Diabetes - Wandong Out of School Hours Care
advertisement
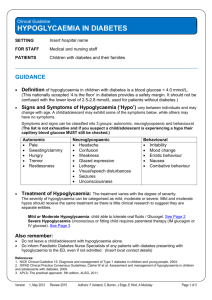
Policy No. 10 Diabetes Policy POLICY NO. 10 DIABETES POLICY Source Material. Diabetes Australia- Information Background. There are two recognised types of Diabetes- Type 1 and Type 2. Generally school children have type 1 Schools have a legal responsibility to provide: A duty of care Adequate supervision Students with diabetes can do everything their peers can do, but because of their diabetes, they will need: Special consideration Extra consideration if unwell Special provisions for privacy if testing blood glucose levels and injecting insulin at kindergarten Extra toilet privileges Closer supervision To eat at additional times, especially with physical activity Additional Care Where the service has been advised that there is a child attending who has been diagnosed with type 1 Diabetes, all staff (including relief staff) need to know about diabetes to ensure the safety of the student. This relates to hypoglycaemia, and safety in sport. It is the parent/guardian’s responsibility to advise the service of their child’s medical condition with on the initial enrolment form- or on an Addendum to the Enrolment Form. Families should provide detailed Individual Management Health Plans for their child’s diabetes. This Plan should be displayed at the service at any time that the child attends. What is Diabetes? Staff should be aware that Type1 Diabetes is caused by a severe deficiency of insulin and is fatal without life long insulin injections. It is an auto immune disease in which the body’s own immune system attacks the pancreas and destroys the body’s own insulin producing cells. Features include. Indications of insulin deficiency include: Lethargy Weight loss Increased urination Excessive thirst. Without treatment the disease progresses to life threatening conditions marked by dehydration and a build up of acids in the blood ( ketoacidosis). Management of a child with Diabetes. Insulin lowers the blood glucose levels and allows a return to good health. Insulin is not a cure- insulin must NEVER be omitted 1 16 January 2013 Policy No. 10 Diabetes Policy Treatment of Diabetes. 2 to 4 injections daily with a syringe or insulin pen or more recently, by a continuous infusion with an infusion with an insulin pump. The dose is adjusted according to blood glucose tests carried out several times a day. a regular pattern of snacks and meals. Staff should be aware that the timing of the child’s injections and food intake is important. What types of food to serve a child with Diabetes. Carbohydrate foods such as bread, fruit, sugar are essential and raise blood glucose levels while exercise and insulin lower blood glucose levels. TYPE 2 Diabetes. Not commonly seen in children of primary school age. May be seen in adolescents who are overweight. Can be treated with diet, exercise and tablets and occasionally injections. Low Blood Glucose A blood glucose level below 4mmo/L is too low in a child with Type 1 diabetes The cause of a hypo include: Too much insulin Physical activity Not enough food (see food and diabetes) Hypoglycaemia may occur at any time, but there is a greater chance of this happening with physical activity or before the next meal is due. HYPOGYLCAEMIA MAY BE DANGEROUS. Staff should be aware of the signs of Hypoglycaemia The signs may progress from mild to severe. Some children will recognise their own symptoms, others may not. Features that staff should look for are: Sweating and paleness, trembling, hunger, weakness. Changes in mood and behaviour ( crying, argumentative outbursts, aggressiveness) Inability to think straight, lack of co ordination. Moderately severe hypo additional signs develop and include: Inability to help oneself Glazed expression Being disoriented, unaware or seemingly intoxicated Inability to drink and swallow without encouragement Headache, abdominal pains or nausea. Severe Hypoglycaemia additional signs develop including: Inability to stand Inability to respond to instructions Extreme disorientation ( maybe thrashing about) Inability to drink and swallow ( leading to danger of inhaling food into lungs) Unconsciousness or seizures (jerking, twitching of face, body or limbs) 2 16 January 2013 Policy No. 10 Diabetes Policy Treatment Sometimes a student will do a blood glucose test at school to confirm a hypo. However, it is important not to waste time. If in doubt TREAT. Do not leave anyone having a suspected hypo alone or send them away for treatment by themselves. Alert the child’s family and treat as described An adult needs to stay with the child at all times to make sure the food or drink is actually consumed and the hypo is effectively treated. Easily Absorbed CarbohydrateAny one of the following will help in the event of a hypo. Fruit juice ( ½ glass or 125 ml) Soft drinks containing sugar ( ½ can or 125 ml) Glucose tablets or glucose gel equivalent to 10-15 grams Sugar, honey, sweetened condensed milk or jam ( 2-3 teaspoons) Jelly beans (4 large or 7 small) This treatment should be repeated if there has been no response within 10-15 minutes. Note: Often a student may be unco operative during a hypo and two people may be needed to help ensure that the student takes the carbohydrate. When recovery commences. Follow up the initial treatment 10-15 minutes later by giving additional carbohydrate foods. A sandwich, biscuits – equivalent to 1 slice of bread or a piece of fruit. For very small children, half of this amount is sufficient. These recovery foods will provide a more sustained release of carbohydrates and will maintain blood glucose levels in the normal range. Supervision. Adult supervision is needed until the child has recovered. If symptoms improve, the student may return to normal activity in approximately 15-30 minutes. If no improvement is apparent in this time, repeat the treatment. If symptoms remain notify the parents/ guardian or transfer to a hospital by ambulance. Recovery Some children take longer to recover than others, they may not be able to concentrate for up to 30minutes after a hypo. Headaches are common. Parents should be notified. Latest update: July 2012 3 16 January 2013