Bukovinian State Medical University “Approved” on methodological
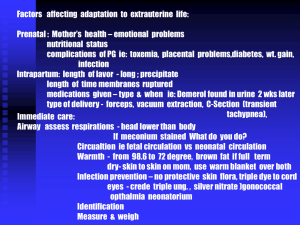
advertisement

BUKOVINIAN STATE MEDICAL UNIVERSITY “Approved” on methodological meeting of Department of Obstetrics and Gynecology with course of Infant and Adolescent Gynecology “___”______________________ 201_ year protocol # T.a. The Head of the department Professor ________________ O. Andriyets METHODOLOGICAL INSTRUCTION for practical lesson “Placental dysfunction. Fetal growth retardation. Pathology of neonatal period.” MODULE 4: Obstetrics and gynecology CONTEXT MODULE 9: Pathological flow of pregnancy, labor and puerperium Subject: Obstetrics and Gynecology 6th year of studying 2nd medical faculty Number of academic hours – 6 Methodological instruction developed by: ass.prof. Andriy Berbets Chernivtsi – 2010 Aim: to learn the causes, clinic, diagnostic, treatment and preventing measures of placental dysfunction and neonatal pathology, including asphyxia of the newborn. Basic level: 1. Physiology of placenta. 2. Condition of normal newborn. STUDENTS' INDEPENDENT STUDY PROGRAM I. Objectives for Students' Independent Studies You should prepare for the practical class using the existing textbooks and lectures. Special attention should be paid to the following: 1. Obstetrics terminology. 2. External and internal obstetric examination. 3. Ultrasound examination 4. Cardiotocography 5. Biophysical profile of fetus 6. Physiology of placenta. 7. Methods of examination of placenta. 8. Definition of primary and secondary placental insufficiency. 9. Diagnostics of neonatal asphyxia. 10. Methods of resuscitation of the newborn. 11. The most common neonatal diseases. 12. Medications for placental insufficiency treatment. Key words and phrases: Placental dysfunction. Fetal growth retardation. Pathology of neonatal period. PLACENTAL INSUFFIENCY (dysfunction) Placental insufficiency (PI) is a symptom complex conditioned by violations of transport, trophic, metabolic, and endocrine functions of the placenta due to structural changes.in it. Reasons: gestoses, miscarriage threat, immunoincompatible pregnancy, intrauterine infection, mother's diseases (pyelonephritis, essential hypertension, diabetes niellitus, anemia), etc. Classification I. By the term of onset 1) primary - develops in the terms of placenta formation (till the 16th week); 2) secondary — usually develops after the processes of placenta formation have finished. II. By the course: acute and chronic. Acute PI appears at. cute violation of decidual perfusion, for instance, at abruption of placenta -sharp violation of blood supply leads to fetal hypoxia or death. Chronic PI is characterised by gradual worsening of decidual perfusion as a result of the reduction of compensatory-adaptive reactions of the placenta to the action of pathological conditions of the maternal organism, has a long-term course, is accompanied by disorders, chronic oxygen starvation of the fetus. Chronic PI (depending on the condition, of compensatory-adaptive reactions) includes: 1. Relative ~ compensatory-adaptive reactions are preserved in the placenta: — compensated (the phase of persistent hyperfunctioning) develops at a threat of miscarriage and not severe forms of gestoses in cases, when these complications are successfully medically corrected; — subcompensated (the phase of exhaustion of compensatory mechanisms, which have begun) — is more often observed in the women, in whom a complicated course of pregnancy is developing against the background of extragenital pathology. 2. Absolute (decompensated) — the severest form of PI characterised by derangement of compensatory-adaptive reactions and develops against the background of chorion ripening disorders at placenta damages of involutive-dystrophic, circulatory and inflammatory character. Diagnostics 1. Regular clinical observation. 2. Dynamic ultrasonography in the 1st, 2"d, and 3"1 trimesters. 3. Dopplerometry. 4. Investigation of the hemostasis system. 5. Detecting the content of estradiol, progesterone, chorionic gonadotropin, and a-fetoprotein in the blood serum. 6. Investigation of estradiol secretion with urine. 7. Detecting the content of oxytocinase, general and placental basic phosphatase in the blood serum. 8. Colpocytologic investigation. Detection of the height of uterine fundus standing (HUFS) is very important in PI diagnostics, the diagnostic value of this method a! the term of 32 weeks makes 76 %. The main method of PI detection is ultrasonographic placento-nietry, which enables assessing placenta thickness, area, and struc-l uro. Placenta thickness from the 20th till the 36th week of pregnancy approximately equals the term of pregnancy in weeks: at 20 weeks — 20 mm, at 28 weeks — 28 mm, at 36 weeks — 36 mm, after this term the placenta does not thicken further. Placenta thinning (less than 20 nun) or thickening (more than 50 mm) testifies to PI, which appeared as a result of intrauterine infection, immunization, etc. At placentography there is carried out the assessment of placenta maturity by structure density singling out 4 maturity degrees (0—3). The Is' degree is characteristic of the 28th-32nd week of pregnancy, the 2"'L 32nd - 37'1' week, the 3rd degree of placenta maturity is characteristic of the term of pregnancy of 38—39 weeks, if it is detected earlier, it testifies to premature placenta aging and fetoplacental insufficiency. Ultrasonography also detects the biophysical fetal profile on the basis of its functional condition, qualitative and quantitative (in points) assessment of the indices of non-stress test, respiratory movements, motion activity, tone, amniotic fluid volume, placenta maturity degree. Normal indices of biophysical profile make 9— 12 points. Modern examination methods also include dopplerometric assessment of the blood flow. The essence of Doppler method consists in the feet that, depending on the speed of object moving relative to the source of wave radiation the length of the wave of reflected radiation changes. Such devices are used for the qualitative assessment, of blood flow in different vessels of the pelvic cavity of the pregnant woman: the uterine artery, carotid artery, umbilical artery, the descending part of the fetal aorta, medial cerebral artery. In case of necessity there are investigated the curves of speed performance of blood flow in the vessel under consideration. Most often investigation is conducted in. the umbilical artery and medial cerebral artery. Blood flow in the umbilical artery is detected by the contractile function of the fetal heart and resistance of the vessels of the fetal part of placenta, whose vascular resistance plays the main role in fetoplacental hemodynamics. The condition of blood flow in this vessel is the most informative index of the vascular resistance of the placental bloodstream. Diagnostic criteria: Normal blood flow — a high diastolic component in the dopplero-gram relative to the isoline, the ratio of systole amplitude to diastole is not more than 3. Pathological blood flow: 1) decelerated blood flow — diastolic component reduction, the ratio of systole amplitude to diastole is more than 3; 2) terminal blood flow testifies to a strong probability of antenatal fetal death; 3) zero blood flow stops in the diastole phase (there is no diastolic component in the dopplerogram); 4) negative blood flow acquires reverse direction in the diastole phase. At PI blood supply to the medial cerebral artery increases. This brain-sparing phenomenon reflects the compensatory centralization of blood supply to the essential fetal organs. Investigation of the content of placental hormones and fetoplacental complex (estriol, placental lactogen, choriomammotropin, etc.) in biological fluids may diagnose violations of fetal condition at the presence of different pregnancy complications or extragenital pathology. The severity of fetal condition correlates with the amount of secreted hormones. FETAL DEVELOPMENT DELAY Fetal development delay (FDD) or fetal hypotrophy is a pathological condition, at which the newborn's weight or biometric parameters of the fetus are not up to gestational age. Classification 1) Symmetric - the weight and length of the fetus are proportionally reduced, all the organs are evenly reduced in size; 2) Asymmetric — fetal weight reduction at normal indices of its length, unproportional dimensions of different fetal organs (Table 1). Table 1. Differential FDD Diagnostics Symmetric Asymmetric mi Beginning 2 trimester 3"1 trimester Fetbmetty Delay of all dimensions increase Delay of abdomen dimensions increase Placental From the 24"1 25"' week After 32 weeks blood flow Amniotic Oligohydramnios Norm disorders Malformation Frequent Rare fluid s At symmetric hypotrophy newborns have small body weight at birth, such a child cannot be differentiated from a premature newborn. The symmetric form is observed at severe disorders of intrauterine development beginning from the 2nd pregnancy trimester. At asymmetric FDD newborns have a considerable weight deficit at normal body length. This from is characteristic of the fetuses, in which unfavorable development conditions began in the 3rd pregnancy trimester. 3 degrees of FDD severity: the 1st degree - delay by 2 weeks; the 2nd degree — from 2 to 4 weeks; the 3rd degree — more than 4 weeks. FDD takes place due to the following reasons: chromosome anomalies and hereditary metabolic disorders, congenital defects caused by other factors, prenatal viral infections, action of ionizing radiation and medicinal preparations, placenta pathologies, mother's diseases, intoxication, malnutrition. Diagnostics If FDD is suspected, complex examination of the pregnant woman is conducted including: 1. Detection of the HUFS and abdomen circumference in dynamics (the weight of the woman should be taken into account). HUFS dimensions delay by 2 cm or the absence of any amount of growth during 2—3 weeks at dynamic observation allows suspecting FDD. 2. Sonographic fetal biometry. To asses fetal biometry there are detected the biparietal diameter of the fetal head (BDFFI), diameter of the chest and abdomen, length of the fetal hip. Gestational age of the fetus is assessed by the complex of signs. If there is detected inadequacy of one or a couple of basic fetometric indices to pregnancy term, extended fetometry is conducted, correlation of the frontooc-cipital and biparietal. dimensions, head and abdomen circumference, biparietal dimension and hip length, hip length and abdomen circumference is calculated. 3. Assessment of the biophysical fetal profile. 4. Detection of the level of hormones in the maternal organism and amniotic fluid. 5. Dopplcrometry of the blood flow speed in the umbilical artery. Treatment PI therapy should be begun with the treatment of the fundamental illness and prevention of unfavorable factors influence. Medica-mental therapy consists in the administration of drugs, which improve the uteroplacental blood flow (sygethin), microcirculation in the placenta and rheological properties of blood (dipiridamol, aciove-gin, essentiale, chophytol), have antioxidant properties (tocopherol). The increase of the uteroplacental blood flow is also promoted by hyperbaric oxygenation. Delivery 1. Delivery through the natural passages is conducted under cardiomonitoring control of the fetal condition at normal or decelerated blood flow in the umbilical arteries, if there is no fetal distress (BFP assessment — 6 points and less). 2. Indications to cesarean section: — critical changes of blood flow in the umbilical arteries (zero and reverse) — urgent preterm delivery is to be conducted irrespective of the pregnancy term; — acute fetal distress (bradycardia < 100 bpm and pathological heart rate decelerations) irrespective of blood flow type (normal or decelerated) in the umbilical arteries during pregnancy; — pathological BFP (4 points and less) in the absence of biological maturity of the neck of uterus (after 30 weeks of pregnancy). There is no efficient method of FDD treatment, therefore the key moment in managing such pregnant women is the clear assessment of fetal condition and timely delivery. Prevention 1. Detecting of FDD risk factors and conducting dynamic control over this group of pregnant women. 2. The pregnant woman holding to the day regimen and rational nutrition. 3. Giving up pernicious habits (tobacco smoking, alcohol consumption, etc.). FETAL DISTRESS. POSTNATAL ASPHYXIA FETAL DISTRESS Presently all the violations of fetal functional condition are denoted by the term "fetal distress". It should be noted that with the help of modern noninvasive methods of investigation it is impossible to find the true reasons for fetal cardiac dysfunction. Therefore in clinical practice one should use the term "fetal distress" instead of "chronic fetal hypoxia" and "acute fetal, hypoxia", which are not clinical. In its turn the term "fetal hypoxia" means the state conditioned by the reasons, which lead to acute or recurrent restriction of access of oxygen to the fetus or to the violation of fetal ability to use oxygen in cellular metabolism. The notions of "fetal hypoxia" and "postnatal asphyxia" must be clearly defined. It should be noted that the term "hypoxia" is to be used in relation to the intrauterine fetus, because, in spite of significant biochemical changes shown by blood analysis, hypocapnia and not hypercapnia declares itself. Concerning newborns it is more correct to use the term "asphyxia", which means the violation of gas metabolism with the development of hypoxia, hypercapnia, and acidosis. Etiological factors of fetal hypoxia are divided into preplacental, placental and postplacental. Preplacental: 1. A group of pathological conditions leading to the violation of oxygen transport to the uterus and placenta: — violation of maternal blood oxygenation (cardiovascular and pulmonary pathology of the mother); — hemic hypoxia of the mother — anemia of pregnancy at Hb < 100 g/L; — generalized circulatory injury (hypotension of pregnancy, essential hypertension, preeclampsia with predominant hypertensive syndrome). 2. Circulatory injury in the uterine vessels: - pathological changes of the spiral arterioles in the area of the placental bed as a consequence of inflammatory diseases of the endometrium and abortions in the history; - occlusive vascular violations of the spiral arterioles in the area of the placental bed, peripheral vasoconstriction (preeclampsia, over mature pregnancy, diabetic retinal angiopathy). Placental proper. - primary placental insufficiency caused by a disturbance of the development and maturation of the placenta (small placenta, placenta bipartite, angioma, etc.); infectious-toxic injuries to the placenta in the late terms of pregnancy; - detachment of placenta. Postplacental: - flexure of the umbilical cord (prolapse, compression, winding, knot); - fetal malformations and pathologies. By the rate of development there is differentiated acute and chronic hypoxia. The reasons for acute hypoxia:, placenta detachment, umbilical factors, inadequacy of the perfusion of the intervillous lacuna of the maternal part of the placenta at acute maternal hypotension (anaphylactic shock, metrorrhexis). All the other listed above factors lead to chronic fetal hypoxia. The main clinical manifestations of fetal hypoxia are: 1) the change of heartbeats character (heart rate, the change of heart sounds, arrhythmia); 2) the change of fetal movements intensity; 3) the appearance of meconium in the amniotic fluid (except for (he cases of pelvic presentation). However, the diagnosis of fetal hypoxia only on the basis of these data not infrequently has erroneous results. In this connection to confirm fetal hypoxia there are detected the indices of the acid-base balance in the blood taken from the skin of the fetal head. A characteristic sign of hypoxia is evident reduction of BE, pH of blood lower than 7.20. Fetal Distress in the Course of Pregnancy For the diagnostics of fetal distress in the course of pregnancy the following methods are used: 1. Auscultation of heart. Junction (beginning from the 20th week of pregnancy) — heart rate bigger than 170 bpm and less than 110 bpm testifies to fetal distress. Auscultation of fetal heart function is carried out at each visil of an obstetriciangynecologist or a midwife. 2. BFP (from the 30th week of pregnancy) - the total of the points for biophysical parameters is evaluated: - 7-10 points - satisfactory fetal condition; - 5-6 points - doubtful test, (to be repeated in 2-3 days); 4 points and less - pathological evaluation of the BFP (the question of urgent delivery is to be decided). 3. Dopplerometnj of blood velocity in the umbilical artery (reflects the state of microcirculation in the fetal part of the placenta, whose vascular resistance plays the basic role in fetoplacental hemodynamics). Diagnostic criteria: 1. Pathological blood flow: - decelerated blood flow - reduced diastolic component; the ratio of systole to diastole makes more than 3; - terminal blood flow (testifies to a strong possibility of antenatal fetal death). 2. Zero — the blood flow in the diastole phase stops (no diastolic component in the dopplerogram). 3. Negative (reverse) — the blood flow in the diastole phase acquires reverse direction (the diastolic component below the isoline in the dopplerogram). Management of pregnancy with fetal distress: 1. Treatment of concomitant diseases of the pregnant woman, which lead to fetal distress. 2. Staged case monitoring of the fetal condition. 3. Outpatient observation and prolongation of pregnancy is possible at normal indices of the biophysical methods of fetal condition diagnostics. 4. At decelerated diastolic blood flow in the umbilical arteries BFP investigation should be conducted: — if there are no pathological BFP indices, repeated dopplero-metry is to be conducted with an interval of S—7 days; — if there are pathological BFP indices, dopplerometry is to be conducted at least once in two days, the BFP — daily. 5. Detection of the deterioration of blood flow indices (onset of constant zero or negative blood flow in the umbilical arteries) is an indication to urgent delivery by means of cesarean section. Treatment: — Till 30 weeks of pregnancy the treatment of concomitant diseases which lead to fetal distress — After 30 weeks of pregnancy the most effective and justified method of fetal distress treatment is timely operative delivery. Delivery: 1. Is possible through the natural maternal passages (at cardiomonitor control over fetal condition) at: — normal or decelerated blood flow in the umbilical arteries, if there is no fetal distress (6 BFP points and less). 2. Indications to urgent delivery by means of cesarean section after 30 weeks of pregnancy are: — critical changes of blood flow in the umbilical arteries (zero and reverse); — acute fetal distress (pathological bradycardia and heart rate deceleration) independent of the blood flow type (normal or decelerated) in the umbilical arteries during pregnancy; — pathological BFP (4 points and less) at the absence of biological maturity of the uterine cervix. Prevention: 1. Detection of the risk factors of arrested fetal development and conduction of case monitoring of the patients of this group. 2. Adhering to the day regimen, rational nutrition. 3. Quitting bad habits (smoking, alcohol consumption, etc). Fetal Distress in the Course of Delivery To diagnose fetal distress in the course of delivery the following methods are used: 1. Auscultation of fetal heartbeats. The technique of auscultation during delivery: — calculation of cardiac beats is conducted for a full minute — every 15 min during the active phase and every 5 rnin during the second stage of delivery; — obligatory auscultation before and after a contraction or a labor pain; — if there are any auscultative violations of fetal heartbeats a cardiographic investigation is carried out. 2. Cardiotocography (CTG): — at fetal distress in the course of delivery CTG usually shows one or a couple of pathologic signs: tachycardia or bradycardia, per sistent rhythm monotony (recording width of 5 bpm and less), early, variable, and especially late decelerations with the amplitude bigger than 30 bpm. Unfavorable prognosis is also testified to by: — deceleration of fetal heart rate at the height of deceleration lower than 70 bpm irrespective of the type and amplitude of deceleration relative to heart rate; — transition of late or variable decelerations to persistent bradycardia. 3. Detection of meconium in the amniotic fluid at fetal sac rupture: — the presence of meconium in. the amniotic fluid in combination with pathological changes of fetal cardiac rate is an indication to urgent delivery at cranial presentation. Delivery management. 1. Avoid the dorsal position of the parturient woman. 2. Stop oxytocine introduction if it was administered earlier. 3. If the reason for pathological fetal cardiac rate is the mother's condition, appropriate treatment is to be conducted. 4. If the mother's condition is not the reason for pathological fetal cardiac rate, and fetal heart rate remains pathological during the last three contractions, one should carry out internal obstetric examination to determine the obstetric situation and find out possible reasons for fetal distress. 5. Fetal distress detection requires urgent delivery: — at the first stage of delivery — cesarean section; — at the second stage: • at cranial presentation — vacuum extraction or obstetric forceps; • at breech presentation — fetal extraction by the pelvic poll!. POSTNATAL ASPHYXIA Postnatal asphyxia is a syndrome accompanied by gas metabolism derangement with hypoxia, hypercapnia, and acidosis. The reasons for asphyxia may be classified in such a way: I. Central reasons, which are accompanied by the primary inhibition of the respiratory centers as a result of: a) fetal hypoxia; b) immaturity of the fetal nervous system; c) an injury of the fetal nervous system; d) pharmacological depressions. II. Peripheral reasons conditioned by the violation of oxygen supply to the fetal brain right after birth: a) airways obstruction resulting from the aspiration of the amniotic fluid, meconium, blood, fetal coat fragments; b) anatomical or functional immaturity of fetal lungs; c) dysfunction of the fetal cardiovascular system (congenital heart disease, hypovolemia, shock, delay of rearrangement of the fetal type of circulation into extrauterine); d) severe fetal anemia; e) congenital anomalies (choanal atresia, diaphragmatic hernia, etc.). Irrespective of the reasons for fetal hypoxia, they result in the decrease of oxygen level in the fetal blood, development of respiratory and metabolic acidosis, which increases the inhibition of respiratory centres, is accompanied by further derangement of pulmonary ventilation, augmenting of hemodynamic and metabolic disorders. Postnatal asphyxia most often results from fetal hypoxia. Therefore till the moment of birth there already exists overstrain or derangement of the adaptation mechanisms of the fetal organism in response to intrauterine hypoxia. The degree of asphyxia is evaluated by the Apgar score on the 1st and 5lh min after birth. However, if on the 5th min of life the assessment does not exceed 7 points, additional evaluations are to be conducted every 5 min. up to the 20th min of life (the final decision about the inefficiency of resuscitation measures), or to double assessment of 8 and more points. At the present stage the Apgar score is considered insufficiently informative in the prognosis of asphyxia development. More exact information, is given, by finding the so-called multiple organ insufficiency (MOI) caused by severe asphyxia at birth. The main MOI criteria are: violations of the indices of the cardiovascular, respiratory, nervous, homeostasis, urinary, and digestive systems, metabolic disorders (pHa 7.1 and less; BEa 15 micromole/L and less; the level of natrium in blood plasma < 130 micromole/L or > 150 micromole/L; the level of potassium in blood plasma < 3 micromole/L or >7 micromole/L; the level of glucose in blood, under the condition of complete parenteral nutrition, < 3.5 micromole/L or > 12 micromole/L. The newborns born, in asphyxia are treated in three stages: — the 1st — resuscitation; — the 2ni — intensive syndrome therapy; — the 3rd — rehabilitation. Preparation to neonatal resuscitation at a high degree of perinatal risk, and also at complicated delivery before the child's birth: one is to prepare the place and means for resuscitation, check the availability and perfect readiness of equipment and instruments, a set of medicaments, beforehand turn on the heating system of the resuscitation table and conditioning of the breathing gas. After evaluating the fetal condition the neonatal resuscitation department should be signalled about the necessity of turning on the couveuse. The problem of temperature rate requires special attention. The newborn supercools easily in the process of resuscitation. This is promoted by the fact that the newborn is not even wiped because of haste, and when the amniotic fluid evaporates, heat loss increases (about 540 calories are needed for the evaporation of 1 ml of water). Intravenous introduction of solutions, whose temperature is not controlled, also promotes the supercooling of the newborn. During artificial pulmonary ventilation (APV) there increases the organism's loss of not only water, but also heat. Resuscitation and intensive therapy without any special measures concerning the optimization of temperature rates is accompanied by the increase of peripheric vessels spasm, which increases the acidosis degree. At the present stage neonatal resuscitation is conducted by the ' neonatologist-resuscitator. The basic components of the resuscitation help to the newborn are known as the "ABC-steps" of resuscitation. A. Airways patency recovery (A — airways). B. Breathing stimulation or recovery (B — breathing). C. Circulation support (C — circulation). Resuscitation stages: 1. Provision of airways patency: a) to evacuate the content of the oral cavity and pharynx from (he moment the fetal head is born, not waiting for the shoulders birth; b) to continue the suction in the "draining" position after the Ictus is born; c) at massive aspiration the toilet is to be conducted using the guidance of a laryngoscope; d) the toilet is to be finished with the suction of stomach content to prevent recurrent aspiration after regurgitation or vomiting. 2. APV is conducted after the airways toilet if there is no indepen dent breathing during 40-60 sec after birth. Respiratory systems of different types are used for this. One is recommended to stick to the following rules when conducting APV: a) the newborn's head is given the position of flexion, for this it is the best to put the newborn on a special table with a movable head support, or to put a roll of diapers under the head; b) after APV beginning one is to conduct lungs auscultation and make sure of the full value of the toilet and efficiency of ventilation, which allows timely change of the APV regimen in case of need. In the newborns with pulmonary vessels hypoperfusion the APV in the regimen "active inspiration — active respiration" (with negative pressure on expiration), at excessive blood filling of the lungs and at continual atelectases the application of the APV with increased resistance on expiration of 5—6 mm Hg is administered; c) if masked APV is ineffective during 2—3 min, trachea intubation is performed under the guidance of a laryngoscope (at a severe stage of asphyxia, massive aspiration, and even at the presence of green amniotic fluid — right after birth), the correct position of the intratracheal tube is controlled auscultativcly; d) in case of need one carries out a repeated toilet of the airways and sanation of the tracheobronchial tree through the intratracheal tube (the catheter diameter must make 2/3 of the tube's diameter). If the aspirate is dense, isotonic natrium solution is previously introduced with a sterile syringe into the intratracheal tube and then evacuated; c) if APV through the intratracheal tube is ineffective, in immature newborns it is indicated to use the helium-oxygen mixture containing 30 % oxygen, during 10—15 inspirations; f) if the APV apparatus is absent or out of order, one must conduct iuou.th-to-mouth ventilation, being especially careful when exhaling air into the intratracheal tube. 3. Cardiac resuscitation. In case of apparent death, single heartbeats or even at heart rate < 60 bpm one must conduct closed-chest cardiac massage simultaneously with APV. The chest is pressed to the spine 2-3 times with the tips of two fingers in such a way that the recess makes 1 cm. if cardiac function is not renewed, 0.2 ml of 0.1 % adrenaline hydrochloride solution is stream introduced into the umbilical vein, 3-5 mg of 10 % glucose solution per kg of body weight, 1 —2 ml of 10 % calcium gluconate solution, glucocorticoids (10 mg/kg of body weight or hydrocortisone 4 mg/kg — prednisolone). If there is no effect, 0.2 ml of 0.1 % adrenaline solution and 1— 2 ml of 4 % sodium bicarbonate solution are introduced into the cardial cavity, cardiac massage is continued. It is expedient to conduct APV with cardiac massage during 10 min. 4. Correction of volemic and metabolic disorders. Disorders in the newborn period Preterm birth Infants born significantly before term usually require neonatal care until around the expected date of delivery. Following the introduction of surfactant coupled with the widespread use of antenatal corticosteroids in the mid-90s mortality rates for these infants fell significantly although in the smallest the risks of death remained high (Fig. 11.1). Rates in the twenty-first century remain similar to those shown. Mortality in extremely preterm babies can be significantly reduced if hypothermia is prevented at birth; this is only possible if the delivery room is maintained at an appropriate temperature. Most survivors do not sufferlong-ter m disability, but in infants of less than 28 weeks gestation some 20% suffer neurodevelopmental impairment. The stress on parents and family of having a baby who undergoes intensive care can be immense. They have to suffer prolonged uncertainly about the infant’s survival as well as a loss of control overtheirbaby’s and their own lives. Careful preparation of parents, with visits to the intensive care unit and meetings with unit staff may help, but the difficulties forfamilies in this situation should not be underestimated. Respiratory disorders Abnormal breathing is a common presentation of many illnesses in the newborn period. Intermittent or periodic breathing is common and not usually significant. However, a respiratory rate persistently above 60 breaths/min needs further investigation, as do periods of apnoea lasting more than a few seconds, especially if associated with cyanosis and bradycardia. Tachypnoea with recession and nasal flaring is frequently the presentation of respiratory or cardiac disorders, while apnoea may be the presentation of a great many disorders such as septicaemia, meningitis, gastrointestinal obstruction or heart disease. SURFACTANT DEFICIENCY The respiratory distress syndrome caused by inadequate surfactant production is mainly a disease of the preterm infant. However, it can occur in term infants, particularly those of diabetic mothers or after caesarean section without labour. Affected infantsmayrequiremechanical ventilation and intensive care. The classical clinical presentation is an infant with tachypnoea, subcostal and intercostal recession and nasal flaring which becomes progressively worse over the first 60 h after birth, and a chest X-ray showing a ground glass appearance with air bronchograms. It can be associated with pneumothorax, bronchopulmonary dysplasia (BPD) and intracerebral haemorrhage although in more mature infants it normally resolves without sequelae. The combined use of antenatal corticosteroids and surfactant modify the illness, improving survival and reducing the rates of complication such as pneumothorax and intracerebral haemorrhage but have little effect on reducing the incidence of BPD. CONGENITAL PNEUMONIA Congenital pneumonia is a relatively common problem associated with a variety of microorganisms. The infant presents with respiratory distress and a chest X-ray shows patchy inconsistent shadowing. Treatment is with antibiotics and intensive care as required. MECONIUM ASPIRATION Inhalation of meconium before or during delivery can be an extremely severe problem if pulmonary hypertension with reduced lung perfusion and severe hypoxaemia develop. Meconium may block large and/or small airways and lead to a ventilatory deficit. Although meconium aspiration may be apparent at birth, severe disease may present an hour or more laterand it is important that babies suspected of having aspirated are carefully observed. Treatment of meconium aspiration complicated pulmonary hypertension requires expert intensive care. Early surfactant administration may be beneficial, high frequency oscillatory ventilation and the administration of nitric oxide reduce mortality. When other measures fail extracorporeal membrane oxygenation should be considered. TRANSIENT TACHYPNOEA OF THE NEWBORN Transient tachypnoea of the newborn is due to delayed reabsorption of lung liquid which leads to a moderate degree of intracostal recession and tachypnoea. In the preterm infant this can lead to marked respiratory distress, but in a term baby needing high inspired oxygen concentrations other causes of respiratory distress should be excluded. BRONCHOPULMONARY DYSPLASIA This is a chronic condition affecting up to 50% of infants born at 26 weeks or less. Prematuredelivery, pre-and postnatal inflammation and infection, ventilation, oxygen and poor nutrition are among the many factors contributing to the development and persistence of BPD. The underlying problem is an arrest in alveolar and peripheral vascular development. The severity is variable ranging from the need forsupplementar y oxygen forsever al weeks to prolonged respiratory support with a ventilator or continuous positive airways pressure and death. A small proportion of babies are discharged home on supplementary oxygen; most outgrow the need by 12 months of age. All babies born prematurely have an increased risk of respiratory illness within the first few years of life. This is increased in the group with BPD and respiratory problems may persist into adult life. Cardiac disorders Some form of congenital heart disease affects between 7 and 9 per1000 live births of whom approximately one quarter will present in the newborn period. Fetal anomaly ultrasound can detect many lesions; antenatally, however, some are more difficult to diagnose. Cardiac disease in the newborn baby presents in five main ways: CYANOSIS DUE TO REDUCED PULMONARY BLOOD FLOW The commonest causes are transposition of the great arteries (TGA), right to left shunts such as Tetralogy of Fallot and pulmonary or tricuspid atresia. Administration of 100% oxygen fails to increase arterial saturation and a chest X-ray may show oligaemia. Tachypneoa may occur; however, respiratory distress is often not a prominent feature of the presentation whereas cyanosis may be profound. A measurement of blood gases is mandatory both to the diagnosis and as a measure of the baby’s condition: metabolic acidosis is an ominous sign. Forthose presenting in the neonatal period immediate treatment is required to prevent the ductus arterious from closing with transfer to a specialist paediatric cardiac centre. CARDIORESPIRATORY DISTRESS DUE TO INCREASED PULMONARY BLOOD FLOW Left to right shunting though septal defects with a consequent increase in pulmonary blood flow decreases the compliance of the lung leading to chest recession and tachypnoea. The homeostatic response to this shunt is fluid retention, leading to congestive cardiac failure with a large liver and oedema. Infants with large left to right shunts are not particularly hypoxaemic except when cardiac failure is severe. The commonest cause of large left to right shunts are large ventricular septal defect, atrioventricular septal defects and patent ductus arterious. CYANOSIS AND CARDIORESPIRATORY DISTRESS Infants inwhommixing between systemic and pulmonary circulations is impaired can present with breathlessness and cyanosis. Complex conditions such as transposition of the great arteries may lead to this presentation. SHOCK SYNDROME DUE TO LOW CARDIAC OUTPUT The clinical picture of shock is a desperately ill infant with generalized pallor, cyanosis, cool peripheries and weak or absent pulses. Breathing is laboured or gasping, and the infant is hypotonic. Neonatal shock is usually due to major sepsis, significant blood loss ormajorinter ruption to the circulation such as hypoplastic left heart syndrome, severe coarctation of the aorta or complex cardiac defects. Shock can also be part of the later natural history of other cardiac defects. THE ASYMPTOMATIC MURMUR Murmurs are common in newborn infants and are frequently innocent. A low-amplitude-ejection systolic murmur is audible in some 60% of normal newborn infants. It is normally best heard over the pulmonary area and may be due to a ductus arterious that has not fully closed or a pulmonary artery branch flow murmur which disappears before 6 months of age. Innocent murmurs are systolic, short, localized and may change. Infants may develop murmurs when unwell, because of increased cardiac output or reopening of the ductus arterious. Other causes of asymptomatic murmurs in the newborn period include septal defects, aortic or pulmonary stenosis and Tetralogy of Fallot. A thorough search for other signs of cardiac disease should be made and an expert opinion arranged where appropriate. It is important to remember that the mention of a heart murmur can strike panic into even the calmest of parents and the situation needs to be handled with great tact. Rapid definitive diagnosis by echocardiography is the mainstay of successful management. Neurological disorders NEONATAL ENCEPHALOPATHY Neonatal encephalopathy can be caused by hypoxia ischaemia due to birth asphyxia but also by other conditions including metabolic disorders and infections. These conditions should be excluded before a confident diagnosis of hypoxic ischaemic encephalopathy due to birth asphyxia can be accepted. Hypoxia-ischaemia followed by resuscitation may lead to apparent recovery followed by inexorable deterioration beginning 6–8 h later and ending in severe cerebral injury. Consequently, it is frequently difficult to determine the prognosis soon after birth on clinical grounds alone. However, if asphyxia is severe or happened some time before delivery the infant will not develop spontaneous breathing; therefore, if despite advance life support there is no sign of spontaneous breathing 20 min after birth the outcome is extremely poor. Hypoxic ischaemic encephalopathy is graded clinically using clinical signs. Infants with grade 1 encephalopathy have a very good prognosis whereas infants with Grade 3 almost all die or are severely impaired. About half the infants with Grade 2 have severe neurodevelopmental impairment. Unfortunately a large number of infants at risk fall into Grade 2, limiting the utility of the system. If asphyxia is suspected, further investigation is required, preferably by paediatricians specialized in neonatal neurology and with access to sophisticated equipment such as electrophysiology, magnetic resonance imaging or magnetic resonance spectroscopy. Diagnosis and an accurate guide to prognosis can then be obtained. CEREBRAL PALSY Cerebral palsy is a non-progressive brain syndrome which may not be apparent until after the first year of life and which cannot be confidently diagnosed at birth. Population based studies have shown that about 20% of all cases of cerebral palsy are due to birth asphyxia in the term infant, approximately one third are associated with preterm birth, and the remainder have no obvious fetal or perinatal antecedent. CONVULSIONS Convulsions occurring just after delivery in term infants may be due to hypoxic ischaemic encephalopathy, metabolic disorders, infections, hypoglycaemia, hypocalcaemia, hypomagnesaemia or pyr idoxine deficiency. Many otherwise idiopathic fits are caused by focal cerebral infarction, which have a much better prognosis than generalized hypoxic ischaemic injury but are difficult to diagnose without magnetic resonance imaging. BRAIN INJURY IN PRETERM INFANTS Preterm infants are at high risk of cerebral injury and approximately10%of infants born pretermdevelop significant neurodevelopmental impairment and another 10% have minorneur ological lesions: two classical lesions which occurin preterm infants. First, intracerebral haemorrhage may affect only the germinal layers or ventricles in which case the prognosis is good; however, haemorrhage into the brain parenchyma is caused by haemorrhagic infarction and this is associated with neurodevelopmental impairment. Second, in periventricular leucomalacia there is a general loss of white matter, sometimes with cavitation. Whereas haemorrhagic parenchymal infarctions can be usually seen by cerebral ultrasonography, periventricularleucomalacia is difficult to see and is probably under diagnosed. Both these conditions seem to be becoming less common than a more subtle loss of cerebral matter; this may present as dilated cerebral ventricles on cerebral ultrasonography but is often only apparent with magnetic resonance imaging. The aetiology of this condition is poorly understood, the extremely preterm infant seems to be most at risk. The usefulness of cerebral ultrasonography alone to predict neurological prognosis in extremely preterm infants is therefore limited. The more mature preterm infants with normal ultrasound scans at discharge from intensive care have a very low risk of neurodevelopmental impairment whereas those with definable loss of brain tissue from whatevercause have a greaterthan 50% chance of long-term impairment. BRACHIAL PLEXUS INJURY Brachial plexus injury occurs in 0.4–2.5 per 1000 live births. The commonest type, Erb’s palsy, involves C5 and 6 nerve roots. The incidence has not declined over the past few decades; however, the prognosis for recovery, has improved with full recovery expected in the majority of babies with Erb’s palsy. Injury to the brachial plexus results in the characteristic waiters tip position, a fracture to the clavical may also be present. Careful neurological examination is needed to determine the level of the lesion as this affects the prognosis for recovery of function; an associated Horner’s syndrome is a bad prognostic sign. Effects of maternal drug ingestion Infants of motherswhotake drugs such as opiates, cocaine, amphetamines, barbiturates, benzodiazepines and some othermedical drugs may develop a withdrawal syndrome with irritability, poor feeding, apnoea and fits. The babies of mothers who have high alcohol or nicotine intake may also exhibit withdrawal. Wherever possible the mother and baby should be kept together; in many cases breastfeeding in not contraindicated. If a history of maternal drug abuse was known antenatally a plan of management can be agreed before birth and a referral to the social work team may be appropriate. Management of a baby at risk of drug withdrawal involves careful observation and skilled nursing. If withdrawal is severe treatment with opiates may be required. Naloxone should never be given to infants at risk of opiate withdrawal as it can provoke convulsions. Many labourwar ds no longerstock naloxone forfearit will be given inadvertently to an infant of a substance-abusing mother. Jaundice Jaundice beginning in the first 24 h after birth is pathological. It is usually unconjugated and the commonest cause are haemolytic anaemia or infection. Jaundice beginning on days 2–5 is commonly physiological, but unconjugate hyperbilirubinaemia may have many causes including haemolytic disease, ABO incompatability and G-6-P deficiency Guidelines forthe management of neonatal jaundice are derived from the belief that bilirubin levels greate than 340 mmol/l in term infants can cause deafness an kernicterus. This is based on data established when kernicteru due to severe rhesus disease was common bu it has not been demonstrated that 340 mmol/l is the critica level for nervous system injury in other conditions. It I generally believed that in preterm infants critical levels ar lower than this, especially if the infants have intercurren illness, while at term higher concentrations may be tolerate without neurological deficit provided the infant does not have additional pathology such as infection oracidosis Many authorities now advocate a more relaxed vie of neonatal jaundice in a well, term infant, but haemolyti jaundice and jaundice in the sick or preterminfant should always be treated aggressively. Failure to control bilirubin levels by phototherapy should lead to urgent exchange transfusion. Conjugated hyperbilirubinaemia signifies liver disease and requires urgent specialist investigation. These infants maybe at risk of complications such as significant bleeding and neurological damage. Hypoglycaemia Blood glucose concentration is only one measure available of metabolic fuel and in term infants who are able to produce and utilize ketones, it is not easy to define an unequivocal level at which the baby is at risk of the neurological sequelae of hypoglycaemia. Authorities differ, but a pragmatic solution is to consider term infants with two consecutive blood glucose levels below 2 mmol/l ora single blood glucose level below 1 mmol/l in need of intervention. The blood glucose must be measured using an accurate device as commercial test strips are not adequate formaking the diagnosis of hypoglycaemia. Conditions commonly associated with transient low blood glucose are hypothermia, infection, prematurity, intrauterine growth retardation and maternal diabetes. Some infants develop transient hyperinsulinaemia, particularly infants of diabetic mothers with poor antenatal control or those with severe rhesus disease. Rare causes include the Beckwith-Wiedemann syndrome and metabolic defects such as cortisol deficiency, galactosaemia and otherenzyme defects of glycogenolysis, gluconeogenesis orfatty acid β oxidation. Preterminfants are much less able to mount a ketotic response and hypoglycaemia should be treated promptly. Treatment is initially to give calories in the form of milk oras intravenous glucose infusion. Rapid bolus injections of concentrated glucose solutions (20–50%) are not recommended. If hypoglycaemia persists investigations, including insulin measurements, are required. Infections Newborn infants are particularly prone to perinatal infection; risk factors include lowbirthweight infants, prolonged ruptured membranes, maternal fever or chorioamnionitis. Iatrogenic infection is problematic for those undergoing intensive care; the presence of indwelling cannulae, central venous lines and invasive mechanical ventilation increase the risk. Organisms responsible for later neonatal infection frequently come from the skin or gut. Breastfeeding helps promote normal gut flora and reduces the risk of acquired neonatal infections. Adherence to good hand-washing practices by all staff, parents and visitors can significantly reduce the risk of acquired infection. SEPTICAEMIA The signs of systemic sepsis are non-specific. Infants may present with apnoea, bradycardia or cyanotic episodes; is a common association. They may be lethargic and hypotonic and they are hyper or hypothermic. Sepsis frequently presents as a metabolic acidosis or shock and occasionally causes petechial skin rash or severe jaundice. Organisms which commonly cause infection in the newborn period are group B streptococci, and gram-negatives such as Escherichia coli orKlebsiella. The prolonged user multiple changes of antibiotics in the antenatal period may increase the risk of infection with resistant organisms. Rapid treatment with antibiotics, immediate resuscitation and, frequently, mechanical ventilation is required. Investigations include chest X-ray, blood cultures, urine culture, and examination and culture of the placenta. A lumbar puncture is performed once the baby is stable and will tolerate the procedure. The mortality of infants who develop septicaemia in the neonatal period is high with a significant number of survivors developing subsequent impairment. GROUP B STREPTOCOCCUS INFECTION Mortality due to maternal colonization by Group B streptococcus (GBS) is reduced by antibiotic therapy to the Mother during labour and early treatment of infants with evidence of infection. About 2% of infants of colonized mothers develop infections, and 70% of these manIFEST risk factors at birth such as preterm labour, prolonged rupture of the membranes or meconium stained liquor. Urgent antibiotic therapy is indicated for these infants. Well infants shown by surface cultures to be colonized, do not require treatment. Recurrent GBS infection can occurbut more commonly GBS infection can occurlater in infancy when meningitis is the presenting problem. MENINGITIS Signs of meningitis in newborn infants are non-specific with a bulging fontanelle; opisthotonos and seizures occurlate in the disease. Meningitis usually presents as septicaemia and can be complicated by cerebral oedema, cerebral infarction, brain abscess or deafness. Common causal organisms are GBS and E. coli. Listeria monocytogenes is a rare cause of perinatal infection in the United Kingdom. URINARY TRACT INFECTION Urinary tract infectionsmaypresent as jaundice, vomiting, poorfeeding orsepticaemia. The main cause is believed to be spread of blood-borne organisms to the kidney during septicaemia. Further investigation is essential as 35–50% are associated with urinary tract abnormalities such as vesico-ureteric reflux or ureterocele. Breastfeeding offers a significant degree of protection. EYE INFECTION The majority of sticky eyes are not infected but are due to a blocked nasolacrimal duct. In the absence of conjunctival redness orswelling investigation forinfection and treatment with topical antibiotics is not required. Simple measures such as cleaning with boiled water and lacrimal duct massage suffice with symptoms usually resolving in 3–6 months. Neonatal conjunctivitis can be caused by such organisms as Staphylococcus aureus,Chlamydia trachomatis, Haemophlus influenzae,Str eptococcus pneumoniae and Neisseria gonorrhoeae. Gonococcal ophthalmia usually presents within 24 h of delivery with profuse purulent conjunctival discharge and immediate diagnosis and treatment (systemic and topical) is required to prevent damage to the cornea. Chlamydial ophthalmia which is now among the commonest causes of neonatal conjunctivitis presents between 5 and 12 days postnatal age; some babies infected as neonates will develop chlamydial pneumonia laterin infancy. Corneal scarring is rare; 14 days systemic and topical treatment is required. The identification of either N. gonorrhoeae or chlamydia in the baby requires referral of motherand hersexual partnerforinvestigation and treatment. SKIN INFECTION Simple hygienic methods such as bathing, hand washing and routine umbilical cord care can prevent many skin infections. The infant’s skin is vulnerable to infection by Staphylococci, which usually leads to small pustules or lesions but can also cause scalded skin syndrome with severe exfoliation. Staphylococcal infections should therefore be treated with antibiotics after appropriate cultures have been taken. Streptococci can also cause skin infection and both may cause systemic illness. Infection of the umbilical cord is commonly limited to periumbilical redness with a small amount of discharge. The presence of oedema indicating cellulitis can occasionally lead to complications such as spreading cellulites of the abdominal wall, fasciitis and septicaemia and requires treatment with systemic antibiotics. Candidiasis usually presents after the first week of life with napkin dermatitis with or without oral thrush. Topical and oral treatment is required to prevent the candidiasis returning as the gut is colonized with candidia. Maternal nipple candidial infection can occur in breastfeeding mothers. TUBERCULOSIS Tuberculosis is a re-emergent disease and many hospitals now offerBacille Calmette-Guйrin (BCG) immunization to newborn infants. Infants born to mothers infected with active tuberculosis should be vaccinated with isoniazidresistantBCGvaccine and kept with the mother while both receive treatment with appropriate drugs. Breastfeeding should be encouraged. Expert advice on drug therapy is advisable as patterns of antibiotic susceptibility change overtime. TETANUS Neonatal tetanus due to infection of the umbilical stump by Clostridium tetanii is the result of poor hygiene and is a distressing and severe condition with extremely high mortality. Opisthotonus and muscle spasms of the jaw and limbs are presenting features and can appear very rapidly after birth. Prevention centres on maternal vaccination during pregnancy and education to improve hygiene and change of local cultural practices. Gastrointestinal disorders OESOPHAGEAL ATRESIA OR TRACHEO-OESOPHAGEAL FISTULA These conditions should be suspected when there is polyhydramnios or excessive mucous from the mouth at birth. The baby may show rapid onset of respiratory stress and cyanosis particularly after the first feed. X-ray confirms the diagnosis, the naso- oror ogastric tube does not pass into the stomach. A large bore nasogastric tube should be placed in the oesophageal pouch, constant suction and regular aspiration help prevent aspiration pneumonia. Associated congenital anomalies occurin 50% or more of infants. Surgery involves division of the fistula and oesophageal repair; if primary anastomosis is not possible lengthened procedures are required before later oesophageal repair. Common long-term complications are gastro-oesophageal reflux and anastomotic stricture formation both of which may require further surgical treatment and long-term medication. Survival is usually determined by the severity of associated congenital anomalies and not the defect itself. DIAPHRAGMATIC HERNIA Herniation of the abdominal contents into the hemithorax leads to severe respiratory difficulties with persistent pulmonary hypertension. Most cases present with respiratory distress and cyanosis at birth. Essential early management is the passage of a large bore nasogastric tube into the stomach to prevent gaseous distension, ventilation and rapid transfer to intensive care. All these infants require tertiary level intensive care, with access to sophisticated mechanical ventilation and modern vasodilator therapy such as nitric oxide. Surgery is delayed until the infant’s respiratory status has been stabilized. Survival depends on the degree of underlying pulmonary hypoplasia and the presence of associated congenital anomalies such as cardiac defects. Long-term complications include persistent gastro-oesophageal reflux and respiratory problem; neurodevelopmental problems can develop if neonatal hypoxia was severe. ABDOMINAL WALL DEFECTS Exopmhalos, in which part or all of the intestine and abdominal organs are in a peritoneal sack outside the abdomen, should be differentiated from gastroschisis where a congenital defect of the abdominal wall allows herniation of the abdominal contents without a peritoneal sac. The former is frequently associated with other congenital defects, while the latter is not. Urgent surgery is required if the amniotic sac has broken and for gastroschisis; immediate management is to wrap the abdominal contents in a plastic wrapper taking care not to twist the bowel and disrupt its vascular supply. This should help prevent hypovalaemia due to fluid loss from the exposed bowel. A large bore nasogastric tube is passed and the baby’s circulatory status constantly assessed. Hypovalaemia orexcessive nasogastric output should be treated with 20 ml/kg 0.9% sodium chloride bolus intravenous infusions. The risk of hypothermia is high unless good thermal management is present from birth. Primary repair is not always possible if the abdominal cavity is not large enough to accommodate all the contents; a silo made of sterile prosthetic material is attached to the abdominal wall and the contents gradually reduced over 7–10 days. Outcomes are worse for those requiring silo treatment as infected complications are high. The long-term outcome for most with exopmhalos is determined by the presence of associated congenital anomalies. In gastroschisis 90%ormor e now survive. However, theirpostnatal course is often protracted and parenteral nutrition may be required for several weeks with its risks and complications. In addition bowel atresias and necrotizing enterocolitis may develop. INTESTINAL OBSTRUCTION Highintestinal obstructions usually present with vomiting whichmaybe bile stained, and this ominous signdemands urgent investigation. Plain X-ray film of the abdomen can confirm the presence of obstruction by showing a lack of air in the lower gut or a sign such as the ‘double bubble’ of duodenal atresia. Hypertropic pyloric stenosis does not usually present until 2–6 weeks of age. Lower intestinal obstruction usually presents as failure to pass meconium within 24 h followed by abdominal distension with orwithout vomiting. Causes include Hirshprung’s disease, meconium ileus due to cystic fibrosis low bowel atresia or hypoplasia and imperforate anus. Ameconium plug can sometimes mimic obstruction especially in preterm infants. NEONATAL NECROTIZING ENTEROCOLITIS This poorly understood inflammatory condition is primarily a condition of preterminfantsandthose with congenital heart disease. It presents as an acute abdomen in the days or weeks after birth and varies in severity from mild to fatal. Diagnosis is clinical, aided by characteristic X-ray changes such as airin the bowel wall orbiliar y tree. Treatment is conservative with cessation of enteral feeding and with antibiotics orsur gery. Common queries from parents Many minor alterations to physiology cause alarm to parents. Some common questions and responses to them are outlined in Table 11.6 and in the absence of disease, reassurance is all that is required. It is wise to read your unit’s breastfeeding policy so as not to contradict the advice given by midwives and lactation consultants. Advanced life support If mask ventilation fails to produce an adequate heart rate check again forevidence of upperair way obstruction and aspirate the nasal passages and nasopharynx. Meconium present in the trachea should have been aspirated under direct vision using a laryngoscope before ventilation, but this may need repeating. If clearing of the airway and reventilation fails to produce a normal heart rate, endotracheal intubation is required. This technique is not difficult but requires practice and carries a considerable danger in inexperienced hands: the endotracheal tube will enter the oesophagus easily and significantly inhibi ventilation. If an infant does not rapidly improve after attempted endotracheal intubation, there is presumptive evidence of the tube being in the oesophagus. It should be removed and intubation repeated. If there is doubt it may be safer to concentrate on bag and mask ventilation while awaiting skilled assistance. Once the endotracheal tube is placed, auscultate the chest overboth lungs to ascertain that breath sounds are equal. Inequality implies that the tube has been inserted too far and entered one lung, but could also suggest majorpr oblems such as pneumothorax orcongenital diaphragmatic hernia. Endotracheal intubation secures access for mechanical ventilation. Initial ventilation should include an inspiratory time of approximately 1 s todistend collapsed alveoli, and peak pressures sufficient to visibly move the chest. Once the alveoli are expanded less pressure is required. Thus the first breaths may require peak pressures of 30 cm of waterormor e in term babies, whereas afterthis it is usually possible to ventilate the lungs with pressures of approximately half this, and a respiratory time of 0.5 s at a rate of 40 breaths/min. If there is evidence or presumption of surfactant deficiency, exogenous surfactant shouldbe administered early. Effective ventilation is enough to resuscitate most infants and only rarely is cardiac massage or the administration of blood because of bleeding required. On very rare occasions, endotracheal adrenaline may need to be administered for persistent bradycardia and if this fails intravenous adrenaline may be given. It is no longer good practice to administer sodium bicarbonate intravenously to infants unless blood gases are measured or circulatory failure is very prolonged. Most low-risk infants who require resuscitation can be extubated within a few minutes and can usually be nursed by their mothers as long as (1) there is no specific problem such as meconium aspiration, prematurity or a history of infection and (2) adequate observation can be maintained. Infants who cannot be extubated successfully in this time or who continue to have respiratory problems require admission to a neonatal unit. Students must know: 1. Etyology and pathogenesis of placental disorders 2. Principles of diagnostics, treatment and management of women with placental disorders. 3. Clinical picture, diagnosis and therapy of asphyxia of newborn, the most common neonatal diseases. Students should be able: 1. To evaluate the state of the fetus by the ultrasound examination an cardiotocography. 2. Principles of organization of the fetal department in the case fetal pathology. 3. Laboratory establishment of the diagnosis of placental insufficiency. 4. To prescribe the laboratory methods of examination. 5. To determine previous diagnosis of the disease of the newborn. 6. To perform emergency procedures of neonatal resuscitation. References: 1. Danforth's Obstetrics and gynaecology. - Seventh edition.- 1994. - P. 560- 590| 2. Obstetrics and gynaecology. Williams & Wilkins Waverly Company. - Thin Edition.1998. -P. 157-179. 3. Basic Gynecoiogy and Obstetrics. - Norman F. Gant, F. Gary Cunningham. 1993. - P. 362-371. 4. Obstetrics.Edited by Prof. I. Ventskivska. – Kyiv. – 2008.