Apr 11, 2011 - School of Medicine
advertisement

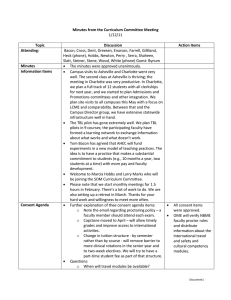
Minutes from the Curriculum Committee Meeting 4/11/11 Topic Attending: Minutes Information Items Consent Agenda Discussion Bacon, Byerley, Bynum, Cairns, Chuang, Cross, Darrow, Dent, Dreesen, Enarson, Farrell, Gilliland, Heck, Hobbs, Marks, Newton, Perry, Quinto, Rao, Serra, Shaheen, Slatt, Steiner, Stone, Viera, White, Woods No questions Comments included: The SOM strategic planning will be quite relevant to the work of the Curriculum Committee in terms of the development of mission, core policies such as bylaws (for faculty inclusion in ongoing activities), diversity and APT and then finally Admissions, including the possibility of rethinking our admissions process. Thanks to the Academy of Educators for Drs. Nivet and the Cruesses. Both were excellent. The professionalism workshops were foundational, coming just at the right time to inform our curriculum. Regarding comparability of grade, across clerkships, most give between 35-40% honors. Across campuses, there is also one clerkship that’s an outlier in terms of grade comparability. We are still off in inpatient medicine. There appears to be some differences in students across sites in that clerkship and will require a further look. The Assistant Dean/Directors of the Office of Special Programs has been offered. More later. LCME next steps: 1) Foundational is the reframing of all blocks/clerkships and sessions in terms of competencies and in light of our strategy for curriculum reform. 2) The core task forces will take place in late April and their input will come here and to CCs. One45 as necessary will be critical in support of and to manage new curricula including reports, clinical logs, the new clerkship evaluation form, mid-course evaluations, Advisory College and milestone report. Year-end retreats of each of the year curriculum committees will be reviewing a) the implementation of competencies in each course, b) calendar/duty hours, c) success of the year and priorities for improvement next year. School of Medicine CC retreat in late June is being scheduled. NB: We’ll also need a retreat in the fall. Approved except for the CTSA. Further discussion Action Items Coordination and timeliness is important. Committee endorsed Document1 about this. The report describes all of the courses that might do a component of the curriculum. Do we have endorsement of the general direction? Following Up the Retreat approach. Kurt will map precisely and report back. Other comments included: Do the clinical clerkships have a formal curriculum with respect to asking questions, reviewing articles and getting answers? How do we accomplish teaching patients about research? Clin. Epi. does both the formal questions and answers as well as teaching students to inform patients about research. There may be other opportunities as well. Strategies at the retreat decided upon are: Active learning in all courses As we create more active learning opportunities, an internal goals becomes decreasing lectures to less than 50% and requiring more accountability for students having read materials in advance in the third year. Systematic broadening of assessment process. The committee endorsed these. Proposed additions were: Reduce the numbers of core faculty teaching both in individual courses and ultimately across the curriculum. Push small groups and assigned readings/accountability in the first two years Have systematic programmatic measures and follow up these principles. Comments included: We need to be careful about the work inherent in “active learning.” If we add prep work and tests, it will add to student effort. Lots of tests will make courses complicated. We need to track student work time and probably decrease lectures to give time for studying. The School of Pharmacy was able to pull back (reduce by 2/3) and use class time only for face to face experiences. Perhaps we can create a system whereby students have options of lecture/iPods or last year’s lecture capture vs. problem based learning and groups. The idea is to accommodate individual learning styles. In the clinical years, students need to prepare for Document1 the clinical experience, not just the didactic experience. Again, we need to be careful about pushing them too far. Cameo lectures have a role, but the issue is they are much more likely not to fit in with the overall course/competencies and other things we are trying to do. Perhaps a way of framing it is the cameo lecture should be good only if it furthers the objectives of the course and if teaching is excellent. Student representatives were very supportive of reduced numbers of faculty within courses. Having some faculty who teach in more than one session and more than one course improves continuity and responsiveness of faculty. Consensus: We need to promote reduced numbers of teachers within individual blocks initially, and over the long term throughout the curriculum while preserving occasional good cameos and appropriate variation in the clinical years. Courses and years will need to come to their best solutions for their particular materials and to share best practices. The core principle is active learning throughout the curriculum. The group was divided about how much to push advanced preparation and accountability. Clearly, some of this is important, but the group was worried about going too far in terms of advanced preparation particularly if there wasn’t any lessening of student work in other areas and to respect student learning styles. C. Next steps on major priorities The next issue was strategies going forward. A proposal was: To have a plan for population health; will come back with a series of proposals for the May Curriculum Committee meeting. To develop plan for calendar changes, to begin that discussion at the next Curriculum Committee, do planning over the course of the next year and start in the following year (i.e., post LCME). Embedding regular ongoing assessment around these core strategies will be critical. Newton/Gilliland will come back with a proposal to CC regarding management of these strategies and improvement over time. CC1 and CC2 leaders will follow up with their CCs regarding incorporating strategies into play for next year. We will need to develop a policy on continuity of groups and other structures and peer feedback as a key part of these learning strategies. Newton, OME and Assessment Task Force will follow up on Document1 this. The Course Formerly Called ICM The proposed new name for ICM is Clinical Skills Development and Clinical Skills Integration (replacing ICM I and II). These are substantial changes from the prior ICM in smaller groups, emphasis on symptomsbased curriculum, increased emphasis on differential diagnosis and clinical integration, and rethinking of community experiences and use of simulations. Feedback questions included: General support for the strategy How will Pediatrics be developed? Ideally, one week block in for Pediatrics in years 1 and 2 then Pediatrics in the third year. The logistics are challenging. While we are developing this, we will try to integrate more clinical skills development with respect to Pediatrics . Core 24 symptoms are an important part of the new courses. This a major contribution to coverage of the UNC96 and the clinical integration around that. What about volume of ambulatory experience? Ideally, we would have each one of these in a half day of clinic/week over the first two years, but resources don’t permit that. We believe that there will be more clinical exposure to real patients in the current curriculum as we move forward. Will specific skills be taught? They could alter the transition to clinical clerkships. How should we integrate ICM material with other courses? Currently, we try to co-schedule and integrate a certain number of symptom-based problems into courses that are held at the same time. On discussion, we raised the question of whether or not we could include days in which we integrated symptoms, basic science and clinical management on a regular basis. Some medical schools do this with a weekly quiz . Students were very supportive of combining all of that. This is very consistent with their goals for this year. Student Self Study CC affirmed direction of development and new course names. OME will continue to work with ICM faculty to develop. OME will work with faculty in order to put these in place. OME will bring to the Curriculum Committee for discussion next time. People had a chance to review the synopsis. The full Document1 Education Certificate document will be coming out in 1-2 weeks. Any surprises? 1) The passion about laptops was strong. 2) The love for MBRB; the students explained that this should be seen in the context of the room itself but not the distance between the two parts of campus and in contrast to the other areas. 3) A surprise was what the students described as a “culture of disrespect” for students – more than single clerkship. It was a very concerning issue. Combined with some of our discussions around professionalism, this makes a need for more systematic treatment such as an emphasis on positive aspirational goals. It will be important to coordinate with the institution and develop procedures for both the positive and negative sides of it, along with a strategy for changing the professional culture. The focus for discussion is: Should we have certificates? These represent programs short of dual degrees with some significant investment of time/activities and which could be recognized in the Dean’s letter and transcript. OME and the task force on professionalism will be following up. We will review student self-study soon. OME will develop specific proposals for further discussion. Comments included: Students are quite interested in this. For some of them, medical education and health disparities research are passions. Some medical schools have developed tracks, as have residencies, that are attractive (and more substantial). It’s unclear whether residencies currently look at or would reward these things. Would this be a distraction given fundamental issues we have around quality of education and teaching of basic procedures, e.g., venipuncture? Do dual degree programs have more substance? Perhaps a priority should be expanding those programs further. Also, the clinical calendar redesign would support this substantially. Students can get some of this coursework in the first and second years. It doesn’t necessarily need to be in clinical years. Conclusion: Needs further discussion. If we do one, make sure that it’s robust enough and pilot one. Document1 Curriculum Committee Meetings (monthly) in 238 MacNider: 5/2 – 5-6:30pm 6/6 – 5:30-7pm 7/11 – 5-6:30pm 8/18 – 5-6:30pm 9/19 – 5-6:30pm 10/17 – 5-6:30pm 11/14 – 5-6:30pm 12/15 – 5-6:30pm Document1