Expression of Dicer in breast cancer and its association with

REPORT FOR PATHOLOGICAL SOCIETY SMALL GRANT SCHEME
AWARD: GRANT REFERENCE NO. SGS 2011/010/16
Title: Expression of Dicer in breast cancer and its association with molecular subtypes, biomarker expression and patient outcomes
Name & Address: Emer Caffrey, Discipline of Pathology, National University of Ireland Galway, Clinical Science Institute, Costello Road, Galway, Ireland.
Background: Dicer is a key enzyme in the biogenesis of microRNAs, a class of short non-coding RNA molecules which negatively regulate mRNA translation. MicroRNAs regulate diverse biological processes including proliferation, apoptosis and differentiation. A global reduction in microRNA biogenesis due to downregulation of Dicer has been associated with several tumour types including breast cancer. Reduced Dicer expression is associated with poor patient survival in certain tumours including lung and
appears that the effects of Dicer may be oncogenic or tumour-suppressive in a context-dependent manner. Deregulated expression of Dicer has been documented in a substantial population of invasive breast cancers. Reduced expression has been associated with epithelial-mesenchymal transition, more
clinically aggressive subtypes and hormone receptor negativity.
studies have associated reduced Dicer expression with poor patient survival, 5 others have not.
7
In order identify specific anti-Dicer antibody we tested several commercially available antibodies for immunohistochemistry using FFPE sections from human breast tissue. We observed specific staining for Dicer with anti-Dicer antibody from Clonegene (13D6R). Next we performed study of Dicer staining in 26 whole tissue sections of breast tumours. Staining intensity was evaluated in comparison to normal luminal cells, and reduced intensity was seen in 12 tumours. We observed that 50% of ER-positive tumours showed reduced Dicer staining, compared to 25% of ER-negative tumours. However, evaluation of Dicer expression in a larger series of tumours is required for robust statistical analysis. We propose to follow-up our pilot study using the same immunohistochemistry protocol, on a cohort of 857 patients the breast cancer managed at Galway University Hospital.
Original Aims (copied from original application): To evaluate Dicer expression in relation to clinico-pathological parameters and outcomes in breast cancer
1. Confirm the specificity and sensitivity of anti-Dicer antibody (13D6R) by transfecting MDA-MB231 cells with Dicer shRNA, followed by qRT-PCR and western blotting for Dicer.
2. Determine the specificity of the anti-Dicer antibody from Clonegene
(13D6R) in IHC by the pre-incubation with the competing peptide.
3. Carry out Dicer immunohistochemistry on a TMA which has previously been constructed in our Department from a series of 857 breast tumours.
4. Use statistical analysis to correlate staining intensity with clinicopathological variables.
Results : Immunohistochemistry for Dicer using rabbit polyclonal antibody
(Clonegene, 13D6R, 1:2500) was carried out on tissue microarrays constructed from formalin fixed paraffin embedded invasive breast carcinoma samples from a database of 666 breast cancer patients. Benign breast epithelium demonstrated strong Dicer staining in the myoepithelial layer.
Strong cytoplasmic staining was also noted in smooth muscle and neural cells. When present in tumour cells, staining was located in the cytoplasm.
Occasional nuclear staining was seen in cases with moderate or strong intensity cytoplasmic staining. Staining of the tumour stromal cells was frequently observed, with or without tumour cell positivity.
The specificity of the antibody was confirmed by pre-incubating Dicer antibody with an excess its competing peptide (Clonegene) for 72 hours and testing on whole breast tissue sections. Dicer antibody without addition of blocking peptide was run simultaneously under the same conditions. Addition of blocking peptide eliminated staining confirming the specificity of the antibody
(Figure 1).
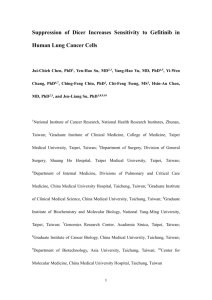
Dicer expression was double-scored based on overall cytoplasmic staining intensity in tumour cells. Negative cases showed absence of staining, positive cases showed weak (score 1), moderate (score 2) or strong (score 3) staining intensity (Figure 2). 145/446 (33%) invasive breast carcinomas, 44/128 (34%) cases of DCIS and 58/101 (57%) lymph node metastases were positive for
Dicer.
Dicer expression in invasive carcinoma will be compared with clinicopathological features using chi-square tests and two-proportion tests.
Survival comparisons for dicer expression will be assessed using Kaplan
Meier estimates and log-rank tests. Associations between Dicer expression and outcome will also be analysed in patient subgroups. Using a Cox
Proportional Hazards model, all clinicopathological variables will be evaluated in a multivariable survival model. The findings will be submitted for publication in a peer-reviewed journal.
Conclusions: Specific immunohistochemical expression of Dicer was demonstrated using Clonegene 13D6R antibody. Benign breast epithelium demonstrated strong Dicer staining in the myoepithelial layer. Dicer expression was observed in 34% of invasive carcinomas in this cohort.
How Closely Have the Original Aims been Met: We have met our aim to investigate Dicer expression in breast cancer. Firstly, we confirmed the specificity of the anti-Dicer antibody by pre-incubation with the competing peptide. As this experiment was successful, we did not pursue transfection of cells with Dicer shRNA. Next, Dicer immunohistochemistry was carried out on tissue microarrays from a large cohort of breast cancer patients. Cases were categorised based on cytoplasmic staining intensity. Dicer expression is currently being correlated with clinicopathological variables and outcomes.
Figure 1. Dicer immunohistochemistry with and without pre-incubation with antibodyblocking peptide in benign breast tissue. A: Dicer staining pattern without peptide block demonstrating strong expression in the myoepithelial layer. B: Addition of blocking peptide resulted in absence of staining.
A B
C D
Figure 2.
Representative images of Dicer expression scores in invasive carcinoma on TMAs. No staining (A), weak cytoplasmic staining (B), moderate cytoplasmic staining (C) and strong cytoplasmic staining (D) correspond to scores 0, 1, 2, and 3.
References
1. Karube Y, Tanaka H, Osada H et al.
Reduced expression of Dicer associated with poor prognosis in lung cancer patients. Cancer Sci 2005; 96 ;111-115.
2. Merritt WM, Lin YG, Han LY et al.
Dicer, Drosha, and outcomes in patients with ovarian cancer. The New England journal of medicine 2008; 359 ;2641-2650.
3. Faber C, Horst D, Hlubek F, Kirchner T. Overexpression of Dicer predicts poor survival in colorectal cancer. Eur J Cancer 2011; 47 ;1414-1419.
4. Chiosea S, Jelezcova E, Chandran U et al.
Up-regulation of dicer, a component of the
MicroRNA machinery, in prostate adenocarcinoma. The American journal of pathology
2006; 169 ;1812-1820.
5. Grelier G, Voirin N, Ay AS et al.
Prognostic value of Dicer expression in human breast cancers and association with the mesenchymal phenotype. Br J Cancer 2009; 101 ;673-683.
6. Blenkiron C, Goldstein LD, Thorne NP et al.
MicroRNA expression profiling of human breast cancer identifies new markers of tumor subtype. Genome biology 2007; 8 ;R214.
7. Martello G, Rosato A, Ferrari F et al.
A MicroRNA targeting dicer for metastasis control. Cell 2010; 141 ;1195-1207.