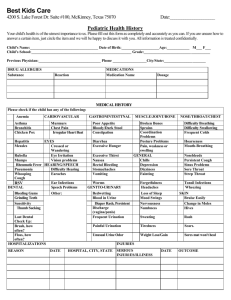
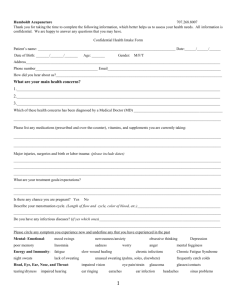
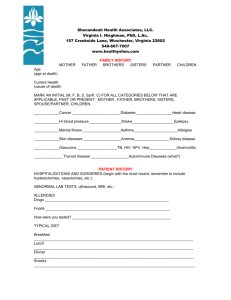
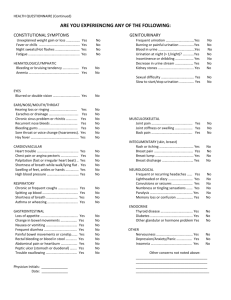
Patient Intake Form - Medical History & Health Details
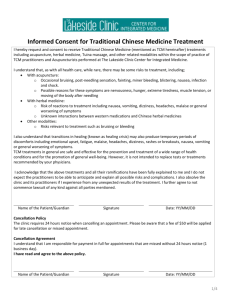
advertisement

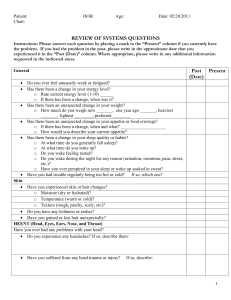
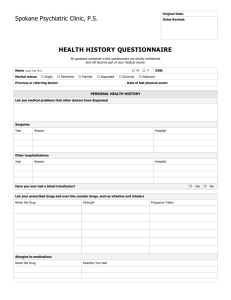
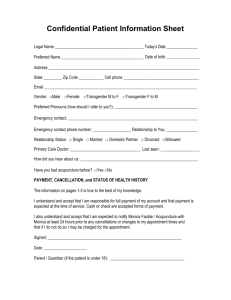
Today’s Date____/____/____ Please Print D M Y Name:__________________________________________________ Date of birth____/____/____ Age:____ (Last) (First) D M Y Address: __________________________________________________________________________________ City: _____________________________ Province: _______________________Postal code: ______________ Tel: ________________Work:________________ Cell: ________________ Email: _______________________________ Would you like to receive email reminders? ________________ Occupation: _______________________ Gender: Male____ Female___ Height: _______ Weight: _____lbs Relationship status: Single: ___ Common-law: ___ Married: ___ Separated: ___ Divorced: ___ Widowed: ___ Emergency Contact Person: ________________________ Relationship: _______________Tel:_____________ Patient Medical History Check any you have had in the past: ___Diabetes ___High/low blood pressure ___Seizures ___Childhood illnesses ___Accident/trauma ___Hepatitis ___HIV Other: ______________ ___Cancer ___Bleeding Tendency ___Nervous Disorder ___Alcoholism ___Drug Addictions ___Mental illness ___Birth trauma ___Heart Disease ___Asthma ___Thyroid disease ___Epilepsy ___Allergies ___CVA (stroke) ___Fibromyalgia ___Cancer ___Asthma ___Epilepsy ___Allergies ___CVA (stroke) ___Heart Disease ___Seizures ___Herpes ___Hepatitis A/B/C other: ______________ Family Medical History ___Diabetes ___High blood pressure ___Alcoholism ___Drug Addictions ___Mental illness Are you currently taking any medication? Yes___ No___ If yes please list medications and for what conditions 1._______________________________________ 4._________________________________ 2._______________________________________ 5._________________________________ 3._______________________________________ 6._________________________________ Are you currently taking any supplements? Yes___ No___. Please list: ________________________________________________________________________________ What medical diagnosis have you received for this condition: ________________________________________ Are you seeking other alternative therapies for your condition (if yes please list): ________________________ _________________________________________________________________________________________ Is this your first experience in Acupuncture? _____________________________________________________ Habits Please indicate usage per day or per week: Cigarettes _________________ per ______ Drugs _________________ per ______ Main problem you would like help with: _______________________________________________________ __________________________________________________________________________________________ When did the problem begin (be specific): _______________________________________________________ To what extent does the problem interfere with your daily activity (work, exercise, sleep, sex, etc.)? __________________________________________________________________________________________ __________________________________________________________________________________________ Any significant traumas? _____________________________________________________________________ Rate you Energy level on a scale of 1 to 10 (10 being the worst): _________ What time of day is your energy: Highest? ______________________ Lowest? _________________________ Do you fatigue easily? _______________________________________________________________________ On the following drawings, please clearly mark any areas of pain. Musculoskeletal ___Joint pain/disorder ___Sore muscles ___Hip pain ___Difficulty walking ___Neck/shoulder pain ___Upper back pain ___Lower back pain ___Rib pain What is the frequency of discomfort: ___________________________________________________ Rate you pain level on a scale of 1-10. Circle one. Less Pain 1 2 3 4 5 6 7 Minimal slight moderate 8 More Pain 9 10 severe Do you suffer from any of the following? Please check all the following that pertain to you. General ___ Fatigue ___ Recent weight loss/gain ___Easy bruising ___ Cold hands & feet ___Cold nose ___Cold low back ___Cold limbs ___Chills/fever ___Itching ___Rashes ___acne ___Eczema/ psoriasis ___Dry skin ___Dry nails ___Brittle nails Other: __________________________________________________________________________ Emotions & Sleep ___Anxiety/worry ___Irritability/anger ___Depression ___Panic attacks ___Poor memory ___Mood swings Other: ______________________________________________________________ Sleep: ___Fall asleep easily ___Lie in bed with eyes open ___Wake repeatedly ___Wake frequently to urinate ___Wake up not feeling rested ___Nightmares or frightening dreams ___Need medication or supplements to fall asleep ___Wake at specific times ___Vivid dreams Eyes, Ears, Nose, Throat & Head ___Blurred vision ___Spots or floaters ___Dry eyes ___Itchy eyes Other: _______________________________________________ Ringing in ears: High pitch____ Low pitch___ ___Sinus infection ___Post-nasal drip ___Frequent sore throat ___Frequent colds ___Nosebleed ___Nasal congestion ___TMJ ___Difficultly on inhalation ___Chronic cough ___ Feeling of a lump in the throat ___Coughing up phlegm ___Shortness of breath ___Tightness in chest ___Heaviness of the chest ___Palpitations Other: _________________________________________________________________________ ___Headaches ___Migraines Frequency? _____ Duration of attacks? __________ Character of pain: ___Feels full/pressure ___ Dull/achy ___Throbs ___Visual aura ___Stiff neck ___Dizziness/vertigo Other: _______________________________________________ ___hair loss ___premature graying Gastrointestinal ___Extreme appetite ___No appetite Cravings for: ___Sugar ___Salt ___Tired after eating ___Gas ___Sour ___Bloating ___Nausea ___Reduced appetite ___Carbs ___Acid reflux ___Belching ___Heart burn Bowl movements: How often? ______time(s) day/week Color of Stool: ________________________ ___Diarrhea ___Constipation ___Loose stools ___Dry hard stools ___Alternate between soft to hard stools ___Early morning diarrhea ___Blood in stool ___Mucus in stool ___Pain/cramping Other: _______________________________________ Fluid Metabolism & Urination How many glasses per day do you drink of the following?: Water___ Pop___ Coffee___ Tea___ Alcohol___ What temperature of beverage do you prefer? Hot___ Cold___ Room temperature___ How would you describe your thirst? Thirsty often___ Have to force myself to drink___ Never thirsty___ Can’t quench my thirst___ Normal___ Sweating: ___Day time sweating ___Night time sweating ___Spontaneous sweating ___Related to exertion Urination: How often? ________times/day ___Cloudy urine ___Burning on urination ___Strong smelling urine ___Frequent urination ___Urgent urination ___Blood in urine ___Wake to urinate Other: _____________________________________________________________________