knowledge Is willing to learn outside of work through reading around subject/access to internet Learns from previous experiences Learns from mistakes Takes responsibility for own learning 10 Demonstrates a desire and willingness to teach others. Is open to and accepts of feedback Is willing to teach others 5. Organisation and Planning Definition Behaviours Manages and plans workload effectively, displaying efficient time management and delivering tasks on time. Able to prioritise effectively and re‐prioritise where appropriate. Is conscientious and maintains accurate records. Demonstrates effective time management Prioritises tasks effectively Manages and plans workload/tasks Checks tasks are complete/follows up tasks Maintains accurate records 6. Patient Focus Definition Behaviours Ensures patient is the focus of care. Demonstrates understanding and appreciation of the needs of all patients, showing respect at all times. Takes time to build relationships with patients, demonstrating courtesy, empathy and compassion. Works in partnership with patients about their care. Able to gain trust from patients/instil confidence Is empathetic towards patients Is able to maintain appropriate distance from patients/ relatives Is willing to make self available to patients (for support/provide continuity/get to know them) Understands/considers the differing needs of patients Recognises that patients have different backgrounds/values/ beliefs Shows respect for patients Works jointly with the patient about their care Recognises the patient as the centre of care Shows a genuine interest in patients Shows compassion towards patients/relatives Is willing to spend time with relatives Builds rapport with patients Is polite, courteous and presents an open manner when dealing with patients Provides reassurance to patients Considers patient’s safety at all times 7. Problem-solving and decision-making Definition Demonstrates an ability to assimilate a range of information and identify key issues. Engages with the wider issues and thinks creatively to solve problems and reach appropriate decisions. Is proactive and demonstrates initiative. Is able to attend to detail. Behaviours Makes appropriate decisions based on all the relevant information Demonstrates ability to use own initiative Able to assimilate and integrate information effectively Understands problems from a wider perspective/takes into account whole picture Demonstrates good attention to detail Is proactive; takes charge of a situation and makes things happen 11 8. Self-Awareness and Insight Definition Behaviours Demonstrates awareness of the boundaries of their own competence and willing to seek help when required, recognising that this is not a weakness. Exhibits appropriate level of confidence and accepts challenges to own knowledge Is willing to seek help when needed Able to say no when faced with a situation/task they are not comfortable with/admit that they don’t know Accepts that asking for help is not a weakness Recognises boundaries/limitations of own competence Displays appropriate level of confidence in self/own ability Accepts challenges to own knowledge Accepts mistakes will be made 9. Working Effectively as Part of a Team Definition Capability & willingness to work effectively in partnership with others and in multi‐disciplinary teams. Demonstrates a facilitative, collaborative approach, respecting others’ views. Offers support and advice, sharing tasks appropriately. Demonstrates an understanding of own and others’ roles within the team and consults with others where appropriate Behaviours a recognition of others’ knowledge/skills/abilities/roles/ responsibilities Able to identify and utilise the most appropriate person for a task/situation Aware of own role/responsibilities within team Builds rapport and establishes relationships with other team members Supports others (in a non‐task related way Is willing to offer assistance with tasks/workload Is willing to offer/provide advice Values other people’s opinions and contributions Shows respect for colleagues Delegates and shares tasks effectively Maintains harmony within the team Identifies when others are in difficulty/are struggling Able to take on board team members’ perspectives Able to adapt role within team where necessary i.e. take on role of leader Shares knowledge and expertise with colleagues Is willing to take direction from others Consults with others and asks for advice Makes others aware of own workload 12 Student Workbook: Improving Your Situational Judgement Name …………………………………………………………. By Frances Varian and Lara Cartwright Contents Introduction …………………………………………………………………………… 3 Using this workbook ……………………………………………………………… 5 Task 1: Preparation ..…………………………………………………………….. 6 Useful references ………………………………………………………. 9 Task 2: Interviewing……………………………………………………………… 10 Task 3: Observation……………………………………………………………….. 18 Task 4: Recording Examples.………………………………………………….. 19 Introduction The selection process for the UK Foundation Programme has changed as of 2013. Instead of essay-style questions on an application form, final year medical students will sit a 2 hour 20 minute assessment of 70 items based on clinical scenarios encountered as a junior doctor, known as Situational Judgement tests (SJT). This counts for 50 points in total – 50% of your application What areas does an SJT cover? Commitment to Professionalism Learning and Professional Development Working effectively as part of a team Patient Focus Problem solving and decision-making Self-awareness and insight Coping with pressure Organisation and planning Effective communication What will an SJT question look like? You are looking after Mr Kucera who has previously been treated for prostate carcinoma. Preliminary investigations are strongly suggestive of a recurrence. As you finish taking blood from a neighbouring patient, Mr Kucera leans across and says “tell me honestly, is my cancer back?” Rank in order the following actions in response to this situation (1= Most appropriate; 5= Least appropriate). A Explain to Mr Kucera that it is likely that his cancer has come back B Reassure Mr Kucera that he will be fine C Explain to Mr Kucera that you do not have all the test results, but you will speak to him as soon as you do D Inform Mr Kucera that you will chase up the results of his tests and ask one of your senior colleagues to discuss them with him E Invite Mr Kucera to join you and a senior nurse in a quiet room, get a colleague to hold your ‘bleep’ then explore his fears Answer:DCEAB It is not a FY1’s responsibility to break bad news to a patient and the full results are not available yet. It would be most appropriate for a senior colleague to speak to Mr Kucera with regards his diagnosis. Informing Mr Kucera that you will speak to him as soon as you get the test results back would still be appropriate as you are giving him some information, although this may not necessarily mean that you would be providing him with the diagnosis. It may be appropriate to discuss Mr Kucera’s fears with him, but by doing this you may not be attending to other ill patients and are asking a colleague to take on your responsibility by holding your bleep. It may also become a difficult conversation when you do not have full details of the results. It would not necessarily be appropriate to tell Mr Kucera that his cancer is back as this has not been confirmed; however it would be inappropriate to provide false hope to a patient when preliminary investigations are strongly suggestive of a recurrence. This examples is from the Improving Selection to the Foundation Programme (ISFP). For more examples see: http://www.isfp.org.uk/SJT/Pages/Example-questions.aspx 1 How to use this Workbook This workbook enables you to use your clinical blocks to most effectively prepare for the SJT. Feel free to dip in an out but you will get the most benefit from systematically working through it as follows: Task 1: take time to understand the definitions for the areas covered by the SJT on pages 6 to 8. Use the references on page 8 to read more widely around the domains, or revisit them when things crop up on the wards. Task 2: Interview an FY1 on the ward – there are four templates in this workbook so try to get one example per block Task 3: Carry out practical observations to increase your knowledge in these areas. These include the types of scenarios that you will be asked about in the SJT. Task 4: Use this workbook to record your own examples either through interview or observation. Aim to complete two examples per block. If you keep in the back of your mind you need to evaluate ‘non-technical’ skills, scenarios will start popping out at you without too much effort. Bring this workbook with completed examples to your scheduled meeting with your Clinical Educational Supervisor to discuss with your group. 2 Preparation The following nine domains are used as the basis for assessment in the SJT which is designed to evaluate your nontechnical skills. Commitment to professionalism Displays honesty, integrity and awareness of confidentiality & ethical issues. Is trustworthy and reliable. Demonstrates commitment and enthusiasm for role. Willing to challenge unacceptable behaviour or behaviour that threatens patient safety, when appropriate. Takes responsibility for own actions Learning and Professionalism Demonstrates desire and enthusiasm for continued learning, takes responsibility for own development. Willing to learn from others and from experience. Is open and accepting of feedback. Demonstrates a desire and willingness to teach others Coping with pressure Capability to work under pressure and remain resilient. Adapt to changing circumstances and manage uncertainty. Remains calm when faced with confrontation. Develops and employs appropriate coping strategies demonstrates judgement under pressure Organisation and planning Manages and plans workload effectively, displaying efficient time management and delivering tasks on time. Able to prioritise effectively and re‐prioritise where appropriate. Is conscientious and maintains accurate records Self-awareness and insight Demonstrates awareness of the boundaries of their own competence and willing to seek help when required, recognising that this is not a weakness. Exhibits appropriate level of confidence and accepts challenges to own knowledge. Effective Communication Actively and clearly engages patients and colleagues in equal/open dialogue. Demonstrates active listening. Communicates verbal and written information concisely and with clarity. Adapts style of communication according to individual needs and context. Able to negotiate with colleagues & patients effectively Problem-Solving and decision-making Demonstrates an ability to assimilate a range of information and identify key issues. Engages with the wider issues and thinks creatively to solve problems and reach appropriate decisions. Is proactive and demonstrates initiative. Is able to attend to detail. 3 Patient Focus Ensures patient is the focus of care. Demonstrates understanding and appreciation of the needs of all patients, showing respect at all times. Takes time to build relationships with patients, demonstrating courtesy, empathy and compassion. Works in partnership with patients about their care Working effectively as part of a team 1. 2. Capability & willingness to work effectively in partnership with others and in multi‐disciplinary teams. Demonstrates a facilitative, collaborative approach, respecting others’ views. Offers support and advice, sharing tasks appropriately. Demonstrates an understanding of own and others’ roles within the team and consults with others where appropriate Useful References BMA on social networking tips: http://www.bma.org.uk/images/socialmediaguidance_tcm41-206859.pdf Doctors in difficulty - read about some scenarios (particularly the “first times” section) and ways to deal with them: http://www.bma.org.uk/doctors_health/index.jsp Good Practice: Surviving Sepsis Video: http://www.chfg.org/articles-films-guides/surviving-sepsis-a-humanfactors-based-approach GMC ‘Tomorrow’s Doctors’ (pp 7-25): http://www.gmcuk.org/education/undergraduate/tomorrows_doctors_2009.asp GMC: Good Medical Practice in Action - elearning interactive case-studies: http://www.gmcuk.org/guidance/case_studies.asp National Patient Safety Agency: http://www.nrls.npsa.nhs.uk/resources/patient-safety-topics/human-factorspatient-safety-culture/ Patient Safety First: http://www.patientsafetyfirst.nhs.uk/Content.aspx?path=/interventions/Leadership/ SBAR e-learning tool http://www.nottingham.ac.uk/nmp/sonet/rlos/patientsafety/sbar/ SJT Examples: http://www.isfp.org.uk/SJT/Pages/Example-questions.aspx If you want to read about some ‘Never’ incidents: http://www.chfg.org/wp-content/uploads/2012/03/NeverEvents-final2-1.pdf 4 Task 2: Interviewing Ask an FY1 about the following …. Commitment to Professionalism: Where have you seen confidentiality being compromised? Have you ever had to challenge inappropriate behaviour? Learning and development: How do you build up your CV? What tips would you give? What ‘teaching’ do you have as an FY1? Coping with pressure: What pressures do you find yourself under? Have you ever made a mistake? What did you do about it? Have you ever experienced a confrontational situation? Who do you turn to when you need help? Team working: Have you ever had difficulties with a colleague? What were they? Find out the roles of other team members on the ward – including administrative staff. 5 Task 3: Observation (tick the boxes when completed) Organisation and planning: Look at how the jobs are prioritised after a ward round. Go with an F1 to the coroners and witness death certificate procedure. Effective Communication: Recognise good communication and bad communication at every opportunity Listen to a referral and practice the SBAR approach with your clinical partner Go with a doctor to see how they negotiate a scan for radiology Patient Focus: Observe times where patient concerns and views are integrated into management Observe the options given to patients about their treatment. What did you learn about their needs? Notes…… 6 Task 4: Build your own scenarios 1. 2. 3. 4. 5. Try to fill in two per block … Identify the judgement area that the scenario most closely relates to Describe the situation Analyse what the dilemma was and why Explain what the doctor did Find out what the doctor should have done, either use references to answer this section or just ask them – they should have learned from the situation 6. Reflect on this scenario to understand what you learned from it 7. Bring any completed scenarios that you are not completely confident about to discuss with your educational supervisor. Example Template Judgement Area: Commitment to professionalism Situation: Doctor was needed on the ward but also had teaching scheduled. Dilemma: Patient care comes first but also responsible for own learning. How urgent are the tasks on the ward? How essential is it that they attend the teaching? Can they rely on my colleagues to get the relevant information for me if they cannot get away? What the doctor did: Got very stressed about the fact they had to be two places at once. What should the doctor have done: Analysed calmly the dilemma and weighed positives and negatives of going to teaching or not before acting on their decision. Doctor decided to stay on the ward and asked colleague to make notes for them as otherwise they would be delayed at work for too long. Reflection: I learned that you should always try to meet your commitment to attend teaching but that patient care comes first; hence there may be times where you have to compromise and sacrifice your own learning. 7 Judgement Area: Situation: Dilemma: What the doctor did: What should the doctor have done? Reflection: 8 Taking into account your experiences, the 9 domains and SJT exercises online; reflect on the following areas and consider: What have you learned about yourself? Did your judgement differ to what you should do? How? Why were there differences? How will you work on this? Professionalism: Pressure: Communication: Organisation and planning: Learning and personal development: Patient focus: Problem-solving and decision-making: Team-work: Self-awareness and insight: 9 Feedback Please tick one box for each of the following… 1. The interviews helped me to think about the role of an FY1. Strongly Disagree 2. Disagree Neutral Agree Strongly Agree Disagree Neutral Agree Strongly Agree Fair Good Very good Excellent The teaching with my educational supervisor overall was: Poor 6. Strongly Agree The online examples available for SJT preparation overall were: Poor 5. Agree Developing my own scenarios helped me evaluate situations for the SJT. Strongly Disagree 4. Neutral The observations helped me to identify with the role of an FY1. Strongly Disagree 3. Disagree Fair Good Very good Excellent My impression of preparation for the SJT overall is: Poor Fair Good Very good Excellent Additional Comments (on improvements or anything particularly good) … 10 Appendix C: Phase 1 Situational Judgement Material Q1. You return home after a long day in the hospital. You log on to Facebook and see that you have a friend request from a patient you interviewed and examined for a portfolio that day. You remember them being a similar age to you. What should you do? Rank these responses from most appropriate (=1) to least appropriate (=5) A. B. C. D. Accept the request and maintain a friendly relationship with the patient Ignore the request Decline the request and explain to them why you cannot be friends Accept the request but alter your privacy settings so they can’t see anything on your profile E. Accept the request and then remove them as a friend later on Domain How the question assesses the domain. Commitment to Professionalism Understands ethical issues of confidentiality and maintaining professional boundaries Deals with difficult situations involving patients, demonstrates good judgement Communicates information to patient appropriately Maintains an appropriate distance from patients, is polite to patients Able to say no to a situation Makes appropriate decision about problem Coping with pressure Effective communication Patient Focus Self-awareness and insight Problem solving and decision-making Answer: CBDEA C is the most appropriate option. You should never accept friend requests from patients. You should explain that you have a duty to uphold a professional relationship. The patient will understand this and should respect that boundary. B is the next most appropriate response as this is preferable to accepting a friend request. You are not under any obligation to explain yourself to the patient – but it is polite to do so. A, D and E are not appropriate as you should not accept friend requests from a patient – no matter how close to your age they are. This is crossing a professional boundary which is there for good reason. The option of altering your privacy settings towards them however is more tempting than E or A. A is the least appropriate option of these as establishing a friendly relationship with a former patient – regardless of whether you are a medical student – is wholly inappropriate. Reference: BMA (no date) Using social media: practical and ethical guidance for doctors and medical students [pdf] available from: http://www.bma.org.uk/images/socialmediaguidance_tcm41-206859.pdf 11 Q2: You are on the medical ward and asked by the junior doctor to put in a cannula. You try three times in one arm and fail to get one in. What should you do? Choose the 3 most appropriate options from the following list? A. B. C. D. E. F. G. H. Ask your clinical partner to have a go Try the other arm to see if you can get it in Tell the junior doctor that you couldn’t do it Don’t say anything and wait until the FY1 asks you about it Ask one of the nurses to do it Ask the patient whether they are OK for you to keep trying Fill your attempts on the cannula pathway form Leave the ward before the FY1 can ask you about it Domain How the question assesses the domain. Commitment to Professionalism Learning and development, self-awareness and insight Problem solving and decision-making, Organisation and planning Take responsibility for cannulation, reliable, honest about not doing it Remains calm in front of patient, knows when to give up, adapts to situation, seeks support when under pressure Relays problem with task to others Ensures that patient gets cannula as IV access will be necessary of their care Willing to learn from clinical partner, aware that should stop at three attempts Makes appropriate decision to delegate task Maintain accurate cannula pathway records Working effectively as part of a team Delegates to colleague and lets junior know Coping with pressure Effective communication Patient Focus Answer: ACG A is appropriate as your clinical partner should gain experience as well as yourself – you are both learning. You might even learn something from them. C is appropriate as you should let your junior know that you couldn’t get the cannula in – it may be a particularly difficult patient in which case they can give you reassurance that you will do it next time. G is appropriate as it is best practice to fill in one of these forms – including all the sites that you attempted. The form is usually pink but you can ask any of the nurses at your trust. B is not appropriate as you should not try venepuncture or cannulation after three failed attempts – you should let someone else have a go. D and H are not appropriate as it is your responsibility to let the junior know you have had problems cannulating a patient. If you don’t they may forget to ask, or assume that you did it and the patient may not receive their medications as they are supposed to. Some drugs need to be delivered at specific times and you not putting in the cannula and delaying telling someone could compromise their care. E is not appropriate as only some nurses are trained in cannulation. Moreover, they have their own jobs to do. This is typically a junior’s job – or a trained medical student! 12 Q3. You are in clinic. You consultant has asked you to take a history from a new patient. He directs you to a different side room. Your clinical partner volunteers to take the history. Whilst you are watching them you notice that they are sitting with their arms crossed and mutter ‘ah ha’ so much that the patient is clearly unsettled. You wonder whether they have listened to anything the patient has said at all. What should you do? Rank the following responses from most appropriate to least appropriate A. B. C. D. Ask them to summarise their findings to you before you see your consultant Tell the consultant that you think the history-taking was very poor Apologise to the patient for their behaviour Give your clinical partner feedback on the consultation, drawing on the good and bad points E. Ask your clinical partner what they think went well and could be improved on Domain How the question assesses the domain. Commitment to Professionalism Honest towards your clinical partner, challenges others where appropriate Challenging situation with colleague Recognising need for good communication, communicating with colleague Importance of communication with patients Willing to learn from others and teach others Identify your good communication skills Use initiative to help clinical partner Coping with pressure Effective communication Patient Focus Learning and development, self-awareness and insight Problem solving and decision-making Working effectively as part of a team Supporting your colleague, provide advice, respect your colleague, share knowledge Answer: AEDCB A is the most appropriate option as you want to gauge what your clinical partner understood from the conversation. That and presenting is an important skill to practice E is the next most appropriate option as an important part of communication is establishing a platform with which to discuss your opinions. Rather than tackling the issue head on, introduce it slowly and make your clinical partner think first about the consultation D is the next most appropriate option as you should give constructive feedback in a manner that this both supportive and critical. This will leave your partner feeling better than if simply point out the negatives. C is the not appropriate as this will make you colleague feel uncomfortable and probably the patient even more so. Showing up your clinical partner like this is not acceptable – you are potentially spending two years with them – don’t alienate them B is not appropriate as again this is undermining your colleague and being unsupportive. See Tomorrow’s Doctors (2009) outcome 15 on the expectations and importance of communication; at http://www.gmc-uk.org/static/documents/content/GMC_TD_09__1.11.11.pdf 13 Q4. You have been taught to use the vacutainers to perform venepuncture by your clinical skills nurse at one of the trusts. A junior doctor asks you to take some bloods from a patient. They check that you have been trained and ask what materials you use. They then say “Oh I can’t be bothered with those; I just use a butterfly needle and syringe…that’s much easier than the vacutainers”. What should you do? Choose the three most appropriate options from the following list A. B. C. D. E. F. G. H. Attempt venepuncture using the vacutainer method Ask the FY1 to explain how to use the needle and syringe Attempt to take blood using the needle and syringe Ask your clinical partner for advice Ask a nurse what equipment to use Ask the FY1 to show you how to use the needle and syringe Bring the query to the attention of your personal tutor Email the clinical skills nurse about learning the needle and syringe method Domain How the question assesses the domain. Commitment to Professionalism Coping with pressure Takes responsibility for actions Managing ambiguity, good judgement under pressure Negotiating and asking questions Patient safety involved in correct technique Desire to learn from FY1, using knowledge learned. Insight into lack of training and experience in use of needle and syringe. Recognition of other skills of FY1 and nurses Effective communication Patient Focus Learning and development, self-awareness and insight Working effectively as part of a team Answer: AGH A is appropriate as you have been trained to use the vacutainer and therefore should proceed to take blood using that method rather than attempt with something you don’t know G is appropriate as these are the types of situations you should discuss with your personal tutor. They should be able to give you support and guidance on training. H is appropriate as there may be a reason why you haven’t been shown the needle and syringe method. The clinical skills nurses are very helpful and are always open for you to email with advice – or even pop in to see them. Ideally skills such as this should be taught to you by someone who knows best practice. B and F are not appropriate as whilst you can learn many things from an FY1, venepuncture should really be taught by the clinical skills nurse so you learn best practice from the outset. There is not guarantee that the teaching from the FY1 is the correct way. C is not appropriate and potentially dangerous for the patient. D and E are not top options as you should be able to make this decision by yourself. You are the one who has been asked to do the venepuncture. 14 Q5: You are in group work. There is one group member who is always late, often doesn’t turn up and when they are there, rarely participates in the session. What should you do? Rank these responses from the most appropriate (=1) to the least appropriate (=5): A. B. C. D. E. Speak to them at one side after the session Talk to your personal tutor about them Comment on their lateness when they arrive to make a point of it Ignore it as this is not your responsibility Find out from your other colleagues in the group whether anyone else is concerned about their behaviour Domain How the question assesses the domain. Commitment to Professionalism Coping with pressure Challenging unacceptable behaviour Challenges peer pressure to conform and propensity to avoid conflict. Communicating with colleagues in an appropriate manner, being diplomatic The focus in this case is on your colleague Maximising group work as an effective learning environment, insight into the well-being of your colleague Recognising that organisation is an important skill, working thorough the situation where colleagues are disruptive. Getting opinions from your group members, maintains harmony within the group Effective communication Patient Focus Learning and development, self-awareness and insight Problem solving and decision-making, Organisation and planning Working effectively as part of a team Answer: EABCD E is the most appropriate response. This behaviour concerns the whole group. It will be likely that other members are annoyed by this. Also, it will give you a chance to share responsibility for the issue, as well as find out any information on the individual concerned that may be important – for example someone might know they are having some personal issues. You can then delegate someone to speak to them so they don’t feel intimidated A is the next most appropriate option once you have spoken to your group. B is the next most appropriate option as you should raise your concerns with your tutor – particularly as this student may be struggling. They will be in a position to help your group and the individual involved. You should try to speak to your colleague first to let them know you are going to do this as you don’t want to go behind their back if you can help it. C is not appropriate as this may cause arguments, or worse, embarrass them so they no longer want to attend group sessions. D is the least appropriate option. You have a duty to your colleagues as outlined by tomorrow’s doctors (2009) 23 (j) to flag up something if they put patients at risk – learn this skill early as it’s important. Ref: http://www.gmcuk.org/static/documents/content/GMC_TD_09__1.11.11.pdf 15 Q6: You are medical student in theatre. A patient is under general anaesthesia and before the operation starts your consultant asks you to practice doing a PR on the patient. You have not gained consent from the patient and there is nothing in the notes. What should you do? Choose the top three options from the following list: A. B. C. D. E. F. G. H. Do the PR as you should respect your consultant Flatly refuse to do the PR Ask the consultant whether the patient has consented Ask your clinical partner to do it Tell the patient afterwards that you did the PR Record in the notes that you did the PR Politely ask if you can do one on the next patient who has consented Raise your concerns with your educational supervisor Domain How the question is assessing this? Commitment to Professionalism Coping with pressure Effective communication Learning and development, self-awareness and insight Problem solving and decision-making, Organisation and planning Respecting GMC guidance on consent Pressure from consultant on student Communicating views appropriately and raising concerns with supervisor Respecting patient’s rights to know about invasive procedure PR is a valuable learning opportunity, should take up where possible. Deciding whether to follow orders or politely decline. Working effectively as part of a team Not making your clinical partner do it Patient Focus Answer: CGH C is appropriate as it is important to ask whether the consultant has checked prior to the patient undergoing a General Anaesthetic G is appropriate as this demonstrates that you are keen to get experience but that you don’t want to do anything that might not be acceptable for the patient H is appropriate as this incident may not be isolated and other students may have also been in this difficult position. Your educational supervisor is there to support you and you should discuss issues like this with them. A is not appropriate as bad practice is never acceptable B is not appropriate as you don’t want to create unnecessary conflict – a more tactful approach will mean your consultant looks on you more favourably D is not appropriate – just because you are uncomfortable doing it shouldn’t mean you can pass it on to your colleague to take the blame if it goes wrong. F is not appropriate as you should not be doing a PR without consent from the patient Reference: see GMC (2009) Tomorrow’s Doctors – outcome 3; 20 (c): http://www.gmcuk.org/static/documents/content/GMC_TD_09__1.11.11.pdf 16 Q7: You are in an ophthalmology clinic, a patient came in with a visual field defect and the CT scan confirmed they are having an ‘evolving stroke’. The consultant calls the patient into the clinic to tell them this. Afterwards the consultant asks you to take the patient to lie down in another side room whilst they wait for a bed to be available. The patient asks you in the room “tell me honestly what the doctor said, I could hardly understand a word they had such a thick accent…you just can’t get a good doctor that speaks English these days.” What should you do? Rank the following responses from most appropriate to least appropriate A. B. C. D. E. Explain to them the consultant said they are having a stroke Tell the consultant that the patient did not understand the diagnosis Tell them that comment was inappropriate and you will not tolerate racism Bring the patient back to see the consultant Tell them you will get someone to come and explain the diagnosis to them Domain How the question is assessing this? Commitment to Professionalism Coping with pressure Effective communication Patient Focus Be honest with your consultant Pressure from patient for explanation Communicates patient views to consultant Does not let their personal views get in the way of their care. Recognises that breaking bad news is not appropriate for you to deliver & seek help Takes charge of situation and uses initiative to solve problem Learning and development, self-awareness and insight Problem solving and decision-making, Organisation and planning Working effectively as part of a team Aware of responsibility to consultant and share knowledge with them Answer: EBDAC E is the most appropriate option as you should address the patient’s concerns but not compromise your position. B is the next most appropriate option as you have a duty to advocate for your patient and explain their concerns to your senior who can address them accordingly D is the next most appropriate option as that way the consultant can readdress their concerns. A is not appropriate as you should not be breaking this news to the patient. You don’t know how they will react, nor are you in a position to answer their questions appropriately C is not appropriate as the patient may simply be angry and accusing them of being racist will not be well appreciated. You should not be passing judgements on patients and have to bypass comments for the sake of their care. 17 Q8. Your exams are coming up and you are feeling the pressure. You can’t seem to shake that cold you got a month ago; you are not sleeping well and have been slipping behind. You have made a revision timetable and you are really concerned that you won’t get through everything before your exams. What should you do? Rank the following responses from most appropriate (=1) to least appropriate (=5) A. Do nothing, it’s probably temporary and you usually manage to get through everything in the end B. Speak to a friend about your concerns C. Speak to your personal tutor about your concerns D. Rework your revision timetable so that you can get through it all E. Ask a senior medical student for advice Domain How the question is assessing this? Commitment to Professionalism Effective communication Learning and development, self-awareness and insight Problem solving and decision-making, Organisation and planning Taking responsibility for own health and wellbeing Employs effective coping mechanisms for dealing with stress Communicating concerns appropriately Willing to seek help when needed and accepts this is not a weakness Proactive about getting support, planning ahead and recognising a problem. Working effectively as part of a team Consulting others for advice Coping with pressure Answer: CBEDA C is the most appropriate response as your personal tutor should be the first person to contact when you require support. They are in the best position to help you. B is the next most appropriate response as you should seek support from someone in a similar position to you who can identify and share your concerns. Peer support is something you will look to throughout your career as a doctor – and who you will likely learn the most from. Start voicing your worries early, rather than bottling them up. E is the next most appropriate option as hopefully you should be in touch with your medical Mum or Dad – or at least know someone senior though an extra-curricular activity. Seniors have been through it all before and so they will be able to give you guidance and hopefully give you some tips on how to manage the workload. There is strong evidence supporting the benefit of students furthering other student’s academic development and is therefore encouraged (Sobral, 2002). 18 D is not an appropriate coping mechanism. Reworking the timetable will increase the pressure on you and mask the true problem. You should be seeking advice early. A is the least appropriate response as you should always flag up struggles earlier rather than later. Hoping that it will go away is not dealing with the problem effectively. Moreover, the later you leave it, the worse things may get. Reference: Sobral, D, T. (2002) Cross-year peer tutoring experience in a medical school: condition and outcomes for student tutors. Medical Education 36 (11); 1064-1070 19 Q9: You are on the ward looking through some patient notes for a portfolio. The phone starts to ring. The nurses are busy with a drug round and there is no one else around. What should you do? Choose the three most appropriate options from the following: A. B. C. D. E. F. G. H. Answer the phone Wait to see if anyone comes to get it Take a message and hang onto it until someone comes Take a message and try to find someone free to deliver the message Ignore it and continue getting the information for your portfolio Go and get someone to answer the phone Ask your clinical partner to answer it as you are busy with your portfolio Take a message and interrupt the nurses on their drug round to deliver it. Domain How the question is assessing this? Commitment to Professionalism Coping with pressure Reliable, honest and trustworthy Managing uncertainty whether to answer phone Clarifies information, takes down message The phone call may be important regarding a patient. Recognises this is within their own competence to answer phone Prioritises tasks – phone call over notes. Recognises no one else to answer phone Effective communication Patient Focus Learning and development, self-awareness and insight Problem solving and decision-making, Organisation and planning Working effectively as part of a team Supporting other team members on the ward. Aware not to interrupt drug round. Answer: ADC A and D are appropriate as you are perfectly within your rights and position as a medical student to answer the phone and take a message. You don’t know why that person is ringing but wouldn’t you rather have your call answered. You can always take a message and say you will get someone to ring them back. You should always pass on the message and therefore finding someone to deliver it is appropriate. C is appropriate. It is your responsibility if you note it down but you should keep hold of it rather than interrupt the nurses on their ward round. B is not appropriate as you can always pass it over to someone if they arrive. Be proactive. E and F are not appropriate as you can answer a phone yourself. G is not appropriate as your portfolio can wait for 5 minutes. This is about prioritisation and recognising that you should stop what you are doing to complete a more urgent task. H is not appropriate as you should never interrupt a drug round – the nurses will get angry with you because this is how mistakes happen and patient safety is compromised. You should find someone who is free who can act on the message. 20