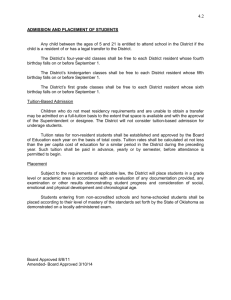
6.1 Introduction to public records
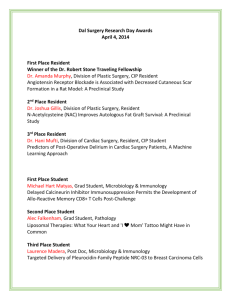
advertisement

Residential Services Practice Manual 3rd Edition – Part 6 In this section 6 Records and procedures 6.1 Introduction to public records 6.1.1 Records kept by residential services 6.1.2 Client Relationship Information System (CRIS) 6.1.3 Personal information privacy and access 6.1.4 Freedom of information 6.1.5 Storing, maintaining, moving and archiving files 6.2 Accountability of money 6.3 Handling funds in respite services 6.4 Critical client incidents and non-critical client events 6.5 Damage caused by people living in residential services 6.6 Missing people 6.7 Responding to physical and sexual assault 6.8 When a person dies July 2013 6.9 Wills and deceased estates re-issued RSPM application to service type Each instruction has service type and instruction application codes to assist to identify how the specific instruction applies to supported accommodation by service type. Service type: FBR facility based respite GH group homes STJ short term justice LTR long term rehabilitation program I Sandhurst and Colanda RTF residential treatment facility (DFATS) Instruction application: Y instruction applies in full N instruction does not apply to service type P Partial application. Service required to implement principle of instruction but service not generally directly responsible for planning, monitoring and reviewing components of instruction LD Locally determined based on client plans, service model and protocols. Applicable to STJ, LTR and RTF only Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – Part 6 Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1-1 6.1 Introduction to public records Issued: August 2012 Applies to all Contents What are public records? Why are public records important? Public records in residential services Legislation and policy directs records management Standards for written records Resources What are public records? A public record is any record made or received by a public officer in the course of their duties. Records come in a variety of formats and media including: hardcopy documents emails computer files letters scanned documents web pages maps plans photographs. Disability Accommodation Services staff are public officers. A public officer includes anyone employed by any department, branch or office of the Government of Victoria including permanent, part-time and contracted staff. Why are public records important? Records demonstrate how the Department of Human Services is accountable for decisions and actions and how it complies with legal, financial and business requirements. Records provide proof of services provided to clients, business practices, communications, decisions and actions. Records generated in residential services are the collection of information necessary for Disability Services to provide evidence of the support which has been provided to residents. Public records in residential services In the course of a working day, all information which provides evidence of the work undertaken must be retained as a record. Records must be created whenever there is a requirement for accountability and evidence of decisions made and actions taken. The Accommodation Services File (ASF) is the public record of the support provided to a resident in a residential service. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1-2 Legislation and policy directs records management There are legal and policy requirements for government departments which places significant responsibility on all public officers. Based on these requirements, all records collected or received must be treated in accordance with the provisions of the legislation which governs practice and the department’s policy on records management. For disability services the following law and policy applies: Victorian Public Records Act 1973 Information Privacy Act 2000 Health Records Act 2001 Disability Act 2006. Evidence Act 2008 Freedom of Information Act 1982 Residential Services Practice Manual 2011 Department of Human Services Records Management Policy (10/001) Standards for written records The majority of records created are subject to the Freedom Of Information Act 1982, so all records must be: factual and non-judgmental legible logical and sequential signed and dated appropriately cross-referenced, for example, if a letter from an administrator is filed in the finance section of a person’s file, this should be noted in the daily communication record. Staff must not: use white-out to correct mistakes; mistakes must be crossed out with a line through the text and initialled archive or store documents in plastic sleeves which can cause printed information to deteriorate file faxes or documents on thermal paper as these deteriorate over time; these documents must be copied onto standard paper before filing use jargon. Avoid acronyms or abbreviations to ensure information is clear to any reader use abbreviations or nick-names of staff or residents. In addition: the use of red pen should be avoided as it may become illegible if it needs to be photocopied for a formal process, such as an investigation by police or the coroner. Resources DHS Business Support Records Management – policy, fact sheets and resources that describe requirements for records management. Available on the DHS Hub. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.1 – 1 6.1.1 Records kept by residential services Issued: August 2012 Applies to all Contents Overview Security of records within residential services Security of records taken to external appointments Portable data storage devices What are resident records? Electronic documents How are residents identified in the system? How do group homes get ASF’s How is the ASF used? What are operational records? How are operational records managed? Role of staff Role of supervisor and manager Resources Overview All documents and files created and used within residential services are known as records. The records kept in residential services relate to both residents and the general operation of the service site. The records required to be completed are specified in each part of this manual. Security of records within residential services Records must be securely kept in locked storage when not in use to ensure protection from: unauthorised access, see RSPM 6.1.3, 6.1.4 tampering damage or destruction Security of records taken to external appointments When information held on a resident’s file is required for an appointment outside of the residential service, for example, a specialist medical appointment, staff must ensure that the record is: in a secure non-transparent document envelope limited to only the specific information required for the appointment never saved to an unsecured portable data storage device. never transported loose or with information visible not left unattended in any place at any time kept with the staff member at all times. A note should be included in the diary or shift report, to identify what records have been removed from the residential services, and when they were returned. This should include the date and time the information was taken and returned. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.1 – 2 Portable data storage devices Portable data storage devices must only be used for resident records if they approved and provided by the Information management and technology units. These devices include: USB memory sticks personal digital assistants (PDA’s) such as palm pilot and Blackberry digital audio players such as iPods and MP3’s mobile phones and smart phones lap top computers removable storage media such as CDs and memory cards. Resident information must never be saved to staff members’ personal device under any circumstance. Where portable electronic storage devices such as a USB, may be required they must be requested via the manager to regional Information Technology services. The devices supplied will be encrypted to ensure that any information is secure and only able to be accessed with passwords or codes. Residents may use personal devices to store personal photo’s or other information and these are not subject to records management requirements. What are resident records? The official corporate file for resident records is the Accommodation Services File (ASF). Resident records include, based on resident support needs, but are not limited to: personal profile health support personal care person centred active support and daily routines support assessments and plans Critical Client Incident reports financial plans These records are documents that: describe support needs and services used by department clients keep a history of how support is provided to each person. Electronic documents Electronic documents include resident plans written on the computer, emails, scanned documents and photo’s. Saving documents to the residential service computer, is not part of the official client information management system like CRIS. Documents required to guide support, or that contain information about a resident (including emails), must be printed and placed in the relevant section of the ASF in accordance with the department’s records management policy. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.1 – 3 How are residents identified in the system? There are two official sources which keep client information. One is the Client Relationship Information System (CRIS), which allocates a number to every person who is registered for services with the department. This number forms the basis for all reference numbers relating to the client records and the services which they receive from the department. Residential services may not currently use or access CRIS however a resident’s CRIS number must be on all files to ensure records can be registered to the right person in the Total Records Information Management (TRIM) system. When a new ASF is requested, the file folder will have a bar coded label attached to ensure the system knows the location of a resident’s records. The two systems, CRIS and TRIM combine records to give the complete resident history. How do group homes get ASF’s The ASF is the corporate file which is used to record client information in residential services. All ASF files must have a TRIM label attached to the cover before information is placed in the file. To obtain a new ASF for a resident contact either the DAS administration or regional records unit, as required by the regions process. Regional records staff will register the ASF to the resident by the CRIS number, on the TRIM system. The file will be sent to the residential service via the regional process. How is the ASF used? Each resident has an ASF where all records must be kept in the relevant section. The ASF is the registered corporate file and is to contain one year of records. Each ASF should not be more than 5cm in thickness. Where a resident requires a large amount of records to be kept that causes the ASF to exceed the 5cm thickness, then a new ASF part should be requested. Parts will be used to form a series of information relating to the resident during the year which should be maintained in sequential date order. To manage retrospective organisation of ASF’s, the date range of the contents may be included as a reference as some of these files may not be sequential. When information contained in the file is more than one year old but remains current and required, it is to be transferred to the new ASF. A note that the document remains current and the date of transfer to the new file, is to be noted on the top of the document. For example a letter from the neurologist with safety instructions for a person with epilepsy. This document should be verified as still being current by notation of date and who verified the information, see RSPM 6.1.5. Records are to be placed into the relevant corresponding ASF section. What are operational records? Operational records capture the day to day operation of the residential service that are not specific to an individual resident. These include: diaries general shift reports staff roster and shift replacement household and staff routines shopping and menu planning household budget and finance information minutes of both staff and resident meetings. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.1 – 4 How are operational records managed? An Administration file (ADF) is the official corporate file that is to be used to manage operational records. An ADF is requested from regional records management. Each year, corporate files should be created for each specific type of information, for example there will need to be a file for house meeting minutes and a separate file for household budget and finance documents. These files are registered in the TRIM system. At the end of each calendar year the documents are to be moved to the archive, see RSPM 6.1.5. Role of staff All staff are responsible to complete and store required documentation on every shift. This will include but is not limited to: shift reports diary entries resident support including health, medication, Person Centred Active Support (PCAS) shift handover tasks such as cash counts In addition, staff are required to ensure: they adhere to the standards for written documents, see RSPM 6.1 all records clearly show the date of creation and, where required, a review or end date the name of the staff member who wrote the record is recorded document copies or those in draft are marked accordingly as only the most current and correct information is to be used. Role of supervisor and manager The records management responsibilities of individual staff and managers are defined in the Department of Human Services Records Management Policy and Department of Health Records Management Policy. The supervisor and manager are required to ensure: staff complete all records as required information is kept secure and only available to people who have a legal right to access the information ASF’s and ADF’s are updated each year the previous years records are managed as required, see RSPM 6.1.5 staff are trained in records procedures which relate to their work Resources File/health note template – a template to use for recording file notes or health notes for the resident file. It is available on the DAS Hub. Resident profile template – a template to record a brief resident profile. It is available on the DAS Hub. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.2 – 1 6.1.2 Client Relationship Information System (CRIS) Issued: August 2012 Applies to all Contents What is the Client Relationship Information System (CRIS)? What information is held in CRIS? What is information in CRIS used for? Who enters information in CRIS? Resources What is the Client Relationship Information System (CRIS)? The Client Relationship Information System (CRIS) is the primary electronic file system used to document client support information required by Disability Services. All people who are eligible for services and request support must have a CRIS file created. CRIS is not always used by residential services and the Accommodation Services File (ASF) remains the formal corporate record for residential services. What information is held in CRIS? CRIS stores information about: Critical Client Incidents or significant events contact with family or others which may impact on support needs changes in resident behaviour or health issues support plans information which may result in health or welfare risks issues which require specific action information and copies of legal or formal orders, such as guardianship or supervised treatment orders. What is information in CRIS used for? CRIS information is used to provide: individualised support a summary of data service use, for example, the Federal Government often requires statistical information to determine on-going funding requirements. Who enters information in CRIS? Staff with CRIS access may enter their case notes, health information, individual health plans, Critical Client Incident reports and alerts onto the system based on regional direction. Resources CRIS, CRISSP, FERIS – client electronic records system. Resources tolls and information http://intranet.dhs.vic.gov.au/corporate-service-hubs/technology/cris-crisspferis Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.2 – 2 Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.3 – 1 6.1.3 Personal information privacy and access Issued: August 2012 Applies to all Contents What is personal information? Privacy of personal information Who can access personal information? Who has legal authority to access personal information? Resources What is personal information? Personal information is any information, or opinion, which directly or indirectly identifies a resident. This includes: personal profiles plans case notes file notes health information. This information is held in a resident’s file. This includes the Client Relationship Information System (CRIS) file and the Accommodation Services File (ASF). Privacy of personal information Residents have a right to have their personal information remain private unless disclosure is required, or authorised by law, see RSPM 6.1. Residents can expect to: have personal information provided to others on a ‘need to know’ basis only have personal information stored securely be informed before any personal information is disclosed in situations where it is practical and desirable, to do so. Who can access personal information? Access to personal information held in resident files is restricted to: the resident, or their guardian or administrator with authority in the relevant area, for example, an administrator can only access financial records staff working in the residential service (including casual staff) who require the information to provide support other departmental staff with a legitimate business need professionals employed to provide services such as health professionals who need to access or record information to ensure the wellbeing of the resident those with legal authority Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.3 – 2 Who has legal authority to access personal information? Resources Under the Disability Act 2006, the following people can access a resident’s personal information without their consent. Community Visitors, who can: inspect any part of a residential service and see any resident, at any time, with or without previous notice make enquiries about service provision inspect any document relating to a resident which is not a medical record, this includes: – financial records – health files inspect any resident medical records, with the consent of the resident or their guardian, as defined in section 37 of the Guardianship and Administration Act 1986. A medical record is a record created by a treating medical practitioner for a medical purpose, that is, for medical assessment, diagnosis and treatment. The Disability Services Commissioner, who can: seek information from any service provider about the workings of their complaints system ask questions about the resident, or their support needs. The Senior Practitioner, who can: inspect and copy any document related to any resident they believe may be subject to a restrictive intervention or Compulsory Treatment Order ask questions about the resident or their support needs. Victorian WorkCover Authority inspectors who can: request any information they require to perform their role, which may include components of a resident’s file or health records. These requests must be referred to the regional Disability Accommodation Services manager. Corporate Integrity, Information and Resolutions Unit – provides information, advice, training and tools to support compliance with privacy legislation. Available on the DHS Hub. Disability Act 2006 – provides a legislative framework to strengthen the rights and responsibilities of people with a disability, see: the Victorian Legislation and Parliamentary Documents website at: http://www.legislation.vic.gov.au Office of the Public Advocate (OPA) – protects and promotes the rights of people with a disability, see: the OPA website at: http://www.publicadvocate.vic.gov.au Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.4 – 1 6.1.4 Freedom of information Issued: August 2012 Applies to all Contents What is freedom of information? Freedom of information and disability client records Records exempt from freedom of information Resources What is freedom of information? The Victorian Freedom of Information Act 1982 gives people the right to: access documents about their personal affairs and the activities of government agencies request incorrect or misleading information about them be amended or removed. The Act gives people the right to request information from: state government departments Ministers local councils most government agencies and statutory authorities public hospitals and community health centres universities, TAFE colleges and schools. Freedom of information and disability client records Disability client records are subject to the Freedom of Information Act 1982. It is important staff are aware of this whenever they create a record. Records exempt from freedom of information Some records are exempt from the Freedom of Information Act 1982 . For example: documents which would involve unreasonable disclosure of information relating to the personal affairs of a person, including one who is deceased health information about a person which would pose a serious threat to the applicant’s health or safety. Resources Freedom of Information Act 1982 – provides a legal framework which enables people to access personal information about them held by the government. Available on the Victorian Legislation and Parliamentary Documents website at: http://www.legislation.vic.gov.au Freedom of information Unit – comprehensive information about freedom of information for department staff. Available on the DHS Hub. Privacy policy – provides the policy and guidelines to meet privacy requirements in the Department of Human Services. Available on the Department of Human Services website at: http://www.dhs.vic.gov.au/disability Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.4 – 2 Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.5 – 1 6.1.5 Storing, maintaining, moving and archiving files Issued: August 2012 Applies to all Contents Overview Why are records retained? How long are records retained? ASF in current use ASF from previous year ASF is archived after 3 years Transferring files when a resident moves location Role of the supervisor and manager Resources Overview Residential services create and keep large amounts of records. Some records such as a personal profile are actively used over a long period of time, others are used short term, for example, continence charts. All information forms part of the department’s records about services provided and business decisions. When this information is no longer required for regular use or reference it is then managed in accordance with policy and legislative requirements known as archiving. Archiving is the process of managing records which are no longer considered to be active but may need to be referred to in the future. The Accommodation Services File (ASF) is the official department file for resident information. A new ASF should be created for each resident each year, and the previous year’s file can be archived. Staff and general household records must not be placed in an ASF. This information is managed in a separate house files and should also be archived on an annual basis. Why are records retained? Records are created and retained to: describe resident support needs keep a history of how support is provided to each resident provide evidence of actions and decisions in relation to resident support and the general management of the group home. Not all information is kept for the same length of time. A statutory document known as a Retention and Disposal Authority (RDA) specifies how long information relating to Disability Services needs to be kept. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.5 – 2 How long are records retained? All information gathered and used in the provision of disability services funded and or managed by the department, are managed according to the RDA. The life span of documents reflects its importance and relevance to both the care of the resident and its legal or legislative requirement. For example, life spans of records range from: Permanent, known as a state archive temporary, only a specified time after the record ceases to be required. For example, this may range from 1 year after information is no longer referred to or up to 75 years after death. ASF in current use Each ASF should contain one year of records relating to a client. At the end of each year a new ASF should be requested from Regional Records Unit and the previous ASF archived on site for 3 years. The archived ASF’s must be archived by DAS offsite after 3 years. All resident information is kept in their allocated ASF – do not place another resident’s information into some one else’s ASF. Check that documents are securely attached and the file does not contain items that should not be in the file, see RSPM 6.1, 6.1.1. ASF files must be kept in a locked and secured area, preventing unauthorised access. Keep Do not keep Original information multiple copies of the same document Notes (including sticky notes) related to a record securely attached to relevant record. draft information. old identification cards such as pension and health care, library or other membership cards Photos taken for support purposes– place into an a paper envelope and secured in the ASF. Note: resident’s personal photo’s are their personal property. other information not relevant to the resident. items that are not documents, see RSPM 6.1 Resident information must never be placed into general waste or household recycle bins. Draft, copies and any other item that has resident, staff or address details must be placed in secure bins for destruction. These are available at regional offices. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.5 – 3 ASF from previous year The ASF is placed into an archive box. The box must not be directly written on. The archive box may contain more than one resident’s ASF’s for that year however it is advisable that residents with a large volume of documentation and multiple ASF parts use a dedicated archive box containing only that residents’ records. The archived records must remain on site at the residential service for three years. During this time, the archive box must be stored in a locked area. After three years the archive is sent to the regional records unit for processing. All staff must ensure that boxes are managed in accordance with safe manual handling practices. Note: Client finance ledgers will not fit into the archive boxes. The hard covers should be removed and the ledgers folded over to place into the box. Ledgers and ASF’s should be kept in a separate archive boxes. ASF is archived after 3 years At the end of three years the records stored in the archive boxes are transferred to the regional office. ASFs are stored according to regional arrangements. This may be in the regional office or on an offsite secure storage facility. The TRIM system allows history, content, location and retention status of records to be easily identified if required. The archive boxes should have a completed box contents form placed in the front of the box which clearly states: what is contained in the box residential service address contact details date range of information Note: the boxes must not be directly written on. Resident information must never be placed into general waste or household recycle bins. Draft and copies must be placed in secure bins for destruction. These are available at regional offices. Operational records Records related to the general operation of the residential service are kept in the Administration file (ADF) and a new ADF should be commenced each year, see RSPM 6.1.1. The requirements for the management of the ADF content is the same as the ASF. The ADFs can be placed in the archive box with other operational records such as communication books and diaries. It is kept on site for 3 years and then transferred to regional records management. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.1.5 – 4 Transferring files when a resident moves location File transfer occurs when a resident moves from one site to another within the service. Files are not transferred to external agencies. The supervisor or manager responsible where the file is located must: check prior to transfer to make sure that all information has been filed appropriately make arrangements for the file to be transported securely attach the file transfer form to the front of the file ensure that details are filled in correctly, including details of the person who will receive the file. The supervisor or manager responsible at the file’s destination must: ensure that file is received intact complete details on the File Transfer form copy the completed File Transfer form and return a copy to previous location attach the File Transfer form to the ASF to ensure that when it is sent in for archiving that the information can be updated in the TRIM system. Role of the supervisor and manager Resources The supervisor and manager are required to have a system in place to ensure records are: managed in accordance with Department of Human Services Record Management Policy and Disability Services statutory obligations stored in a secure location within the residential service transferred securely to regional offices: – at the end of the three year on site storage requirement – when a resident is deceased or leaves the service. File Transfer form – a form that must be completed when files are transferred. Available on the DAS Hub. Information management – records storage and management information, policies, procedures and contacts on the DHS Hub. Information management – security policies, procedures and contacts on the DHS Hub. Records education unit resources and guides. Available on the DHS Hub. Archiving records in Disability Accommodation Services – a visual guide to managing the packing and management of archive box contents. Available on the DAS Hub. Public Records Office Victoria – PROS 08-13 Authority – Retention and Disposal Authority for Records of the Disability Services Function. Describes the retention period required for documents and who is authorised to dispose of documents that are not kept as a permanent public record. Available at: http://prov.vic.gov.au Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.2 – 1 6.2 Accountability of money Issued: August 2012 FBR – N GH/I – Y STJ/LTR/RTF – LD Contents Accounting for money Resident’s who don’t require assistance with money Staff accountability for funds Monthly statements of client funds The financial plan Unplanned expenses Resident inclusion Resources Accounting for money Staff are required to account for all resident and department money expended. The systems designed to manage and account for money used at the group home are there to: protect the funds of residents who cannot manage their own money ensure compliance with departmental financial management and accountability requirements, see RSPM 6.1 provide reports to financial administrators. The system is designed to keep a record of: all money held on behalf of residents in the Resident Trust Fund bank account transactions by staff who hold cards to access accounts on behalf of clients and the house how residents’ money has been spent Resident’s who don’t require assistance with money Residents who do not require any staff assistance and independently manage their own money are not required to participate in the Resident Trust fund processes. If staff are required to handle any client funds for any purpose they must be accounted for via the Resident Trust Fund process. The funds of respite and emergency accommodation service users are managed by a separate process. Staff accountability for funds Staff are accountable for all funds they handle so must document all expenditure as required in the relevant ledger and ensure receipts are provided. Staff must not use funds or resources intended for use by residents. For example, staff must make a contribution for meals and pay for private telephone calls, see RSPM 2.1. Monthly statements of client funds The department must provide residents, or their administrators a monthly statement of money received and spent. Residential services are provided with monthly statements which must be reconciled against all transactions for expenditure. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.2 – 2 The financial plan A financial plan must be developed and approved for every resident whose money is managed through the Resident Trust Fund. The financial plan is to be developed by the: resident administrator supervisor manager. The plan allocates the money available to residents and what it may be spent on. Staff must only expend funds according to the approved financial plan. The plan is to be kept in the finance section of the ASF. Financial plans must be reviewed annually. Unplanned expenses Occasionally there may be a need to use funds for a purpose not anticipated in the financial plan, for example, a resident may need extra money for: new clothing an unanticipated outing membership fees of a local sporting or leisure club. The administrator must approve unplanned expenses, before any purchases can be made or fees paid. Resident inclusion Resources Residents should be involved and informed about their financial plan. Where possible, they should be encouraged to manage their own money independently especially for small or regular purchases. This requirement can be included in routines and their financial plan. Client Expenditure Recording System (CERS) policy manual and tools – comprehensive instruction and forms for the management of people’s finances in Department of Human Services disability residential services. Available on the DAS Hub. Disability Services - Department managed Residential Charges Policy – Long Term Accommodation and Facility Based Respite – contains the current accommodation fees payable in department managed accommodation services. Available on the Department of Human Services website at: http://www.dhs.vic.gov.au/disability Managing utility costs – tip sheet to assist in managing and reducing use of electricity, gas and water. Available on the DAS Hub Rights and Accountability: Management of Money Policy – a policy for disability service providers and their staff on their roles and responsibilities in relation to managing the money of people with a disability living in residential services managed or funded by the Department. Available on the Department of Human Services website at: http://www.dhs.vic.gov.au/disability Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.3 – 1 6.3 Handling funds in respite services Issued: August 2012 FBR – Y STJ/GH/I/LTR/RTF – N Contents What monies can staff accept? Process for receiving spending money When a client holds their own money or valuables Housekeeping money Resources What monies can staff accept? Staff can only accept cash as personal spending money for respite service users. Staff must not accept respite and accommodation charge payments. These are made by, or on behalf of the person, to regional finance. Process for receiving spending money When respite service staff receive money, the following processes apply: they must check the amount given and immediately provide a receipt to the family, carer or service user, as appropriate if the service user arrives independently, staff must: – receipt the amount given – have it countersigned by another staff – provide a receipt to the family, carer or service user the amount received must be documented in the Record of Client Expenditure form. Cash provided should be secured in a locked tin which must be stored in a locked safe or cabinet. When a client holds their own money or valuables If a respite service user retains their own money or valuables, the following must apply: a Release form must be completed. This form releases staff from responsibility should the money or valuables be lost or stolen a Release form should be signed if a respite service user brings valuable personal property to the service, or when it is known they are retaining spending money. The Release form must be kept on file and only needs to be completed once. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.3 – 2 Housekeeping money Housekeeping money is made up of departmental funds which are provided to pay for groceries and, in some regions, utilities. This money is department funds and paid directly to group homes. When using housekeeping money, staff must: clearly document cash spent provide receipts complete a Declaration of Expenditure form when receipts cannot be obtained. All recording forms are pre-printed and available from management. Resources Rights and Accountability: Management of Money Policy – a policy for disability service providers and their staff on their roles and responsibilities in relation to managing the money of people with a disability living in residential services managed or funded by the Department. It is on the Department of Human Services website at: http://www.dhs.vic.gov.au/disability Disability Services – Department managed Residential Charges Policy – Long Term Accommodation and Facility Based Respite. Contains the current accommodation fees payable in department managed accommodation services. Available on the Department of Human Services website at: http://www.dhs.vic.gov.au/disability Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.4 – 1 6.4 Critical client incidents and non-critical client events Issued: August 2012 Applies to all Contents Overview What is the Critical Client Incident Management Instruction 2011? Regional responsibility for after hours support Role of support staff Completing a critical client incident report When a manager must be notified immediately (day or night) Staff actions When notification to a manager can wait until the next business day Staff actions Managing and recording non-critical client events Types of non-critical client events to record Additional reports and notifications may be required Role of supervisors and managers Resources Overview Reporting critical client incidents and non-critical client events that occur in Disability Accommodation Services form an important part of the ongoing process of monitoring practice and promoting quality improvement. The process ensures incidents and events are managed appropriately and all people involved are adequately supported. Serious incidents involving a resident are managed according to the Department’s Critical Client Incident Management Instruction 2011 and this must be followed by all directly managed services and funded agencies. Non-critical client events do not fall within the critical client incident management reporting system but still need to be recorded and captured at a local level to support and improve service delivery to residents. Non-critical client events are to be recorded in Department managed residential services and regularly used by local management to monitor practices and identify quality improvement strategies. This may reduce the risk of non-critical client events escalating to critical client incidents as far as possible. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.4 – 2 What is the Critical Client Incident Management Instruction 2011? Critical client incidents are those that have or may have a significant adverse impact on clients, service providers, the community, the department or government. Within the Department’s Critical Client Incident Management Instruction 2011 there are two categories of critical client incident: Category one These are the most serious incidents. A category one incident is an incident that has resulted in a serious outcome, such as a client death in unusual or unexpected circumstances, or severe trauma. Category two These incidents involve events that threaten the health, safety and/or wellbeing of clients or staff. The Department’s Critical Client Incident Management system ensures: appropriate Ministers, the Secretary, Executive Directors, Directors and Regional Directors are accurately and promptly informed the appropriate response and support are provided to all involved analysis of critical incidents both locally and centrally to assist and guide: – identification of gaps in policy and practice – review and improvement to policy and practice – practice strategies to reduce the reoccurrence of similar and serious incidents Regional responsibility for after hours support Regions are to ensure that appropriate management support is provided after hours. The reporting requirements for critical client incidents do not vary between business and after hours so regions must ensure that staff who will be providing this support: have sufficient knowledge and experience to provide the required support have a good knowledge of the Residential Services Practice Manual and the Department’s Critical Client Incident Management Instruction 2011 have a clear understanding of the reporting process and timelines required for critical client incidents are able to provide any immediate supports that may be required at the location of a critical client incident or provide referral for this to occur. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.4 – 3 Role of all staff Staff must follow the Critical Client Incident Management Instruction 2011 requirements and: make the required notifications to the manager where a manager must be notified immediately, staff must make all attempts to speak directly to a manager rather than leaving messages complete an incident report whenever a critical client incident occurs if in doubt whether an issue is a critical client incident or a non-critical client event, report it as a critical incident ensure other staff are informed of the incident and any actions to be implemented by documenting this in the shift report and resident files, as required by regional process notify the family of incidents that involve injury or hospitalisation of a resident, according to any agreed prior arrangements notify the manager immediately if you are unsure of the category of an incident, or if the circumstances related to the original report change complete any other reports required such as the Disease, Injury, Near Miss, Accident (DINMA) report. Completing a critical client incident report Staff must use the Department’s Critical Client Incident Report template. The report must be written clearly and include all factual information relating to the incident including: the exact circumstances of the incident including what happened, where and when the names and dosages of medications when incidents involve medication the names and role of every person involved in, or as a witness to the incident actions taken by any person, for example, applied first aid, called fire brigade, ambulance or police any instruction received from the manager or emergency services, stating what you were asked to do and by whom actions you took including what you did, when and where. This is to ensure all required and appropriate actions have been undertaken, including the provision of supports to residents and staff involved, and to check the incident is categorised appropriately. Staff should be aware that incident reports may be used in formal processes such as investigations into injuries and deaths. The reports are public records, so it is important that they do not contain comments or personal judgements that cannot be verified. Incident reports must be submitted via the regional critical client incident report lodgement process within the specified timelines. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.4 – 4 When a manager must be notified immediately (day or night) If any of the following incidents occur, a manager (the regular line manager during business hours or the manager providing after hours on-call support), must be contacted immediately regardless of the time and verbally notified of (in addition to the completion of the incident report): the death of, or serious injury to, a resident or staff member allegations of, or actual, sexual or physical assault of a resident or staff member by a staff member physical assault by a resident where the victim requires medical attention a fire involving death or serious injury a fire involving closure or significant damage to parts of a building or its contents serious property damage that makes the building unsafe or unusable injury or deterioration in health that requires urgent medical attention, hospital admission or attendance by an ambulance (that is not a requirement of an epilepsy management plan) all PRN chemical restraint medication errors missed or refused medication or errors in administration where these result in: – referral to, or attendance at a hospital emergency department – loss of consciousness or seizures – changes in consciousness that reduce a persons physical ability or normal communication capacity such as sleepiness, unsteadiness on feet or inability to communicate using usual communication methods an event occurs that has the potential to involve the relevant Minister, or subject the department to high levels of public or legal scrutiny. Staff actions The incidents noted above require immediate contact with a manager to notify them. Staff must: speak directly to a manager. The manager receiving notification of the incident must immediately determine if they should notify the DAS manager. follow any instruction provided by the manager ensure, as far as possible, that any person involved in the incident is adequately supported lodge the critical client incident report via the regional lodgement process. When notification to a manager can wait until the next business day If any of the following occur the regular manager should be notified. If any of these occur outside business hours, notification to a manager does not need to occur immediately and can wait until the next business day. These include: serious threats made against residents, staff, visitors or members of the public criminal behaviour resulting in police intervention excluding assaults that require immediate notification sexualised behaviour of a concerning nature that does not involve sexual assault unethical behaviour by staff, particularly if it involves taking advantage of residents, excluding assaults that require immediate notification. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.4 – 5 Staff actions Staff are required to: notify the manager lodge the critical client incident report via the regional lodgement process. The manager receiving notification of these incidents is not required to immediately notify the DAS manager, but should do so if they have concerns about the incident. Managing and recording non-critical client events Non-critical client events are events involving a resident that do not require incident reporting, but still need to be recorded and used at a local level to identify trends and develop strategies to prevent future critical client incidents. These are not reported as a critical client incident. These events are to be recorded using the Non-Critical Client Event Log to ensure all events involving a resident can be readily accessed by staff and their line manager at the local level. These event logs can be used regularly by key workers and house supervisors to develop strategies to minimise the risk of these issues escalating to critical client incidents. This information can also be used for discussion at staff meetings, and to regularly discuss with line managers the nature and frequency of non-critical client events at a site as part of regular monitoring and supervision. Where multiple residents are involved in an event a notation should be made in each resident’s Non-Critical Client Event Log to describe their role and how they were affected, to ensure all non-critical client event information for each resident can be considered together. Where details of an event are recorded in another location, for example, a behaviour support chart, a brief notation in the log is adequate with a cross reference to the location of the detailed event description. Staff are generally not required to report non-critical client events to the manager either immediately or the next business day, unless they have concerns about a particular issue. Similar to other client information, the Non-Critical Client Event Log should be kept in hard copy on the resident’s current Accommodation Services File and be made available to Community Visitors on request. Non-critical events that do not involve specific residents, such as minor neighbourhood concerns about vehicle parking or general noise levels, the loss of Client Expenditure Recording System (CERS) bank cards, or accidental withdrawal from the wrong bank account, do not get recorded as Non-Critical Client Events and can be recorded in shift reports. Current policies that include a requirement to complete an Incident Report for issues that are no longer reportable according to the Critical Client Incident Management Instruction 2011, will be amended to reflect these changes as they are due for review. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.4 – 6 Types of noncritical client events to record The following are types of non-critical client events that are to be recorded on the Non-Critical Client Event Log: Health and Wellbeing Concerns (Code HW) Anticipated deterioration of a known medical condition in a resident, where any contact is made with NURSE-ON-CALL, a medical practitioner or allied health professional. (Unanticipated deterioration of a known condition or the onset of an illness, where the resident attends, or receives treatment from a medical practitioner, is reported as a category 1 or 2 critical client incident). If doubt exists whether deterioration was anticipated or not, this should be reported as a critical client incident). Medication (Code MED) Any refused or missed medication or incorrect administration that a Pharmacist, Doctor or Poisons Information Line has advised does not require medical attention. (Errors leading to attendance at or treatment by a medical practitioner are reported as a category 1 or 2 critical client incident). Accidents/Falls (Code AF) Any accident or fall involving a resident, that does not lead to an injury, or the resulting injury does not require treatment by a medical practitioner. (Injuries requiring treatment by a medical practitioner, or unexplained or concerning injuries, are reported as a category 1 or 2 critical client incident). Concerning Behaviour (Code CB) Any PRN medication given for behaviour management that is authorised in a Behaviour Support Plan. (PRN medication for behaviour management that is not authorised is reported as a category 1 critical client incident). The focus of the recording in the event log is to capture the details of the behaviour and what occurred before and after, in order to identify patterns and ways to prevent events occurring or escalating to critical client incidents. All other PRN medication (not for behaviour management) can continue to be recorded in a resident’s file notes. Other (Code OTH) Any other events that raise staff concerns about the wellbeing of residents that are not serious enough to be reported as a critical client incident. These should also be raised with the manager as soon as possible on the next business day, to confirm they should not be reported as a critical client incident. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.4 – 7 Additional reports and notifications may be required Role of supervisors and managers Some critical client incidents will require completion of additional relevant reports. For example: The incident involved occupational violence: – Complete the Occupational Violence Risk Assessment Management Tool (OVRAMT) post incident tool – Complete a Disease, Injury, Near Miss, Accident (DINMA) report. A staff member was injured or nearly injured: – Complete a DINMA report – The Health and Safety Representative (HSR) must be notified. Any person on the property including residents, staff, contractors or visitors, was seriously injured and required medical attention: – Complete a DINMA report – Notify WorkSafe immediately by phone and send a completed Incident Notification form to WorkSafe within 48 hours. See RSPM 3.15, Serious incident notification to WorkSafe Victoria. If the incident involves a department vehicle: – The driver must complete the Lumley Insurance claim form, and a DINMA report. – If the vehicle is a bus, the fleet manager must be informed as a Transport Safety Victoria, bus incident notification may need to be completed and lodged. If a resident dies: – The coroner must be immediately notified of the death of any resident living in department managed residential services. Only the coroner can certify a resident’s death and authorise removal of their body. – The DAS Manager is required to notify the Community Visitors of the death. See RSPM 6.8. Supervisors and managers must ensure: supports, including debriefing, counselling or advocacy for residents’ or staff involved in an incident, are available all critical client incidents and non-critical client events have been recorded and dealt with appropriately and as required any additional reports and notifications have occurred as required communication has occurred to ensure all staff are aware of critical client incidents and any recommendations or follow up actions required implementation of recommendations or follow up actions is documented. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.4 – 8 Resources Responding to allegations of physical or sexual assault – a department instruction that sets out management and reporting requirements relating to allegations of assault. Available on the DHS Hub. Critical Client Incident reporting – reporting policy, report templates and guides. Available on the DHS Hub. Transport Safety Victoria – Bus safety information and incident notification forms available at: http://www.transportsafety.vic.gov.au/bus-safety When a person dies action checklist – a checklist to help ensure all requirements are met in the event of a person’s death. It is on the DAS Hub. When a person dies incident reporting guide – a guide to assist in writing the incident report in the event of a person’s death. Available on the DAS Hub. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.5 – 1 6.5 Damage caused by people living in residential services Issued: August 2012 Applies to all Contents Procedures to follow if a person causes damage What is intentional damage? Who pays for damage? If the person must pay for the damage What if the person who caused the damage, or their administrator, is unwilling or unable to pay? If the police have decided the damage is a criminal matter Resources Procedures to follow if a person causes damage Staff must refer to the Critical Client Incident Reporting Policy to determine what type of report should be completed when damage occurs. The manager must be informed immediately if damage: is related to property belonging to a member of the public results in the police being involved. The report for the circumstances above must contain: – the name of the person responsible – the type and extent of the damage and the circumstances of the incident – if the damage was intentional or unintentional – the name and address of the person whose property was damaged – the names of any witnesses. What is intentional damage? Intentional damage is damage which is deliberate. To be intentional a resident must understand the outcome of their action. This includes damage to property belonging to: the department co-residents staff a member of the public. Staff must follow the Critical Client Incident Reporting Policy in conjunction with this instruction. Who pays for damage? The damage may be paid for by the resident or the department. Responsibility for costs will be determined by regional management based on considerations including: if the damage was intentional, or unintentional if the resident was being supported appropriately when the damage occurred. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.5 – 2 If the person must pay for the damage The supervisor and manager should determine the cost of the damage according to quotes or receipts. This information must be provided to the resident’s administrator. The administrator will decide how the payments will occur. For example, the administrator can arrange payment by: making a direct payment to the person whose property was damaged requesting payment be made out of the client funds available at the group home. The administrator may suggest replacing or repairing the damaged item. What if the person who caused the damage, or their administrator, is unwilling or unable to pay? If the resident or their administrator refuses to pay, after it has been determined they are responsible for the costs, the matter should be referred to the department’s Legal Services Branch. If the resident does not have sufficient funds they, or their administrator, should make arrangements to make the payment by instalments, or when funds become available. This arrangement should be documented and a copy placed with the resident’s ASF financial information. If the police have decided the damage is a criminal matter If the police decide the damage is a criminal matter, client services should be involved to ensure the resident is represented and understands the proceedings. The court will determine if the resident is guilty and may provide directions regarding how the resident must pay. The supervisor and manager are required to determine the cost of the damage and provide the police with this information. Resources Critical Client Incident reporting – reporting policy, report templates and guides. Available on the DHS Hub. House maintenance guide – a guide for accessing maintenance and repairs in group homes. Available on the Department of Human Services website at: http://www.dhs.vic.gov.au/about-the-department/documentsand-resources/policies,-guidelines-and-legislation/disability-supportedaccommodation-house-maintenance-guide Singleton Equity Housing Limited and properties owned or managed by other housing options, follow the maintenance information provided at the site. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.6 – 1 6.6 Missing people Issued: August 2012 FBR/GH/I – Y STJ/LTR/RTF – LD Contents Overview Confirming if a resident is missing If a resident is confirmed missing Informing and reporting When the resident is found Resources Overview Residential services are generally voluntary and residents have freedom of movement within their community unless they have an authorised restrictive intervention or legal order in place. This must to be balanced with reasonable actions to ensure resident’s who require support to access the community safely are not placed at unreasonable risk, see RSPM 1.2, 4.2. The level of support and the resident’s safety risks are to be documented in their profile and plans to ensure appropriate action can be taken if the resident’s whereabouts are unknown. Confirming if a person is missing Staff must take the following steps to confirm if a resident is missing: If Then the resident is known to wander the resident will have a response plan in their file (consult the plan for the steps to follow) a resident goes missing from the residential service check the diary to see if the resident is at a pre-arranged meeting or appointment ask others at the residential service if the resident mentioned they were going out and where they were going search inside and outside the residential service and nearby properties search the resident’s favourite places a resident goes missing on an outing a resident does not return to the residential services at the usual, or allocated time search the immediate area notify staff at the residential service or the manager seek assistance from the police, or bystanders, if the resident is at risk when on their own if the resident was at a particular organisation, contact the organisation to find out information about the resident’s whereabouts if a pre-booked taxi was used, contact the taxi service to determine if, or when the resident, was picked-up or dropped off. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.6 – 2 If a person is confirmed missing As soon as a resident is confirmed missing, staff must notify the manager immediately and: If the resident: Then has a Supervised Treatment Order is at risk to themselves or the community when unsupervised does not have a Supervised Treatment Order is not known to wander is not a risk to themself or the community when unsupervised the police do not need to be contacted immediately (the police must be contacted if the resident is not found within an hour of being confirmed missing) in case the police need to be contacted, compile a description of the missing resident by completing the Missing Person Identification form and have a recent photograph of the resident, should it be required has not been found within an hour of being confirmed missing telephone 000 to report the missing resident give the police a copy of the Missing Person Identification form and a recent photograph of the missing resident record in the communication book the name, rank and personal identification number of the police officer who compiled the report decide whether to contact the police earlier than an hour depending on the situation and the resident involved (management must assist with this decision, as required). Informing and reporting report the matter to the police immediately and: provide information documented on the Missing Person Identification form provide a photograph of the resident record in the communication book the name, rank and personal identification number of the police officer consulted Step Action Up-date the manager management must be informed of the missing resident if a report is made to the police, the staff member who made the report must inform their manager immediately inform the missing resident’s family the manager must inform the missing resident’s family and develop a plan to keep them up-dated complete a Critical Client Incident Report the staff member on duty when the resident went missing must complete an Critical Client Incident Report the category of the incident will depend on the circumstances and the resident involved, see RSPM 6.4 Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.6 – 3 When the person is found Staff must immediately inform: their manager other relevant staff the family the police, if the resident was not found by them. Staff must ensure the resident’s wellbeing by: checking for physical or emotional injuries assessing and arranging medical attention, as required. Resources Critical Client Incident reporting – reporting policy, report templates and guides. Available on the DHS Hub: http://intranet.dhs.vic.gov.au/resources-and-tools/policies-andstandards/incident-reporting-departmental-instruction Missing person checklist – a list of tasks to complete if a person is missing. Available on the DAS Hub. Missing Person Identification form – a form to provide emergency services with relevant information. Available on the DAS Hub. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.6 – 4 Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.7 – 1 6.7 Responding to physical and sexual assault Issued: August 2012 Applies to all Contents What is physical assault? What is sexual assault? Issues that are not reportable as physical or sexual assault Reporting allegations to the police If staff suspect a client has been sexually assaulted What to do when an allegation is made Supporting victims of sexual assault Who must report the allegation to the police? Staff actions Resources What is physical assault? For the purpose of this instruction, physical assault is defined as the application of force which causes physical injury requiring medical attention. This definition is not as broad as the definition provided in the Crimes Act 1958, to exclude some actions which people with a disability may take due to a lack of social expectation awareness. What is sexual assault? Sexual assault includes rape, assault with intent to rape and indecent assault. Examples of indecent assault include: unwelcome kissing or touching of a person’s breasts, buttocks or genitals forcing a person to watch pornography or masturbation. Issues that are not reportable as physical or sexual assault There are some behaviours that do not require a Critical Client Incident Report and reporting to police. These are treated as non-critical client events and they include: minor shoving between residents inappropriate touching by a resident who lacks understanding of the behaviour exposure in a public place by a resident in some contexts a resident does not understand the significance of their behaviour, because of their cognitive ability, for example, a resident may be unable to distinguish between the significance of touching someone on the arm, as opposed to touching them on the breast. The manager is to be informed, see RSPM 6.4, and an appropriate support plan implemented and monitored. If staff are unsure as to the nature of the issue they should seek immediate advice from a manager. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.7 – 2 Reporting allegations to the police Allegations of physical or sexual assault, are defined in the department’s Responding to Allegations of Physical or Sexual Assault policy, and must be reported to the police. Physical and sexual assault includes: rape of or by a resident rape or indecent assault by a staff member, volunteer carer or member of the volunteer carer’s household the production of child pornography by a resident, staff member or volunteer physical assault of a resident by a staff member, volunteer carer or member of the volunteer carer’s household (regardless of the need for medical attention) physical assault of or by a resident resulting in medical attention being required (treatment by a medical practitioner) physical assault of or by a resident involving a weapon, such as a knife, hammer or other object. This instruction applies whenever there is an allegation a resident has assaulted, or been assaulted by: another resident a staff member a volunteer carer a visitor to the residential service a family member a community member. If staff suspect a client has been sexually assaulted Some residents may be unable or unwilling to report a sexual assault. Staff working with people with a disability must be aware of possible indicators of sexual assault. These include: significant behavioural changes which may include: – self-destructive behaviour – sleep disturbances – acting-out persistent or inappropriate sexual play physical symptoms caused by sexually transmitted diseases or pregnancy complaints of physical symptoms, such as abdominal pain. Staff who suspect sexual assault may have occurred must immediately discuss this with their manager, or after hours support. A medical review should also occur as soon as possible with immediate medical attention sought, if a resident displays physical or emotional signs of assault. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.7 – 3 What to do when an allegation is made Allegations of assault must always be treated seriously. When there is an allegation of assault, staff must: immediately takes steps to create a safe environment, if the threat remains reassure and support the resident and advise them of what will happen next report the allegation to the police. If the victim or perpetrator has a cognitive disability, advise the police, an Independent Third Person (ITP), will be required. If the victim or perpetrator is less than 18 years of age, a parent, plenary guardian, or Independent Person (IP) must be present when they give a statement. The police are responsible for contacting the ITP or IP. Staff must not: act as an ITP interview the resident about the allegation, as this is a police role. Some discussion may be required to: ensure the resident’s safety obtain a basic understanding of what has happened. If the resident needs to talk about what occurred, listen and show concern. Depending on the resident’s age and status, notify their next-of-kin, or guardian, as appropriate. For further information, refer to the department’s policy: Responding to allegations of physical or sexual assault. Supporting victims of sexual assault A resident’s feelings may be influenced by their initial reaction to the allegation. If they sense a negative response, this may cause or reinforce feelings of guilt and shame. If a sexual assault is disclosed, a helpful response may include: letting the resident know you believe them making it clear whatever happened is not their fault reassuring them disclosing the assault is the right thing to do telling them they are not is responsible for the assault. Sexual assaults reported to police are immediately referred to The Centre Against Sexual Assault (CASA). CASA provides 24-hour advocacy and counselling and will support the victim to decide what they want to do. Who must report the allegation to the police? The allegation must be reported to the police by: the most senior staff member on duty at the residential service the person who was told of the alleged assault, if a senior staff member was not on duty at the time. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.7 – 4 Staff actions Resources If the alleged perpetrator is present and is continuing to threaten any person, then staff are to call ‘000’ to seek immediate assistance. Critical Client Incident reporting – reporting policy, report templates and guides. Available on the DHS Hub: http://intranet.dhs.vic.gov.au/resources-and-tools/policies-andstandards/incident-reporting-departmental-instruction Independent Third Person, Office of the Public Advocate – for comprehensive information on role and functions of the Office of the Public Advocate, see: http://www.publicadvocate.vic.gov.au and click on ‘Services’ Responding to allegations of physical or sexual assault – a department instruction that sets out management and reporting requirements relating to allegations of assault. Available on the DHS Hub. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.8 – 1 6.8 When a person dies Issued: August 2012 Applies to all Contents The role of the Coroner If staff believe a person has died at the residential service Who can determine if a person has died? When it is determined a person has died at the residential service If a person dies in hospital Role of the manager Removal of the body when a person dies at the residential service After the Coroner’s investigation Responsibility for funeral and burial arrangements The role of friends or staff in funeral arrangements Departmental inquiry into a person’s death Resources The role of the Coroner The coroner may investigate deaths that must be reported to the Victorian Coroner by law. This includes deaths that: are sudden are traumatic or unexplained occur in people who reside in residential or custodial services that are the responsibility of government (even if the death occurs elsewhere). This means it is mandatory to report the death of a resident of a department managed residential services, even if the person dies while absent from the service, for example, in hospital, on holiday or an overnight stay with family or friends. The Victorian Coroner is the only person who can legally certify a resident’s death and authorise removal of their body from the residential service. If staff believe a person has died at the residential service If staff believe a resident has died, they must: call an ambulance immediately implement relevant first aid procedures, see RSPM 3.12, 5.16 follow directions provided over the telephone by ambulance personnel note the time the resident was discovered notify the manager as soon as possible. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.8 – 2 Who can determine if a person has died? The following people can determine if a resident has died in a residential service: a doctor ambulance personnel other medical professionals. When it is determined a person has died at the residential service If it is determined that a resident has died at the residential service staff must: contact management contact police document the names, rank and identification numbers of the police who attend discuss with management, the most appropriate person to contact the family, and ensure they are notified provide verbal information requested by the police not provide a written statement to the police at this time. If a person dies in hospital If a resident dies in hospital, staff must: inform the manager, or after hours support, as soon as possible. check if the hospital has notified the family where the family is not present at the time the person dies. While the hospital has primary responsibility to notify next of kin and respond to any queries related to medical issues, a representative of the department is also required to make contact with the family. This may need discussion with the manager to determine the most appropriate staff member to make contact, for example, it would usually be the supervisor or manager but at times a key worker may have a close working relationship with the family and may make this contact. The contact must occur as soon as possible. ensure the hospital is aware that the Coroner must be involved inform staff coming on shift of the resident’s death. follow the Critical Client Incident Reporting instruction, see RSPM 6.4. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.8 – 3 Role of the manager The manager must ensure: the family has been contacted by the most appropriate departmental staff person the family is aware of the legal requirement for the Victorian Coroner to be notified of the death the Coroner has been informed (regardless of where the death occurs) where another service, such as police or hospital, state they have informed the Coroner, the manager must confirm this with the Coroners office Critical Client Incident reports are completed and the Disability Accommodation Services manager is informed, see RSPM 6.4 the resident’s guardian has been informed of their death (orders cease upon death, but notification should occur as soon as possible). support is arranged for co-residents and staff, this may include debriefing from the Critical Incident Stress Management service, or counselling through the Employee Assistance Program, see RSPM 2.4 requirements are completed according to the ‘When a person dies’ checklist the Divisional Executive Director or delegate notifies the Community Visitors Program Manager of a resident death the death is noted in the Client Records Information System (CRIS) and records are archived, see RSPM 6.1.5. Removal of the body when a person dies at the residential service When a resident dies at a residential service the Coroner, or their representative, are the only people who can authorise removal of their body. In the metropolitan area, the Coroner will arrange for the body to be taken to the Coronial Services Centre. In rural areas, the resident’s body is usually taken by ambulance to the local hospital mortuary. After the Coroner’s investigation After the Coroner has investigated the death, the family, or person arranging the funeral, must arrange for the body to be collected by the funeral director. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.8 – 4 Responsibility for funeral and burial arrangements The family is usually responsible for funeral arrangements. If the resident does not have a family, advice should be sought from the State Trustees. The State Trustees take responsibility for burial when there is no one to arrange it. In this case there may not be a funeral service. The role of friends or staff in funeral arrangements The person arranging the funeral will decide who should be consulted, or asked to participate in the funeral service. Sometimes a decision is made that a private service will occur where group home staff and other residents may be excluded from attending. Where this occurs, the group home may choose to hold its own memorial or participate in some other event or ritual to remember the resident, for example by planting a memorial tree in the garden. This can be an important part of the grief process. If residents or staff require support to manage the death of a resident, they should access the Australian Centre for Grief and Bereavement. Staff may also access the Employee Assistance Program (EAP), see RSPM 2.4. Departmental inquiry into a person’s death Resources The death of a resident is always treated as a Critical Incident, see RSPM 6.4. Many Critical Client Incidents are reviewed and in some cases the department may investigate a resident’s death. Critical Client Incident reporting – reporting policy, report templates and guides. Available on the DHS Hub: http://intranet.dhs.vic.gov.au/resources-and-tools/policies-andstandards/incident-reporting-departmental-instruction –incident reporting policy, report templates and guides. Available on the DHS Hub State Coroners Office of Victoria – telephone: 1300 309 519. Available at: http://www.coronerscourt.vic.gov.au State Trustees – helps people with their financial needs, telephone: 03 9667 6444. The website is located at: http://www.statetrustees.com.au When a person dies action checklist – a checklist to help ensure all requirements are met. Available on the DAS Hub. When a person dies: incident reporting guide – a guide to assist in writing the incident report in the event of a person’s death. Available on the DAS Hub. Australian Centre for Grief and Bereavement – provides information about counselling and support services. Available at: http://www.grief.org.au Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.9 – 1 6.9 Wills and deceased estates Issued: August 2012 Applies to all Contents Who can make a will? What is testamentary capacity? Witnessing a will and making an affidavit Role of support staff What if a person dies without a will? What if the person who died had unpaid bills or debts? Resources Who can make a will? Anyone who has testamentary capacity can make a will. The Supreme Court can also make a will on behalf of a person who lacks the capacity to do so. What is testamentary capacity? Testamentary capacity means at the time of making the will the person: understands the nature and effect of what they are doing knows in general terms what property they own and can dispose of can judge the claims different people may have on their estate. Witnessing a will and making an affidavit For a will to be valid, it must be signed by two independent witnesses aged over 18 years of age. A person’s partner should not be a witness. Witnesses should also not be beneficiaries of the will. If there is any reason why a person’s capacity to make a will may be challenged at a later date, it is advisable to ask a GP or solicitor to witness the will and swear an affidavit as an attachment. In the affidavit, the GP or solicitor must confirm the person has testamentary capacity when making the will. Role of support staff It is not the role of staff to: ensure residents have a will. This is the responsibility of the resident or their guardian. be involved or assist with preparing a resident’s will. Additionally, staff must not: assess a resident’s capacity to make a will act as an executor for a resident’s will. In situations where staff are made executors without their knowledge, they must renounce the appointment by filing an affidavit with the Register of Probates and arrange for the court to appoint someone else. benefit from the estate of a resident they support. In cases where staff are named beneficiaries without their knowledge, they should renounce this knowingly attempt to benefit from the estate of a resident. Staff can refer residents to an appropriate service such as a solicitor, the Community Legal Centre or State Trustees if they want to make a will, or their family requests a will to be made on their behalf. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 6.9 – 2 What if a person dies without a will? When a resident dies without a will: The manager must notify the client services officer at the State Trustees and arrange for a letter to be written advising them of: – the person’s death – details of any known assets and liabilities – next-of-kin, if known. The State Trustees are responsible for the estate until an administrator is appointed. The deceased resident’s former financial administrator is not the administrator of their estate. The next-of-kin, or interested parties, can apply to the Supreme Court to administrate the estate. If no one applies to be the administrator, State Trustees will be responsible for administering the estate. This includes: paying any debts distributing the estate to beneficiaries. State Trustees are responsible for arranging the collection of the resident’s property and holding it in storage until it can be distributed to beneficiaries. Prior to the property being collected, the manager should arrange for small items to be stored in a locked cupboard, or safe at the residential service. Money must be returned to the Resident Trust Fund. Larger items, such as a chair, table or audiovisual equipment, may remain in the residential service, or be stored in a secure locked garage or shed, if available. What if the person who died had unpaid bills or debts? If the resident has unpaid bills or debts, the organisation or individual owed money (the creditor) must seek payment from the executor or administrator. Resources If Then the resident has a will there will be an executor managing their estate (refer the creditor to this person) the resident does not have a will their assets will be frozen until an administrator is appointed (the administrator will be State Trustees or a person appointed by the court – refer the creditor to this person). National Association of Community Legal Centres – has links to local Community Legal Centres which provide free, confidential advice and assistance about a variety of legal matters. Available at: http://www.naclc.org.au State Trustees – helps people with their financial needs. Available at: http://www.statetrustees.com.au Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – Part 7 In this section 7 Positive behaviour support 7.1 Reducing and preventing behaviours of concern 7.2 The Senior Practitioner 7.3 Restrictive interventions 7.4 Behaviour Support Plans 7.5 Compulsory treatment RSPM application to service type Each instruction has service type and instruction application codes to assist to identify how the specific instruction applies to supported accommodation by service type. Service type: FBR facility based respite GH group homes STJ short term justice LTR long term rehabilitation program I Sandhurst and Colanda RTF residential treatment facility (DFATS) Instruction application: Y instruction applies in full N instruction does not apply to service type P Partial application. Service required to implement principle of instruction but service not generally directly responsible for planning, monitoring and reviewing components of instruction LD Locally determined based on client plans, service model and protocols. Applicable to STJ, LTR and RTF only Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – Part 7 Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.1 – 1 7.1 Reducing and preventing behaviours of concern Issued: August 2012 Applies to all Contents Overview Factors that impact on behaviour Role of staff When is an authorised BSP required? Resources Overview Behaviours that impact on an individual and those around them is more than behaviours defined as behaviours of concern and use of restrictive interventions. Support strategies that provide opportunities for a resident to develop skills for meaningful interaction and participation, in conjunction with appropriate health management will prevent or significantly reduce the risk of behaviours of concern or withdrawal. All life areas need to be considered and addressed as far as possible before any restrictive interventions can be considered, authorised or implemented. Also see RSPM Preface: Promoting positive practice and RSPM 4.3. Factors that impact on behaviour All human beings behave according to a variety of factors that include but are not limited to: personal life experiences attitudes and expectations of the individual and others physical and social environments physical, mental and oral health People with a disability may also be impacted by: the cognitive and physical impacts of disability medications they take discrimination, for example, being denied access to education or employment poor access to information, support or physical environments exclusion from activities, conversations and decisions. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.1 – 2 Role of staff Staff are to follow the Person Centred Active Support (PCAS) method of working with resident’s and seek specialist advice and assistance as directed by the resident needs, support plan and related parts of the RSPM. Residents are to be supported to develop and maximise: good health communication skills relationships and social connections choice and decision making skills to manage and cope with change The resident’s support plan, implemented in conjunction with the resident along with RSPM sections 4 and 5, provide guidance about the information and support activities required for each individual resident. When is an authorised BSP required? A Behaviour Support Plan (BSP) may be a useful support tool where a resident has behaviours of concern that are managed without the use of restrictive interventions. In this circumstance, the use of the BSP does not require authorisation or reporting to the Office of the Senior Practitioner as no restrictive interventions are used. An authorised Behaviour Support Plan is required when a resident has significant behaviours of concern where supports or interventions require the use of restrictive practices, see RSPM 7.3, RSPM 7.4. Staff must not implement any intervention that is restrictive without a BSP that is developed using the Positive Behaviour Support framework, approved by the Authorised Program Officer (APO), explained to the resident by an Independent Person (IP) and lodged with the Office of the Senior Practitioner (OSP). Resources Positive Behaviour Support framework- a practice framework designed to reduce use of restrictive interventions and improve quality of life for people with behaviours of concern. Available on the Department of Human Services website at: http://www.dhs.vic.gov.au/about-the-department/documents-andresources/reports-publications/positive-behaviour-support-getting-it-right-fromthe-start Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.2 – 1 7.2 The Senior Practitioner Issued: August 2012 Applies to all Contents Role of the Senior Practitioner Functions of the Senior Practitioner What is an Authorised Program Officer? Role of the Authorised Program Officer What is an independent person? Role of the independent person Resources Role of the Senior Practitioner The Disability Act 2006 states the role of the Senior Practitioner is to ensure: the rights of people subject to restrictive interventions and compulsory treatment are protected appropriate standards for restrictive interventions and compulsory treatment are complied with. Functions of the Senior Practitioner The Senior Practitioner develops guidelines and standards with respect to restrictive interventions and compulsory treatment and provides: education and information with respect to restrictive interventions and compulsory treatment information with respect to the rights of persons with a disability who may be subject to restrictive interventions or compulsory treatment advice to improve practice in relation to restrictive interventions and compulsory treatment directions in relation to restrictive interventions, compulsory treatment and behaviour support and treatment plans The Senior practitioner is also to: develop links and access to professionals, professional bodies and academic institutions for the purpose of facilitating knowledge and training with regards to clinical practice for staff working with persons with a disability undertake research into restrictive interventions and compulsory treatment and provide information on practice options to disability service providers evaluate and monitor the use of restrictive interventions across disability services recommend improvements in practice to the Minister and the Secretary perform any other functions specified or required by the Disability Act 2006. What is an Authorised Program Officer An Authorised Program Officer (APO) is any person approved and appointed by the Secretary of the Department of Human Services, to authorise Behaviour Support Plans that require the use of restrictive interventions. Authorisation can be revoked by the Secretary. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.2 – 2 The role of the Authorised Program Officer The APO must ensure that strict criteria have been met in the development of the Behaviour Support Plan, including inclusion of least restrictive alternatives consistent with the Positive Behaviour Support framework. Restrictive interventions can only be used when a resident displays behaviours which place them or others at risk, and behavioural change has not occurred with the introduction of nonrestrictive interventions. The APO may only authorise the use of restrictive interventions where: It is necessary to prevent the resident from: – causing physical harm to themselves or others – destroying property when doing so involves the risk of harm to themselves or others. Note; property destruction alone is not sufficient to implement a restrictive intervention. evidence is provided that it is the least restrictive alternative for the resident and co-residents and the evidence describes: – the strategies that have already been tried – why the restriction is necessary – how the restrictive intervention will be reduced and removed overtime – how the option places the least restriction on co-residents. What is an independent person? An Independent Person (IP) assists residents to understand the restrictive interventions in their Behaviour Support Plan. An IP must not: be a disability service provider, or a representative or an employee of a disability service provider have any interest in a disability service provider which is providing, or has provided, disability services to the person with a disability. An IP toolkit, which contains a range of information for service providers and staff and persons who may act as an IP, is available from the Office of the Senior Practitioner. Role of the independent person The IP must explain to the resident: the inclusion of restraint or seclusion in their BSP they can seek a review of the decision to include restraint or seclusion in their BSP how the revised BSP will be different, should they already have a BSP. The IP may report the matter to the Public Advocate if they consider: the resident is not able to understand the proposed use of restraint, or seclusion, as detailed in their BSP the requirements of the Disability Act 2006 are not being complied with. Resources Office of the Senior Practitioner – oversees, and provides information and resources on, the use of restrictive intervention and compulsory treatment. Available on the Department of Human Services website: http://www.dhs.vic.gov.au/for-individuals/your-rights/offices-protectingrights/office-of-the-senior-practitioner Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.3 – 1 7.3 Restrictive interventions Issued: August 2012 Applies to all Contents What are restrictive interventions? Least restrictive strategies must be tried Locking of doors and windows The use of side rails on beds Chemical restraint Physical restraint Seclusion What interventions are not reportable? Approval of restrictive interventions Emergency use of restraint and seclusion Reporting requirements The role of the supervisor and manager Resources What are restrictive interventions? A restrictive intervention means any intervention used to restrict the right or freedom of movement of a person with a disability. This includes: chemical restraint – a chemical substance used for the primary purpose of behavioural control mechanical restraint – the use of devices to prevent, restrict or subdue movement for the purpose of behaviour control seclusion – the sole confinement of a person where the windows and doors cannot be opened by the person from the inside, or are locked from the outside. Staff should refer to the Disability Act 2006, Part 1 – Preliminary, Section: 3 for more detailed definitions of the above restrictions. In addition, any action which impacts on a resident’s rights according to the Victorian Charter of Human Rights and Responsibilities Act 2006 must be viewed as restrictive, see RSPM Preface. Restrictions may be physical or psychological. Physical restrictions include, but are not limited to: locking doors, windows and cupboards physically holding a resident (physical restraint) or blocking access to a common area of the residential service, such as the kitchen straps or belts on chairs and bed rails used to stop or restrict a resident’s freedom of movement. Psychological restrictions include, but are not limited to: exclusion from activities verbal threats and intimidation any action or directive which creates compliance through the use of fear. For example, ordering a resident to go to their room, or lie on the ground. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.3 – 2 Least restrictive strategies must be tried Least restrictive strategies must always be tried by following the Positive Behaviour Support framework. Staff must only apply restrictive strategies that are part of the authorised Behaviour Support Plan (BSP). Restrictive interventions must be: 1. Part of a resident’s approved BSP 2. Administered in accordance with the resident’s approved BSP 3. Only applied for the period of time which has been approved by the APO 4. Have been explained to the resident by an Independent Person. To decide if an intervention is restrictive the intent or primary purpose needs to be determined. To do this staff must ask if the intervention is for behaviour control or to restrict freedom of movement. Unauthorised restriction may breach duty of care, see RSPM 1.2. If the intent or primary purpose is unclear, the intervention should be treated as restrictive, be authorised before it can be used and must be reported. The locking of internal or external doors and windows to restrict a resident’s access in or out of the residential service, or access to internal common areas or facilities, is a restriction on freedom of movement and is a restrictive intervention. This includes: placing locks on cupboards and refrigerators to restrict access to food turning-off the water supply to taps in bathrooms or kitchen, or restricting access to water. The approval and reporting processes in these situations is the same as those required for other restrictive practices. Access restrictions to any area or common facility must be noted on the Residential Statements of co-residents. The information must include strategies to reduce the impact on co-residents. Examples of locked doors and windows not considered a restrictive intervention include: a door being locked from the outside when a resident is absent (to protect their property from theft) external doors and windows (which do not require a key to be opened from the inside) being locked for the purpose of deterring intruders the front door being locked from the inside to ensure the safety of resident who require constant supervision when outside of the residential service. For example, residents with little or no understanding of road safety who may walk onto the road. For these residents the following must occur: – the safety issue must be noted in their support plan – the practice must be included in the Residential Statements of co-residents – written approval for door locking practices to be implemented must be provided by the Disability Accommodation Services manager – doors must only be locked when the resident for whom approval is applicable, is at the residential service – the approval must be reviewed every 12 months to ensure it: o remains necessary o is the least restrictive option for co-residents. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.3 – 3 The use of side rails on beds The use of bed side rails should only be considered in exceptional circumstances. Chemical restraint Chemical restraint medication must be authorised and administered in accordance with the medication section of the RSPM. Staff should read the medication information provided by the resident’s doctor and pharmacist and contained in their BSP to understand the reasons why it is being prescribed. If the prescribing doctor details specific medication monitoring is required, it must be included in the resident’s BSP. If additional monitoring, other than observing the resident is required, the supervisor and manager must determine the capacity of staff to do this based on the: requirements involved skills of staff. Information from the pharmacist and prescribing doctor should be discussed at the staff meeting to ensure staff have a shared understanding of why the resident has been prescribed chemical restraint medication. If other medication changes occur, staff should ask the doctor if these may impact on the prescribed chemical restraint medication. If the doctor or pharmacist indicates the effect of chemical restraint medication may be altered, (even if the chemical restraint medication dose has not been altered), the information must be reported to the APO and the Office of the Senior Practitioner to determine if a variation to the resident’s BSP is required. Chemical restraint must be reviewed by the treating doctor at no more than four month intervals. A review must also occur annually (or more often if determined during the planning process) by the relevant medical specialist, for example, the psychiatrist, paediatrician, neurologist or gynaecologist. For example, consideration should be given to less restrictive interventions such as lowering the bed to its lowest level and placing a fall-out mat beside it, if there is a risk the resident may roll-out. Bed side rails represent the most restrictive option and can only be used where a comprehensive assessment by a qualified occupational therapist demonstrates they: present a lower risk to the resident than not using them are not for mechanical restraint purposes. The same therapist must specify the details of how and when bed side rails can be used. In this circumstance the APO needs to sight evidence, for example, an assessment tool, report or recommendation, which states the bedding system has been prescribed for therapeutic purposes, and not mechanical restraint. Any bed side rail system which has not been recommended following assessment by an occupational therapist, and prescribed by them, must be: considered mechanical restraint approved and reported as a restrictive intervention. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.3 – 4 Physical restraint Physical restraint is where a person is physically held by another person to prevent movement. Physical restraint may only be used in strict accordance with the OSP Direction on Physical Restraint as it presents a high risk of injury to all involved. Some forms of physical restraint in conjunction with specific risk issues that some individuals may have, can cause death so are prohibited. Applying unauthorised or prohibited physical restraint may be assault. Staff should never apply physical restraint unless it is part of an authorised BSP they have been trained to implement. Safety measures, such as holding a person’s arm for a brief period to stop them walking onto a road, is not considered physical restraint. Seclusion Seclusion is the confinement of a resident to a room or part of a building that is locked or has a barrier used that stops their freedom to exit. Where seclusion is part of an authorised BSP staff must ensure: the environment is suitable, including appropriate heating and cooling clothing, food and medications are available access is available to appropriate toilet facilities The maximum time period allowed for the seclusion must be documented in the BSP and adhered to. What interventions There are some restraint exemptions which are not reportable under the Disability are not Act 2006. These include: reportable? the use of seatbelts and seatbelt buckles to stop a resident removing the belt when in a moving vehicle support straps to ensure a resident does not fall from a wheelchair splints applied for therapeutic purposes psychotropic medications prescribed to treat a resident’s psychiatric illness which has been diagnosed and documented by a psychiatrist. Prescribed treatment or therapy which is not reportable as a restrictive intervention must be documented as a specific management strategy in the resident’s health plan, and be reviewed by the relevant medical or health professional, see RSPM 5.2. Restrictive interventions cannot be applied without APO approval. The Office of the Senior Practitioner must be provided with a copy of the approved BSP within two working days. Staff must not apply any intervention which may cause restriction without approval from the APO. The BSP guidelines available from the Office of the Senior Practitioner should be used to assist BSP development. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.3 – 5 Emergency use of restraint and seclusion Section: 147 of the Disability Act 2006, directs the circumstances whereby restraint and seclusion may be used in an emergency situation on a resident who does not have an approved BSP that provides for the use of restraint and seclusion. For example, doors may be locked in a one-off emergency where a resident is engaging in behaviour which is placing co-residents and staff at risk. Locking the doors ensures the safety of the parties involved. Emergency restraint and seclusion can only be used if the approved disability service provider believes: there is imminent risk of the resident causing serious physical harm to themselves or others and the conditions for use of emergency restraint or seclusion have been satisfied it is necessary to use restraint or seclusion to prevent such risk. In these cases, the following conditions apply: the use and form of restraint or seclusion must be the least restrictive possible, given the circumstances the use of restraint or seclusion must be authorised by the person in charge the APO must be notified without delay of the use of restraint or seclusion the manager must be notified of the intervention, including after hours. The Restrictive Interventions Data System (RIDS) is the tool which must be used to report restrictive interventions. RIDS must be completed monthly and forwarded to the APO. If interventions are not used, a nil-return must be lodged. The APO is required to report to the Office of the Senior Practitioner the use and form of restrictive interventions for the service outlets in which they are responsible. The APO is also responsible for ensuring returns are completed, as required, and forwarded to the Office of the Senior Practitioner within seven days of the end of each month. Staff should ensure they: participate in the development of support plans and BSP’s implement tasks and activities outlined in resident support plans including PCAS follow the directions of the approved BSP do not apply restrictions which have not been authorised, see RSPM Preface, 1.2, 4.2 attend training to ensure the health and safety of: – the resident to which the restriction is to be applied – colleagues – themselves document the use of interventions, as required are familiar with RSPM Section: 1.2: Duty of care in residential services report concerns to their supervisor or manager. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.3 – 6 The role of the supervisor and manager Resources Supervisors and managers must ensure assessments and documentation are completed. This requirement will assist the APO to determine if the proposed restraint or seclusion is the least restrictive option. If a resident is subject to restrictive interventions, supervisors and managers must ensure: the approval is current the restriction is implemented as per the approved BSP the restriction is recorded appropriately, as applied the restriction is reported as directed by the Office of the Senior Practitioner concerns regarding the use of the intervention are documented staff, including casuals, who are required to implement the restraint or seclusion described by the BSP, are trained in inclusive communication strategies and have refresher training, as recommended staff training needs are referred to regional Learning and Development Coordinators. Where locked doors are in place, and it is not considered a restrictive intervention as outlined in this instruction: the Disability Accommodation Services manager must confirm it is the least restrictive option for the resident involved and co-residents strategies must be in place to reduce the impact on co-residents written approval must be provided and reviewed every 12 months by the Disability Accommodation Services manager for the locked door practice to continue Where the use of bed side rails is in place and is not considered a restrictive intervention as outlined in this instruction, the APO needs to sight evidence to be satisfied the bedding system has been prescribed for a therapeutic purpose and not as mechanical restraint. This evidence may include: an assessment tool report and recommendations. Office of the Public Advocate (OPA) – protects and promotes the rights of people with a disability, see: http://www.publicadvocate.vic.gov.au Office of the Senior Practitioner – oversees, and provides information and resources on, the use of restrictive intervention and compulsory treatment. Available on the Department of Human Services website: http://www.dhs.vic.gov.au/for-individuals/your-rights/offices-protectingrights/office-of-the-senior-practitioner Senior Practitioners direction on physical restraint – The direction from the Senior Practitioner on the prohibition of physical restraint. Available on the Department of Human Services website: http://www.dhs.vic.gov.au/aboutthe-department/documents-and-resources/reports-publications/physicalrestraint-direction-paper-senior-practitioner Restrictive Interventions Data System (RIDS) – the system for reporting the use of restrictive interventions. Available on the DAS Hub Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.4 – 1 7.4 Behaviour Support Plans Issued: August 2012 Applies to all Contents What is a Behaviour Support Plan? What are behaviours of concern? Developing an authorised BSP Before lodging a BSP with the APO for approval To ensure a BSP can be implemented Review of an authorised BSP Role of the supervisor and manager Role of support staff Resources What is a Behaviour Support Plan? A Behaviour Support Plan (BSP) is a plan which is developed within the Positive Behaviour Support framework and: specifies a range of strategies when supporting a resident to alter their behaviour reduces the risk of harm. The plan includes proactive strategies to build on a resident’s strengths and increase their life skills. A BSP which has provisions for the use of restrictive interventions must be developed and authorised for implementation in accordance with the directions of the Authorised Program Officer (APO) and Office of the Senior Practitioner (OSP) and be explained to the resident by an Independent Person (IP). Authorised BSP’s are only used where a resident has a behaviour of concern that has not responded to positive behaviour support strategies. The BSP template provided by the OSP is to be used when restrictive interventions are proposed, as this format has been developed to assist with positive behaviour support and compliance requirements. What are behaviours of concern? Behaviours of concern are behaviours which individuals who have a physical, sensory or cognitive disability present with, or are at risk of presenting with, which: are severe dangerous behaviours are not age or culturally appropriate cause serious harm to the individual, others or property without long-term support and intervention will continue to challenge usual support services and potentially form a barrier to the resident’s participation and inclusion in society. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.4 – 2 Developing an authorised BSP An authorised BSP cannot be developed or implemented if the residents’ health and other life areas have not been addressed as far as possible, see RSPM 7.1. This includes any changes that may have occurred in the residents’ life or routines being investigated and appropriate support strategies provided. In addition, a functional behavioural assessment must be completed if: a resident presents with behaviours which impact on their health and safety, or the health and safety of others the known behaviour increases, or alters significantly. The Occupational Violence Risk Assessment Management Tool (OVRMAT) must also be completed, or reviewed, as required. Staff and managers should consult the Office of the Senior Practitioner resources to familiarise themselves with current behaviour support publications and information. Requests for specialist services support must be registered with Client Services Intake, or as per regional processes. Before lodging a BSP with the APO for approval The BSP form must be completed in full to ensure the OSP is: able to register the BSP follow-up queries or concerns. This includes the: resident’s name, address, date of birth, gender and CRIS number address and name of the service provider, for example, the DHS region and regional address details of other disability services which the resident accesses completed and review dates name, date and signature of the APO name of the Independent Person and their relationship to the resident. If the resident has an appointed guardian, this person must be involved and be identified in the BSP as their guardian. Additionally, the BSP must clearly: identify the type of restraint required state the circumstances for which the approved restraint can be used list the least restrictive options to be used first explain the benefits of the intervention. Failure to check and complete these details may result in the BSP not complying with the requirements of the Act. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.4 – 3 To ensure a BSP can be implemented When implementing a BSP it is important: the environment is suitable for the requirements of the plan co-residents receive information and support to ensure their wellbeing and safety, if incidents occur managers refer training needs to regional Learning and Development Coordinators to ensure staff have access to learning and development opportunities which: – develop communication skills with a focus on augmentative and alternative communication strategies (if these are recommended in the communication assessment) is part of a positive behaviour support strategy which includes strategies to address: – communication issues – the safety of staff and others. If the BSP identifies staff require assault response training, this can only occur after positive behaviour support training has been delivered. This requirement must be clearly documented in the resident’s BSP. Review of an authorised BSP Authorised BSP’s must be reviewed within a 12 month period, or at intervals as specified by the APO or OSP. BSP reviews should include those who were involved in the original planning process. A resident may request a BSP review at anytime. Staff should review the BSP at on-going staff meetings to ensure it is: well understood being implemented, as required. Role of the supervisor and manager The supervisor and manager must ensure: authorised BSP’s are in place, as required staff understand their role in implementing BSP’s staff training needs are included in the support information required to implement the BSP staff have access to identified training and refresher training, as required staff training needs are referred to regional Learning and Development Coordinators BSP’s are discussed at staff meetings to ensure they are understood and consistently applied. Role of all staff Generally, staff have the primary responsibility for implementing BSP’s on a day-today basis. It is important staff: participate, as far as possible, in the development of BSP’s raise concerns or queries with the relevant person attend training specific to BSP’s complete necessary documentation as required by BSP’s assist with the reporting requirements of authorised BSP’s are familiar with RSPM Preface, 1.2, 4.2. do not implement any restriction which is not part of the authorised BSP follow the PCAS method of working with residents, see RSPM 4.4. Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.4 – 4 Resources Behaviour Support Plan format and Practice guide. Available on the Department of Human Services website: http://www.dhs.vic.gov.au/aboutthe-department/documents-and-resources/forms-and-templates/behavioursupport-plan-template Occupational violence – policy, implementation guidelines, procedures and tools. Available on the DAS Hub. Occupational violence risk assessment and management – an electronic tool on preventing occupational violence. Available on the DAS Hub. Office of the Senior Practitioner – oversees, and provides information and resources on, the use of restrictive intervention and compulsory treatment. Available on the Department of Human Services website: http://www.dhs.vic.gov.au/for-individuals/your-rights/offices-protectingrights/office-of-the-senior-practitioner Office of the Public Advocate (OPA) – protects and promotes the rights of people with a disability. Available at: http://www.publicadvocate.vic.gov.au Strengthening rights in residential services: Policy statement – an explanation of the policy expectations of residential service providers in relation to residential rights. Available on the Department of Human Services website at: http://www.dhs.vic.gov.au/__data/assets/pdf_file/0010/599122/dis_act_20 06_residentialrightspolicy_pdf_-0610.pdf Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.5 – 1 7.5 Compulsory treatment Issued: August 2012 Applies to all Contents What is compulsory treatment? Changes to treatment plans Resources What is compulsory treatment? Compulsory treatment, residential treatment orders and security orders can only be applied if specific requirements are met. People who are authorised under the Disability Act 2006 to participate in making this determination include: the Secretary of the Department of Human Services the Senior Practitioner Authorised Program Officers the Adult Parole Board the Secretary of the Department of Justice. Any resident who is subject to a compulsory treatment order must have an approved treatment plan. The treatment plan requirements outline the way that staff must support the resident. Changes to treatment plans A change cannot be made to a treatment plan unless it is approved by the Senior Practitioner. The Senior Practitioner cannot approve a change to a treatment plan which relates to an increase in supervision or restriction, except in an emergency. The Victorian Civil and Administrative Tribunal (VCAT) is the only authority which can approve a variation in a treatment plan which involves an increase in supervision or restriction. If the Senior Practitioner approves a change in an emergency situation, they must immediately apply to VCAT for a variation of the treatment plan. Resources Office of the Senior Practitioner – oversees, and provides information and resources on, the use of restrictive intervention and compulsory treatment. Available on the Department of Human Services website: http://www.dhs.vic.gov.au/for-individuals/your-rights/offices-protectingrights/office-of-the-senior-practitioner Victorian Civil and Administrative Tribunal (VCAT) – VCAT deals with a range of disputes, appoints guardians and administrators and has the power to review certain matters under the Disability Act 2006. Available at http://www.vcat.vic.gov.au Access the Disability Accommodation Services Hub to ensure the most up to date information is used Residential Services Practice Manual 3rd Edition – 7.5 – 2 Access the Disability Accommodation Services Hub to ensure the most up to date information is used