Checklist Modification Guide/Frequently Asked Questions
advertisement

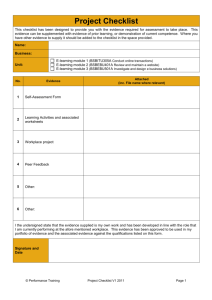
Checklist Modification FAQ Table of Contents South Carolina Checklist Template………………………………………………………………………………………………..…………….………Page 3 I. Understanding the Basics of Modification and How to Get the Most Out of Your Checklist………………….………Pages 4-9 Why do we need to modified our checklist?....................................................................................................Page 4 Who should modify the checklist in our hospital?............................................................................................Page 4 How can we make sure we are getting the most out of our checklist when modifying it?.........................Pages 4-6 What are some questions we should ask when modifying the checklist as a team?.......................................Page 6 Is the checklist the best way to take care of some problems?.........................................................................Page 6 Our surgeons are usually present before the induction of anesthesia. How can we make the checklist work for us?.....................................................................................................................................................................Page 7 Do you have examples of ways people have worded checklist items differently?......................................Pages 8-9 We work at a small facility and everyone knows each other by name. How do we incorporate the concept of introducing each other by name and role without having to perform formal introductions?.........................Page 9 II. Testing Outside of the OR...........................................................................................................................Page 10-11 How can we test our checklist before using it with a patient?……………………………………………………………………Page 10 How can we make sure our checklist contains critical elements before using it with a patient?...................Page 11 III. Testing Your Checklist with a Surgical Team in the OR................................................................................Pages 11What is a physician champion and how can we choose one? How should we display our checklist in the OR while we are testing it? Where can I get more information on checklist modification?......................................................................Page 2 When modifying your checklist, there is a process that you will want to follow to ensure that you are getting the most of your modified checklist. This document will take you through the steps of modification for creating a successful checklist. It will summarize checklist modification and will also answer frequently asked questions that we have been asked most often by hospitals when they are working on checklist modification. Below is a copy of the South Carolina checklist template that can be used to modify and fit with the practices in your hospital. 3 Understanding the Basics of Modification and How to Get the Most Out of Your Checklist Why do we need to modify our checklist? The checklist templates are not intended to be comprehensive. We recommend that every hospital modify the checklist to meet their specific needs. Modification of the checklist also creates buy-in from staff and ownership of the project. Additionally, the process of modifying the checklist is considered to be a key step in the implementation process. The modification process brings people together from all relevant disciplines and fosters teamwork that will enhance the use of the checklist. Who should modify the checklist in our hospital? Before you begin to modify the checklist it is important that you assemble an implementation leadership team. The implementation team should consist of at least one representative from the following disciplines: - Administrator - Anesthesia Provider - Nurse - Surgeon - Scrub tech - Any other people that you would like to include How can we make sure we are getting the most out of our checklist when modifying it? Retain Teamwork and Communication- The teamwork and communication items that are included on the checklist are considered essential items of the Safe Surgery 2015: South Carolina initiative and should not be removed. These communication and teamwork items can be found in the briefing and debriefing sections of the South Carolina checklist template as well as the item that prompts the surgical team to introduce themselves to one another or to the patient. In the United States these items have had a tremendous impact in improving surgical care and have positively changed the way in which surgical teams interact with one another and the patient. These items are meant to enhance communication around things in the OR that might not otherwise get communicated. The checklist template on page 5 shows the teamwork items on the checklist highlighted in green. 4 The other elements that are included on the South Carolina checklist template include items that ensure adherence to surgical processes while other items are targeted at enhancing teamwork and communication. Keep it Focused- The checklist should strive to be concise, addressing those issues that are most critical and not adequately checked by other safety mechanisms. If you feel that there are items on the checklist that are adequately checked and measured using established safety systems you can remove them. Keep it Brief- The checklist should take no more than a minute for each section to be completed and the whole checklist should never take longer than the procedure. While it may be tempting to try to create a more exhaustive checklist, the needs of fitting the checklist into the flow of care must be balanced with this impulse. The checklist should fit on onepage and be in a font size that is easy to read by all team members. 5 Make it Verbal- A major key to the function of the checklist is the fact that it is a verbal exercise among team members. Reading the checklist “out loud” as a team-exercise is critical to its success and it will likely be far less effective if used solely as a box checking instrument What are some questions we should ask when modifying the checklist as a team? Items that belong on the checklist are ones that have serious consequences if they are missed and things that need to be done and are commonly missed. When adding things to the checklist or taking items off the checklist, it is helpful to keep in mind the following questions, as they are ones we consider to be the most important to ask during the modification process. Is this a critical safety step at risk for it being missed? Is this a safety step that you might not notice if it is not done? Is this item discussed at a time when all relevant team members are present? Is this adequately checked by other mechanisms? Is the checklist the best way to take care of it? Can something be done about it? If the item will not help you, will this item help anybody here? Is the checklist the best way to take care of some problems? Glycemic control, fire risk assessment, hair removal, and checking pressure points are all items that hospitals have considered adding to their checklists. If you choose to add glycemic control or the fire risk assessment to your checklist, we have found that it is best if you use the checklist as a prompt for a protocol that you have in place. It is best if the checklist does not include the protocol but just the prompt for the protocol. Many hospitals have considered adding hair removal to their surgical checklists; however, the checklist may not be the best place to address this issue. Most times this is something that should be addressed before you go into doing your checklist. Some hospitals have also used the checklist to check for pressure points if they have had problems in the past. If you are considering adding this to your checklist, you will need to think about the procedures that you do and the risk that patient’s have for pressure points before you decide if it is necessary on your checklist. When considering adding any new items to the checklist you will need to keep in mind the questions above and remember that the more items that are on the checklist, the more difficult it becomes to do the checklist. 6 Our surgeons are usually present before the induction of anesthesia. How can we make the checklist work for us? The standard South Carolina checklist template has been designed with the briefing piece before the skin incision because often times the surgeon is not present until just before the skin incision. However, if your surgeons are always physically present before the induction of anesthesia, there is the option to move the briefing piece to the Before Induction of Anesthesia column (shown below). Both of these templates can be found here. To get the most out of this checklist template, the surgeon will always need to be present before the induction of anesthesia. Having the surgeon present at this point is ideal because you will able to take care of any problems that arise prior to the skin incision. 7 Do you have examples of ways people have worded checklist items differently? There are many items on the checklist that can be worded differently depending on the local culture of the hospital. The following are examples of alternative wordings for some of the most commonly modified checklist items. Blood Loss- Many individuals have had concerns that discussing blood loss when the patient is awake will frighten the patient. As a result some hospitals have chosen to modify the blood loss item that appears in the Before Induction of Anesthesia portion of the checklist (pictured below). While many facilities prefer to modify this language we feel strongly that if the patient should be aware that they might lose blood before they are brought into the operating room. The following are alternative wordings for the blood loss item: Are blood products required and available? What is the EBL? Blood (or cross-match) available if needed. Is there a need for blood products? Blood availability confirmed. EBL/blood plan Do we have adequate IV access? Is there a Type and Screen/cross done? Team Introductions- The section of the checklist template that is highlighted below shows the team introduction component of the checklist in which each person states their name and roll. This piece of the checklist is extremely important because introductions not only help surgical team members know who each other are in the OR but they are key in creating an environment where any team member can feel comfortable about voicing concerns about the patient. Below we have included various ways that team members can use to introduce themselves. The following are alternative wordings for introductions: We will start by introducing ourselves. Team introductions to patient, including name and role. Is there any unfamiliar staff in the room? Please introduce yourself by name and role. Safety Statement-The safety statement in which the surgeon asks anyone to speak up if they have a problem is highlighted below and is referred to as the “Surgeon Safety Statement”. This item on the checklist is essential for creating an environment where everyone in the OR can feel comfortable voicing concerns at any time during the case. The surgeon may want to express this statement in a different way, and we have included many alternative wordings of how this can be done. The following are alternative ways of saying the safety statement: Can take on many different forms as long as it has the spirit that the surgeon wants to open the room to communication if it is necessary If anyone on the team sees something that the team should know about, please speak up If anyone on the team sees something that the team should know about, please speak up anytime during the procedure If you see, suspect, or feel that patient care is compromised, will you speak up? 8 Remember that all are free to voice any concerns at any time throughout the procedure Does anyone have concerns? If you think there is a problem, please speak up Please speak up and out if you think something may not be right. We work at a small facility and everyone knows each other by name. How do we incorporate the concept of introducing each other by name and role without having to perform formal introductions? In some hospitals all team members truly know everyone by name and don’t feel like it is necessary to perform introductions before each case. If everyone in your hospital truly knows each other by name, it is still important that they have a chance to say something prior to the start of the procedure as it has been found this makes people more comfortable to speak up later if they see a problem. One way to do this is to have the surgeon address each team member by name and ask if they are ready to proceed before skin incision during each procedure. The picture below shows how this concept can be incorporated into your checklist and you can also find the template here. 9 Testing Outside of the OR How can we test our checklist before using it with a patient? After each modification of the checklist, it is important that it be tested before taking the checklist into the OR. We recommend that your team try using the checklist in an empty operating room or even in a conference room. We refer to this as a table-top simulation. A table-top simulation is an easy way to test the checklist outside of the OR and does not take a lot of time. Since the checklist is being done outside of the OR, there are no pressures of time or making mistakes and it can be practiced as many times as you need. This will help you learn whether or not your modified checklist will work in a real OR setting and it can prevent you from making big mistakes during an actual procedure. During the table-top simulation, you will run through your modified checklist with OR team roles assigned to each person to determine whether the checklist will work during an actual procedure. Many times, you may have to stop during the table-top simulation if something needs to be changed on the checklist. After you have run through the table-top simulation with the checklist, the team should discuss if any further changes need to be made to the checklist based on what happened during the simulation. 10 What are questions we can ask ourselves before using our checklist with a patient? Does your surgical checklist have three phases in the OR, before induction of anesthesia, before skin incision, and before the patient leaves the room? Are the items meant to be read out loud, without reliance on memory so all members of the team can hear them? Does every person that is present in the operating room have the opportunity to say something before skin incision, at a minimum they introduce themselves by name and role or state that they are ready to proceed? (This includes perfusionists, surgical assistants, PAs, residents, observers, manufacturer representatives, and other observers)? Will the surgeon share an operative plan and discuss: anticipated blood loss, expected duration of the procedure, possible difficulties, and implants or special equipment needed for the case with the entire team before skin incision? Will the nurses and surgical techs discuss with the entire team their concerns about the patient? Will the anesthesia providers discuss with the entire team the anesthetic plan and airway or other concerns? Will the surgeon ask the entire team to speak up if they have any concerns during the case? Before the patient leaves the OR, will ALL members of the surgical team discuss equipment problems that need to be addressed, key concerns for recovery and management, and anything that could have been done better to make the case more efficient? Does our checklist follow our current flow in the OR? Testing Your Checklist with a Surgical Team in the OR Before testing your modified checklist in an OR, there are some you will need to take to engage your colleagues and get the on board with using the checklist in the OR’s. What is a physician champion and how can we choose one? A physician champion is an important member of the implementation team and can help you to implement the checklist in your hospital. When thinking about choosing a physician champion, you will want to ask an enthusiastic surgeon who 11 is on board with the checklist work. They should be an informal leader and someone that others look up to because they will be able to talk to others and share their experience with the checklist. If you are having trouble finding a physician champion, nurses are a good resource to help you with this. Many times the nurses know which surgeons are easy to work with and would be open to this kind of work. When you approach a physician to ask them about becoming your champion you will need to outline what you will need from them as the champion. First, you will need to explain to them what they are being asked to do and what kind of help you are looking for. This will include helping to modify the checklist and potentially help test it, attend some of the implementation team meetings and help guide the project, and helping to talk to some of their colleagues about using the checklist. It is important that they know that there is a time commitment working on this project but they are not expected to attend every meeting or you are willing to work around their schedules for the meetings. How should we display our checklist in the OR while we are testing it? During the testing phase, there is a possibility that you may still modify the checklist and for this reason it is best to keep the checklist on a piece of paper rather than making a large poster or using an electronic medical record. While you are in the testing phase, you have several options: Have the circulator hold the checklist up in front of clinicians so they can read their parts aloud. Tape the checklist to an IV pole where clinicians can look at it and read their parts aloud. Have multiple copies of the checklist in the OR. Once you have tested your checklist in the OR and are happy with any modifications, you can move to hanging a large checklist poster, using an electronic medical record, or you can continue to use the checklist on paper. What do we need to do to test our checklist in the OR? When you decide to test your checklist inside of the OR, the team you are working with may not be your implementation team. If the team differs from your implementation team, you should test with a team that has enthusiastic members in all roles. Everyone on the testing team should be open to trying the checklist during an actual case. It is important to test the checklist in a straightforward and simple case. Preferably in a case where the patient is likely do well and the OR team can initially be somewhat distracted by the extra effort that they are going to have to put into doing the checklist. 12 It is a good idea to have a member of your implementation team in the OR when the checklist is being tested. An implementation team member can be a good resource to answer any questions that the surgical team may have about the checklist since they helped craft the checklist. Where can I get more information on checklist modification? Please visit the Modification and Customization section of our website or email us with any questions you might have at: safesurgery2015@hsph.harvard.edu 13
![Assumptions Checklist [Word File]](http://s3.studylib.net/store/data/005860099_1-a66c5f4eb05ac40681dda51762a69619-300x300.png)