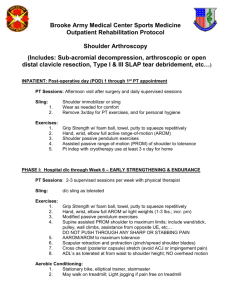
Shoulder protocol
advertisement

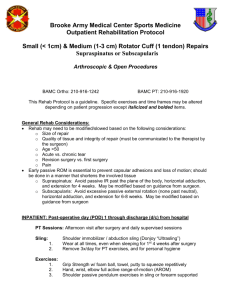
Physiotherapy-protocol for shoulder surgery (Based on Neer’s protocol – 1990: tissue healing > mobilisation> muscle strengthening) Hospital patient – pre-operative Evaluate the patient: objective – ROM and muscle strength; subjective - pain Comfort the patient regarding stiffness and pain post-surgery. Information regarding sling (put on; take of; and other advice). Demonstrate as far as possible. Nowadays sling have abduction pillow and ball for circulation exercises. Inform about portovac drain and IVI connected to PCA-pump. (pain controlled analgesia) Short explanation regarding physiotherapist’s role post-operatively. Explain the use of the CPM if it is part of the protocol. Information brochure: Better to wear shirt with buttons during wear of sling. Allowed to shower if wound clinic allows it, otherwise wait for removal of stitches. Must wash and dry properly in axilla. When washing or showering the sling may be taken off, but hold the arm close to the body as far as possible. Do not stretch forward or lift the arm. Not allowed to drive until the doctor allows it. Whenever the patient comes for out-patient physio, he/she should take the pain medication 30 minutes before the appointment. Bring a family member or friend with to the first physio-session. They can help with the home exercises and this will limit the physio-sessions for the first phase drastically. Put on ice packs at home to relieve pain and swelling. Only start using heat when the physiotherapist allows this. (If it is used too soon it will disturb the haematoma and cause bleeding or worsen the swelling.) Diagrams and all possible exercises during rehabilitation. Length of the expected rehabilitation time: can be 6 – 12 months. It all depends on the severity of the injury pre-operatively. Usually at the end of rehab the pain is completely under control but the ROM will never be quite the same (especially true for TSR). Hydrotherapy information if the facilities are available. Hospital patient – day 1 post-operative (sometimes in case of TSR, only day 5) If not able to see the patient pre-operatively, subjective evaluation regarding pain, ROM and muscle strength. Give all the info as you would have pre-operatively. Organise with the nursing staff for pain medication 30 minutes before treatment / PCA pump. Exercises: (hold for 5 seconds, start with 3-4 reps only) Pure passive shoulder flexion, stop where discomfort starts – aim for 90º. Pure passive shoulder abduction, stop where discomfort starts – aim for 90º. Pure passive shoulder abduction, stop where discomfort starts or up to prescribed pre-caution. (Upper arm on a small towel roll, to be in line with the spine and the shoulder in a comfortable position.) Circulation exercises and maintain ROM of the elbow, wrist and fingers. Maintain neck ROM. Exercise to put on and remove the sling. Advice regarding ice pack for pain. Make a follow-up appointment. Outpatient - for ±4-6 weeks (for as long as passive movements are prescribed) Scapular passive movements. All the passive movements as was done in the hospital, but teach it to the patient as well (use a broom stick or the other arm; a shorter lever is better at the start). Teach the abovementioned exercises to the patient’s family member or friend in order to limit the outpatient visits during this phase. Exercises done 3-4 times per day, 5- 10 reps guided by pain.) Neck and thoracic mobilisations for stiffness and pain. (Thoracic also as home exercise with towel roll in supine.) Neck and thoracic massage for pain relief muscle spasm relaxation. Continue with hand and elbow exercises for circulation and maintenance of ROM. US; laser and TENS for pain relief and promotion of wound healing. Scapular stabilisers facilitation and activation. Rotator cuff activation. Crio therapy at home after treatment for pain and swelling and heat only when the physiotherapist allows it. Some surgeons will allow pendulum (Codman) exercise at this stage. Do it for 60 seconds per movement / 10 repetitions. May start doing the passive movements in standing at the end of this phase, using the broom stick (include shoulder extension). Some surgeons will allow isometric exercise at the end of this stage. Physiotherapist follow-up: weekly/fortnightly/monthly (depending on the patient’s self discipline and financial situation). Hydrotherapy can also be done during this phase if the facilities are available. Exercises should be done very slowly and controlled, the water is there for support and no resistance whatsoever. Maintain a good posture and give appropriate exercises – the pain and the sling will sometimes cause a kyphotic posture. Outpatient – start with active exercises (sling is off) All ranges active assisted active: pulley towel exercise wall climb with fingers hold onto wall/wall rack and flex knees hands behind head and move elbows outwards Strengthening with theraband (progress from light to heavy). Proprioception exercises (balance board; aerex; trampoline – ball throw and push-ups; bottle half filled with water). Monitor posture. Monitor neck and thoracic spine. Monitor pain. Complete scapular stabilisers rehab. Outpatient – sport/function specific Final rehab regarding mobilisation; strengthening (stabilisers included) and proprioception.