Vaccine Preventable Deaths
advertisement

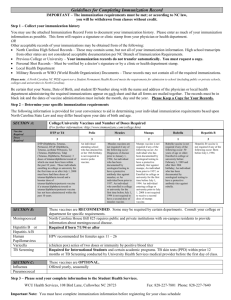
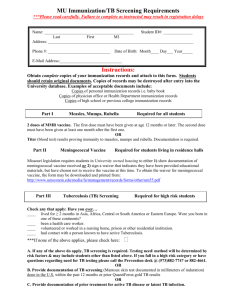
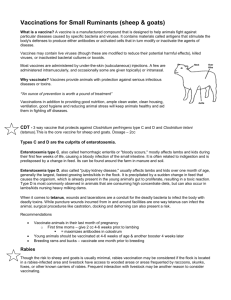
UNDERVACCINATION BY THE NUMBERS VACCINE PREVENTABLE DEATHS Child Deaths from Vaccine Preventable Diseases, 2008 Despite reaching 109 million children last year with three doses of the tetanus, diphtheria and pertussis (whooping cough) vaccine, 19.3 million children were not reached in 2010 (WHO, 2011). As a result of undervaccination, the WHO estimates that 1.7 million children under 5 still die from diseases preventable by vaccines currently recommended by WHO (2008 estimate) (WHO, 2011). Hib 15% Rotavirus 31% Tetanus (nonneonatal) 0% Pneumococcal Disease 31% Pertussis 12% Measles 7% Neonatal Tetanus 4% Hib 260,000 Pertussis 195,000 Measles 118,000 Neonatal Tetanus 59,000 Tetanus (non-neonatal) 2,000 Pneumococcal Disease 520,000 Rotavirus 527,000 This represents approximately 20% of under five child deaths and 30% of child deaths between 1 – 59 months old (WHO, 2011). Distribution in child deaths is not equal. Children in low-income countries are nearly 18 times more likely to die before the age of five than children in high-income countries. WHERE DO UNDERVACCINATED CHILDREN LIVE? If undervaccination is cause for nearly 20% of under five child deaths, where are they? Children who aren’t reached by 3 doses of DTP, which forms the basis of a traditional immunization program, are often unreached by traditional routine immunization systems – making it unlikely that they are immunized with other life saving vaccines. Of the 19.3 million children who were not reached by the third dose of the tetanus, diphtheria and pertussis in 2010, seventy percent live in ten countries: Afghanistan, DRC, Ethiopia, India, Indonesia, Iraq, Nigeria, Pakistan, South Africa and Uganda. (WHO, 2011) Though national level coverage is revealing, disparities within countries at the sub-national level can be stark. Geography: Many unreached children live in geographic locations which are costly and difficult to reach by traditional health facilities and immunizations. For example, UNICEF is working to increase vaccine coverage in communities that are unreached in Haiti, and estimates that targeting remote communities with low coverage rates can cost 1.5 to 4.5 times more per child than traditionally reached children (UNICEF, 2012). Partly as a result, only 5 African countries achieved the international target of reaching every district with at least an 80% DTP3 coverage in 2010 (WHO, 2011). Every African country with data had higher DTP3 vaccine coverage rates among urban children aside from Rwanda. Urban/rural disparities reach as high as 33% coverage differences in some countries (WHO, 2011). Why does this matter? Children in rural and remote areas are less likely to have access to treatment at health facilities should they become sick. Wealth: Like geography, children from the poorest quintiles are less likely to have been reached with three doses of the DTP vaccine. In Africa, all but two countries have coverage gaps between the richest and poorest quintile. Wealth disparities can be even higher than geographical disparities, with the greatest gap reaching 50% in Nigeria (WHO, 2011). Why does this matter? Children from poor households have much greater risks of dying from vaccine preventable diseases than children born in wealthier households (The GAVI Alliance). Though there is some data to show us where undervaccinated children live and what characteristics they may share, additional community-specific research is needed to understand the factors associated with underimmunization with life saving vaccines (WHO, UNICEF, World Bank, 2009). WHY ARE THESE CHILDREN UNDERVACCINATED? Though more research at the sub-national level is needed, researchers have undertaken analyses to propose common factors associated with children who are underimmunized. At the general level, disparities in vaccine coverage can be caused by limited resources, competing health priorities, poor health system management, and inadequate monitoring and supervision (Centers for Disease Control, 2011). At the more human level, factors associated with underimmunized children can be attributed to both the supply of, and demand for immunizations. Analyzing available data provided by district health surveys and multiple indicator cluster surveys reveals some trends across time and regions. Underimmunized children lack access due to geographical barriers, face missed opportunities at health posts (due to stock outs, misinformation/understanding, or health worker attitudes and performance). Their underimmunization may be impacted by other family characteristics, social exclusion and the educational status of their mother which impact their demand for vaccines (Eggers, 2010). What remains clear is that the strength of immunization systems and community involvement in immunization programs are two features that would address supply and demand side causes of undervaccination (Eggers, 2010). How this gets done is a topic that will need additional investigation. Works Cited Centers for Disease Control. (2011, 11 11). Global Routine Vaccination Coverage, 2010. Retrieved 1 25, 2012, from Morbidity and Mortality Weekly Report (MMWR): http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6044a3.htm The GAVI Alliance. (n.d.). Health Systems Goal Indicators. Retrieved 1 25, 2012, from The GAVI Alliance: http://www.gavialliance.org/results/goal-level-indicators/health-systems-goal-indicators/ UNICEF. (2012, 1 23). Vaccinating children in Haiti’s hardest-to-reach communities. Retrieved 1 25, 2012, from UNICEF: http://www.unicef.org/infobycountry/haiti_61402.html WHO. (2011, October). Children: Reducing Mortality. Retrieved January 2012, from World Health Organization: http://www.who.int/mediacentre/factsheets/fs178/en/index.html WHO. (2011, November). Global Immunization Data. Retrieved January 2012, from World Health Organization: http://www.who.int/immunization_monitoring/Global_Immunization_Data.pdf WHO. (2011, 10 3). WHO Vaccine Preventable Diseases Monitoring System. Retrieved 1 10, 2012, from WHO Department of Immunization, Vaccines and Biologicals: http://apps.who.int/immunization_monitoring/en/globalsummary/IndicatorSelect.cfm WHO, UNICEF, World Bank. (2009). WHO Publications. Retrieved 1 25, 2012, from State of the World's Vaccines and Immunizations, Third Edition: http://whqlibdoc.who.int/publications/2009/9789241563864_eng.pdf