Open Access version via Utrecht University Repository
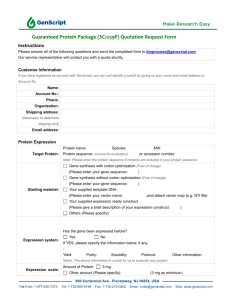
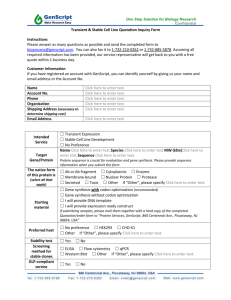
advertisement

Regenerating an Immune System: Gene Therapy and Stem Cell Transplantation for Severe Combined Immune Deficiency Brooke LaTour Studentnr. 3729451 Supervisor: Dr Frank Staal Leiden University Medical Center Utrecht University Examiner: Dr Andries Bloem Immunity & Infection, Graduate School of Life Sciences 2012-2013 Table of Contents I. Introduction 2 B-Cell Associated Immunodeficiences 2 Phagocytic Immunodeficiences 6 Combined Immunodeficiencies 6 II. T-Cell Lymphopoiesis in Health and Disease 7 III. Molecular Causes of SCID 10 Defective common chain cytokine signaling associated SCID 10 Adenosine deaminase deficient SCID 12 Defective V (D) J recombination associated SCID 13 Defective pre-TCR/TCR signaling associated SCID 14 Genetically similar, symptomatically divergent 15 IV. Current Therapy 15 V. A History of Progression 18 Major setback: T-ALL due to insertional mutagenesis VI. VII. Gene Therapy and Toxicity: The Evolution of Vectors 20 21 Retroviral Vector Insertional Mutagenesis in Gene Therapy 23 The Role of LMO2 in T-Cell Development 26 Patterns of Viral Integration 26 Predicting Genotoxicity: Animal Models 28 Future Treatments Genomic editing 30 32 VIII. Discussion 37 IX. References 41 1 I. Introduction Primary immunodeficiencies (PIDs) are a subset of immunologically based, inherited diseases that predispose affected individuals to a variety of infections, allergies, and autoimmune disorders, and leave them at risk of developing cancer. PIDs provide an invaluable model to dissect intrinsic mechanisms of the human immune system. Examination of these mostly monogenic conditions has lead to the identification of many of the associated genes and has produced a wealth of information about the development and function of the immune system. These pathologies give rise to immunological insights on the regulatory and genetic complexities of the innate and adaptive immune system and allow for the accreditation of scientific observations to underlying genotypes. Critical analysis and understanding of these disorders is essential as it fosters the development of new diagnostic and therapeutic tools for improved treatment of a wide variety of pathologies. B-cell associated primary immunodeficiencies Multiple PIDs exist that arise from impairments in early B-cell development (Figure 1). Mutations that prevent signaling via the pre-B-cell receptor (BCR) lead to an absence of mature B-cells and consequently a lack of immunoglobulins. Studies of these disorders have elucidated information on the process of normal B-cell differentiation. Development of a mature and functional antibody repertoire occurs via stochastic recombination, during which B-cells express rearranged immunoglobulin heavy (IgH) () and light (L) genes 1, and response to antigen engagement, which initiates Ig class switch recombination (CSR) and the generation of somatic hyper mutations (SHM). These two major antibody maturation events require close contact with T-cell 2. Following these processes, selection of B-cells 2 expressing functional non-autoreactive B-cell receptors (BCR) is initiated, resulting in the generation of mature B-cells with a high affinity for antigen. The majority of genetically characterized abnormalities that result in a lack of mature B-cells involve defective signaling through the pre-BCR. Of these, approximately 85% of patients that present with early onset recurrent bacterial infections, hypogammaglobulinemia, and abnormally low levels of B-cells have mutations in the X-chromosome encoded cytoplasmic Bruton’s tyrosine kinase (BTK) 3. BTK, a member of the Tec family of tyrosine kinases, plays a central role in B-cell signaling, development, and differentiation 4. Mutations in BTK result in Xlinked agammaglobulinemia (XLA). Other genetically defined cases of agammaglobulinemia are caused by mutations in the heavy chain, Ig, the 5 component of the pre-BCR surrogate light chain, or the B-cell adaptor protein BLNK (also known as SLP65) (reviewed in 5) because these elements are necessary to proceed past the pre-B stage during B-cell lymphopoiesis. The phenotype of these disorders differs profoundly between species. For example, substantial differences have been observed between the xid mouse model, which carries a defective BTK allele 6 and XLA patients. XLA patients fail to produce antibodies in response to vaccination, have substantially low levels of all immunoglobulin isotypes, and have less than 1% of normal B-cell numbers. In comparison, xid mice are able to generate an antibody response to most T-cell dependent and some T-cell independent antigens. They exhibit very low serum levels of IgM and IgG3 but have almost normal concentrations of IgG1, IgG2a, IgG2b and they have approximately half the normal amount of B-cells. It is interesting to note that defects in pre-BCR signaling generally elicit a much more severe phenotype in humans than in mice. Mutations in 5 and BLNK results in a block of early B-cell differentiation in both human and mice, however disruption of the gene encoding Btk only causes a developmental block in humans. This strongly suggests that there are differential needs for B-cell development between species. Further support of this point is underscored by the fact that mutations in the interleukin-7 receptor (IL-7R) cause a complete abrogation of B-cell differentiation at the pre-B 3 pro-B stage in mice 7, 8 whereas a lack of IL-7 signaling in humans, as seen in specific types of severe combined immunodeficiency (SCID), results in the absence of T-cells and a normal or elevated number of immature B-cells. These distinctions illustrate important species-specific criteria for B-cell development and highlight the complexities of interspecies translational models. Common variable immunodeficiencies (CVID), or acquired hypogammaglobulinemia, is a collection of primary immune deficiencies characterized by low serum levels of IgG, IgA, and/or IgM (reviewed in 9) with varying underlying genetic causes. Unlike other PIDs, CVID generally presents around the patient’s mid-20s but can manifest as late as the fourth decade of life 10. While several genetic lesions have been identified, the majority of causational biochemical and genetic abnormalities remain unknown. Mutations in which the inducible T-cell costimulator (ICOS) protein and B-cell expressed CD19 are disrupted account for approximately 1% of CVID cases. Most patients have altered B-cell subsets, which indicate impaired B-cell differentiation. While specific response to antigen is severely attenuated, detectable levels of autoantibodies and autoreactive B-cells can be found 10. Also characterized by low immunoglobulin levels, hyper IgM (HIGM) syndrome is an amalgamation of several closely related but genetically divergent disorders affecting B-cell development. It is characterized by defective immunoglobulin CSR and consequently very low levels of IgG, IgA, and IgE. HIGM syndrome led to the discovery that the collaboration of B and T-cells, via CD40/CD40L interaction, in response to antigen recognition is required for CSR to take place. T-cell surface protein CD40 ligand (CD40L also known as CD154) is necessary for germinal center (GC) formation in lymphoid organs, which is the site where B-cells interact with T-cells and undergo CSR. This finding was further accredited by the discovery that mutations in the gene encoding CD40 results in the inability of B-cells to undergo CSR 2. An intrinsic defect of B-cells is also observed in HIGM syndrome. Utilizing genetic linkage analysis it was identified that a subset of HIGM is caused by mutations of AICDA, the gene encoding the enzyme activation induced deaminase (AID). In the absence of this enzyme, B-cells fail to undergo CSR 4 and are defective in their ability to generate somatic hyper mutations (SHM) in the variable (V) segment of the immunoglobulin genes 11. Knowledge of this resulting defect firmly linked the CSR and SHM events which both occur in the GC at approximately the same time in B-cells development. Figure 1: Primary Immunodeficiencies affecting B-cells development. Self-renewing HSCs exist at the apex of the hematopoietic hierarchy. They have the capacity to differentiate into lymphoid or myeloid progenitors. CLPs are the precursors of the lymphoid branch. They can divide to form Tcells, NK-cells and B-cells. Developing B-cells progress through a series of discrete stages to become mature B-cell, in this diagram they are simplified into the Pro B, Pre B, and B-cell steps. Stages at which the specific aforementioned PIDs arise are indicated. Affects on each isotype of immunoglobulin are indicated in the table below the schematic diagram. Abbreviations are as follows: HSC, hematopoietic stem cell; CLP, common lymphoid progenitor; BLNK, B-cell linker protein; XLA, X-linked agammaglobulinemia; BTK, Bruton’s tyrosine kinase; CVID, common variable immunodeficiency; ICOS, inducible T-cell co-stimulator; HIGM, hyper IgM syndrome; AICDA, activation-induced cytidine deaminase; UNG, uracil-N-glycosylase; AICDA C, deletion of the Cterminal end of AICDA 16. AID acts on DNA to deaminate cytosine to uracil in immunoglobulin genes 12 and recently it was demonstrated that uracil residues are generated in immunoglobulin genes within 24 hours of B-cell stimulation 11. Uracil-N- glycosylase (UNG) is a DNA repair enzyme that acts cooperatively with AID to assist in shaping the specificity of AID induced SHM 13. Loss of function recessive mutations of UNG are associated with substantial impairment in CSR at a DNA precleavage step and with partial distruption of SHM, these findings support the model that AID directly deaminates cytosine into uracil in the switch (S) and variable (V) regions of 5 immunoglobin genes 14. An analysis of HIGM syndrome phenotypes lead unexpectedly to the discovery that certain mutations of AID result in a nearly normal frequency of B-cell SHM but impaired CSR 15. This phenotype was associated with mutations in the 8-17 C-terminal residues of AID, suggesting that the Cterminus is required for CSR but not SHM. This is most likely due to cofactor binding or recognition of specific conformations of the DNA immunoglobulin S region 16. Phagocytic immunodeficiencies Engulfment and destruction of invading pathogens by phagocytosis plays an indispensible role in the innate immune response. Phagocytes also serve to clear apoptotic bodies and other cellular debris during tissue homeostasis and remodeling. There are several congenital disorders that hamper phagocytic function (reviewed in Flannagan et al., 2012). Phagocytic disorders can be divided into intrinsic and extrinsic based disorders. Extrinsic factors that are impaired in phagocytic deficiencies include opsonic abnormalities, impaired antibody function, and defective complement factor activity. These issues can lead to severe neutropenia via suppression of granulocyte production or autoantibodies directed again host neutrophils. Intrinsic defects can result from impaired granulocyte development or exit into peripheral circulation. They can also be the effect of impaired granulocyte killing ability or chemotaxis. Examples of intrinsic disorders associated with impairment in phagocytic killing include chronic granulomatous disease, glycogen storage disease type Ib, Chediak-Higashi syndrome, and specific granule deficiency. PIDs associated with deficiencies in chemotaxis include hyper-IgE syndrome, leukocyte adhesion defects, Shwachman-Diamond syndrome, and syndromes with periodontitis. Combined immunodeficiences SCID is a heterogeneous disorder characterized by the aberrant development and/or functional of T-lymphocyte. It often is fatal during the first few months of life due to severe and recurrent infections unless transplantation of hematopoietic stem cells (HSCs) restores the functional T cell compartment of the immune system. 6 Clinical manifestations of SCID, despite its wide range of underlying causes, share several phenotypic characteristics including failure to thrive, extreme susceptibility to infections, significant lymphopenia, a complete absence of T-cells, and reduced thymic size and capacity17. The presence of B-cells is variable in different subtypes of SCID, however even when B-cells appear in normal number, they have intrinsic defects in addition to the impairments they suffer due to the absence of T-cells. As previously noted, the lack of T and B-cell interaction results in immature B cells that cannot undergo CSR and consequently cannot produce antibodies in response to antigens 2. II. T-Cell Lymphopoiesis in Health and Disease PIDs have propagated a myriad of information about immune development and function. Critical species-specific differences in T-cell lymphopoiesis exist which create challenges in deriving translational knowledge of human T-cell development from mouse research. SCID, due to its characteristic, genetically determined blocks in T-cell differentiation, has created the circumstance for modeling human T-cell differentiation and function. These conditions have also revealed several nonredundant roles for cytokines and cytokine signaling molecules in human lymphopoiesis. Moreover several interspecies dissimilarities in cytokine signaling pathways have been elucidated via the comparison of human and mouse SCID phenotypes. Cytokines are paracrine factors that are classified as type I or II based on three-dimensional structure. A shared feature of both types of cytokines is that, with few exceptions, their associated receptors lack intrinsic tyrosine kinase capacity so signaling is accomplished through the Janus-activated kinase (JAK)/ signal transducer and activator of transcription (STAT) pathway (reviewed in 18). Mutations that interfere with these signaling pathways result in deficiencies in select hematopoietic cells types. 7 Figure 2: Differential phenotypes of T-cell development in the human versus mouse thymus. During normal T-cell development, T-cell precursors migrate through different specialized regions of the thymus. Different definitive phenotypic markers demarcate stages of T-cell development in humans and mice. The main checkpoints associated with human T-cell development are indicated. DN, double negative; ISP, immature single positive; DP, double positive; SP, single positive19 During physiologically normal human T-cell development (Figure 2), T-cells arise from pluripotent progenitors cells in the bone marrow or fetal liver and migrate to the thymus in order to differentiate. It is through a complex and highly regulated process that a diverse and effective mature T-cell population is generated and sustained. Naïve, single positive T-cells develop from thymocytes in the specialized microenvironment of the thymus20. Maturation of T-cells requires controlled rearrangement of the different T-cell receptor (TCR) genes to assemble diverse TCR-complexes, this process is mediated by recombinase activating genes (RAG) 1 and 2. It is important to note, that because RAG1 and 2 are also responsible for the rearrangement of immunoglobulin gene segments in B-cells, mutations in either gene results in an absence of mature T and B-cells. T-cells that recognize foreign antigens in association with the self-major histocompatibility complex (MHC) are positively selected for survival, while autoreactive T-cells are eliminated via negative selection. Positive and negative selection events culminate in the expression of mature TCR molecules. 8 T-cells progress through a series of discrete stages of development, characterized by loss of potential for alternative lymphoid fates, that can be discerned via the expression of membrane associated clusters of differentiation (CD) such as CD4 and CD8 (Figure 2). The TCR lineage bifurcates from the TCR lineage in murine models around the double negative (DN) 1 and DN2 subsets. In human T-cell development TCR loci rearrangement begins around the DN1-DN2 stage when cells are at the immature CD34+CD38-CD1a-stage. TCRB rearrangement occurs as soon as cells acquire expression of CD38. At the DN stage, pre-T-cells are CD4 and CD8 negative. For murine thymocytes, there are 4 DN stages defined by the gradual loss of CD34 and gain of committed T-cell associated genes; these stages are defined by differential expression of CD44 and CD25. In humans there are 3 heterogenous subsets of the DN stage: the most immature being the CD34+CD38CD1a-stage, followed by the expression of CD38, and then finally CD1a expression 21 ,TCR selection occurs during this final DN stage. Only a few T-cell progenitors enter the thymus per day, but once they have migrated to this new environment they proliferate exponentially due to specific cytokine exposure, during the DN1 and DN2 stages of development (reviewed in 22). By DN3 cells cease to proliferate and undergo rearrangement of the TCRB locus 21. In mice TCRD rearrangement begins in the DN1 stage followed by TCRG and TCRB in the DN2, TCRB rearrangement continues in the DN3 stage. The discrete human stages resemble murine Tlymphopoiesis as follows: murine early DN1 (CD44+CD25-CD117-) corresponds to the human CD34+CD38-CD1a- stage. The murine late DN1/DN2 (CD117+/CD44+CD25+) and DN3 (CD44-CD25+) correspond the human CD34+CD38+CD1a- and CD34+CD34+CD1a+ respectively (Figure 2). During the progression from DN3 to an immature single positive T-cell there is surface expression of the TCR chain with the pre-TCR chain and together these chains make up the pre-TCR complex. During this period the functional ability of the mature TCR chain is tested, this process is known as -selection. At this time, activation of the pre-TCR complex induces proliferation and initiates rearrangements of the TCRA gene. It is at this point that the thymocyte expresses 9 both CD4 and CD8. Productive rearrangement results in the expression of the mature TCR complex, which then allows these lymphocytes to undergo the process of positive and negative selection. If the cell survives selection it matures into a naïve CD4 or CD8 single positive T-cell. TCR signaling is critical for T-cell development and lineage specification. Tcell homeostasis plays a central role in maintaining proper immune function. Patients that present with the presence of a mature but non-functional T-cell repertoire share several common features including impairment in positive and negative T-cell selection, high levels of lymphocyte specific apoptosis resulting in lymphopenia, susceptibility to viral and bacterial infections and high incidences of autoimmune manifestations. The study of rare T-cell associated PIDs provides insights not only into T-cell development but also in the molecular and biochemical pathologies of other disorders. A novel form of SCID defined by a bi-allelic loss of function mutation in the ZAP70 gene was first described in Mennoite Indians that presented with a selective depletion of CD8+ lymphocytes. ZAP70 is a TCR associated tyrosine kinase necessary for signaling TCR activation. These individuals had detectable CD4+ T-cells in circulations but these cells failed to respond to CD3+ cross-linking. In mice, the phenotypic manifestation of a lack of functional ZAP70 results in a differentiation block at the DP stage of T-cell development, interestingly development of TCR+ T-cells is unaffected (reviewed in 23). III. Molecular Causes of SCID Defective common chain cytokine signaling associated SCID There are at least 15 different underlying genetic causes of SCID 24. X-linked SCID (SCID-X1) is the most common form of SCID accounting for approximately 50% of cases 25 (Figure 3). Its underlying genetic cause is attributed to a deficiency in the cytokine receptor common chain (c) also referred to as the Interleukin-2 receptor chain- (IL-2R). There have been hundreds of mutations described in the c gene that are causative of SCID 26. The c chain is an essential subunit of several 10 cytokine receptors, including IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21 27. IL-7 receptor signaling is indispensible for development, survival, and proliferation of mature human T-cells. It is known that IL-7 is essential for T-cell development because mutations in the gene encoding the -chain of the IL-7 receptor lead to an absence of T-cells, but the retained presence of B and natural killer (NK)-cells 28. The phenotypic lack of NK-cells associated with SCID-X1 is attributed to defective IL15/IL-15R interaction 29, 30 as murine models have demonstrated that the absence of IL-15 or IL-15R leads to a phenotypic lack of NK-cell. A notable immunological difference between humans and murine models is that c mutation in humans leads to a form of SCID marked by the absence of T and NK cells, while in mice this same mutation results in an animal completely devoid of lymphocytes demonstrating the fact that c signaling is not required for B-cell development in humans but is essential for proper B-cell development in mice. This could be attributed to the fact that murine B-lymphopoiesis, as previously mentioned, is dependent upon IL-7/IL7R signaling (reviewed in 18). A symptomatically indistinguishable form of SCID can also result from mutations in the JAK3 gene 31 because the JAK3 tyrosine kinase is functionally coupled to cytokine receptors that utilize the c chain. In order to signal interleukin receptors, which lack intrinsic catalytic activity, require the c chain to associate with the intra-cytoplasmic tyrosine kinases JAK1 and JAK3 32. At least 23 unique mutations have been identified in different structural domains of the JAK3 gene that contribute to the formation of SCID. Dysfunction or absence of c chain associated signaling results in a block in T and NK lymphopoiesis leading to compromised immune development. B-cells are present in normal or high numbers, but are not functional. 11 Figure 3: Relative distribution of SCID subtypes. Data obtained from 33,34 Adenosine deaminase deficient SCID Adenosine deaminase (ADA) deficient SCID is the second most common form of SCID (Figure 2). It is an autosomal recessive metabolic disorder that affects multiorgan systems. The ADA enzyme plays a central role in purine metabolism and its absence results in the accumulation of the toxic metabolite, deoxyadenosine triphosphate (dATP). Build up of adenosine and deoxyadenosine causes an accretion of cellular dATP, which triggers cell death by apoptosis 33. The buildup of toxic metabolites severely compromises hepatic, skeletal, and neurological function 12 35. Because lymphocyte precursors are extremely sensitive to the toxic build up of dATP, lack of ADA leads to an absence of T, B, and NK cells. Valerio and colleagues characterized that this form of was due to the presence of an aberrant form of the ADA protein, suggesting that the lack of ADA activity is not attributable to transcriptional or translation defects but instead to changes in the configuration of the protein that affect it enzymatic capacity 36. This disease is almost always fatal by year 2 of life if not treated with immune reconstitution therapy (Giblett et al., 1972 republished 37). These patients can also be sustained on pegylated ADA enzyme replacement therapy (ERT). Defective V (D) J recombination associated SCID The third most common type of SCID is caused by recombination defects in any of three genes involved in this process. Variable, diverse, joining V (D) J recombination ensures somatic diversification of immunoglobulin and TCR genes and is an essential part of both B and T-cell differentiation. V (D) J recombination is initiated by Rag1 and Rag2. The Rag1 and Rag2 complex creates nicks between the V, D, J coding elements of the TCR and BCR genes. These nicks are converted to double stranded DNA breaks, which form hairpin sealed coding ends and blunt signal ends (reviewed in 38). Mutations in either RAG1 or RAG2 result in impaired V (D) J recombination and incomplete B and T cell differentiation. In this form of SCID NK development is spared. Another assortment of mutations that impair V (D) J recombination can occur in proteins involved in the non-homologous end joining repair (NHEJ) pathway. The NHEJ machinery is responsible for joining the two coding ends that result from the double stranded DNA breaks. Mutations in the endonuclease protein Artemis cause hypersensitivity to DNA double-strand breakinducing agents, like ionizing radiation, and an absence of T and B cells due to the inability to repair DNA breaks 39. Mutations in DNA ligase IV, another NHEJ protein, result in a partial T+ B-cell SCID-like immunodeficiency 40. Absence of functional DNA ligase IV leads to a substantial reduction in the number of B-cells due to an incomplete but substantial block in early B-cells differentiation, and a 10-fold reduction in the number of T-cells but patients had normal numbers of T-cells 13 41. SCID Phenotypes characterized by very low levels of B-cells and a complete absence of T-cells have also been described for mutations in the gene encoding DNA ligase IV 42. Figure 4: Blockades in lymphopoiesis at different stages manifest as different subtypes of SCID. Vertical arrows indicate the approximate stage where lymphopoiesis is block in each condition. ADA deficiency results in an absence of mature B, T, and NK cells. Mutations in the genes encoding the c chain or JAK3 result in a lack of T-cells and NK cells. Mutations in CD45 and the associated subunits of CD3 prevent pre-TCR/TCR signaling and result in an absence of T-cells. Mutations that interfere with V (D) J recombination, such as RAG1, RAG2, or Artemis lead to a deficiency of B and T cells. Adapted from33 Defective pre-TCR/TCR signaling associated SCID The TCR complex is made up of the and or the and variant chains. These chains pair as heterodimers in association with the invariant CD3 associated chains, CD3, CD3 , CD3, and CD3. Defective pre-TCR and TCR signaling due to impairments in CD3 associated subunits result in the absence of T-cells. Mutations in the CD45 phosphatase are rare but also result in the formation of the SCID phenotype. Deficiencies in each of the pre-TCR/TCR signaling complex subunits CD3 and CD3 and CD3 and CD3 have been described. For unknown reasons, 14 deficiency in CD3 43 yields a substantially less severe phenotype than those corresponding with CD3 and CD3 mutations 44. Genetically similar, symptomatically divergent Omenn Syndrome (OS) is an autosomal recessive disease that is genetically similar to SCID. Also known as “leaky SCID,” it is characterized by hypomorphic mutations in RAG1 and 2, and often in other genes implicated in the SCID phenotype (reviewed in 45), such as Artemis, DNA ligase 4, c chain, IL-7R, and ADA (Niehues et al., 2010). Partial activation of RAG1 and RAG2 leads to the generation of a small number of T-cell clones. The clinical manifestations of this disease are extremely serious as these patients present with severe susceptibility to infection as seen with classic SCID patients as well as extensive tissue inflammation due to autologous oligoclonal hyper-autoreactive T-helper cell 2 (Th2) lymphocytes. These lymphocytes proliferate extensively due to thymic and peripheral reactivity 46 and create extreme levels of inflammation. Individuals with OS have markedly low to absence levels of immunoglobulins with the exception of IgE, which is present in elevated concentrations. The high levels of IgE are hypothesized to be due to the expansion of Th2 cells (reviewed in 47). Other key symptoms include hepatosplenomegaly, lymphadenopathy, often accompanied by recurrent infections, and alopecia. Rapid diagnosis and intervention is essential as OS is fatal if not treated 47. IV. Current Therapy Hematopoietic stem cell transplantation (HSCT) is the primary therapy used to effectively treat SCID. In most cases transplantation is from an unaffected, HLA identical sibling. However, in the majority of situations HLA matched donors are not available so transplantation from a closely HLA-matched, unrelated donor or a haploidentical (parental) donor may be performed, in such cases of none matched HLA, the grafts must be T-cell depleted. Survival rates post transplantation are 15 significantly lower with haploidentical donor transplantations and symptoms of graft versus host disease, such as severe erythematous rash or chronic liver disease often result from engraftment of maternal T-cells. Partially HLA incompatible transplantation is responsible for a 30% mortality rate within the first year postHSCT 34. Allogeneic transplantation carries significant complications such as graft versus host disease, lack of T cell reconstitution and consequently immune deficiency, engraftment failure, and severe side effects from myelosuppressive chemotherapeutic ablation. The advent of bone marrow transplantation began in 1968, and since then it has been shown to effectively alleviate the adverse symptoms associated with SCID by substantial and sustainable immune reconstitution 48. Despite complications, the cytokine dependent signaling defects seen in SCID foster an optimal situation for allogeneic HSCT, even in the absence of a HLA matched donor. The absence of Tcells or a combined lack of NK and T cell substantially reduces possibilities of grafts versus host disease. Because of this, individuals with SCID cannot reject grafts 48 so prior conditioning is not required. It has, however in cases of ADA SCID been shown to improve engraftment 49 due to its ability to dissolve bone marrow from the bone cavity while preserving the thymic niche. New approaches for reconstituting the adaptive immune compartment following HSCT are in development. In most cases of SCID, patients maintain thymic architecture similar to the fetal thymus seen before week 12 of gestation 50. The thymus is made up of primarily undifferentiated epithelial elements, Hassall’s corpuscles, and small blood vessels, and an absence of lymphoid cells. The maintenance of this fetal thymic architecture suggests that migration and differentiation of pre-thymic lymphoid cells are required for the induction of a mature thymus. In a very small number of patients, autopsies or post transplantation thymic biopsies have indicated the present of a normal thymic microenvironment, suggesting that in the presence of lymphoid precursors, the thymus is able to recover and develop normally. Immune reconstitution following HSCT, with T-cell depletion, in SCID patients is 3-6 months, which may in part be 16 due to the need for additional thymic development and thymic niche availability prior to T-lymphocyte generation. In individuals suffering from ADA deficiency, polyethylene glycol-conjugated bovine derived ADA (PEG-ADA) can be used ameliorate symptoms caused by the defects in purine metabolism and minimize the risk of infection associated complications. With PEG-ADA intervention, there is a continuous circulation of enzymatically active ADA available to detoxify adenosine and deoxyadenosine metabolites. PEG-ADA effectively increases the numbers of circulating lymphocytes and level of protective immunity, however the long-term effectiveness of PEG-ADA is not quite as promising. Assessments of patients, ages 5-15 years, treated with PEG-ADA for 5 or more years a decreased lymphocyte count despite the initially observed improvement as well as a gradual decline in mitogenic proliferative response leading to impaired antigenic response. Despite this, in a studying looking at the long term effects of PEG-ADA treat, Chan and colleagues noted that at the time of assessment all patients, despite low B-cell counts, had normal levels of immunoglobulins and were in overall good health 51. These patients will need to be monitored closely to ensure they do not experience further decline in immune function if they continue on this therapy. This research demonstrates ADA therapy can result in a decrease in efficacy with continuous use, which is a major concern with long-term enzyme replacement therapy. Correcting genetic diseases at a DNA level is an attractive option because it alleviates the issues associated with allogeneic transplantation and long term ERT and it restores functional and persistent corrected cell types. It also provides an alternative treatment for individuals without an HLA matched donor, thereby overcoming the immunological barriers associated with HSCT. In standard protocols of gene therapy, HSCs are obtained directly from the patient, corrected ex vivo, and re-infused. SCID represents an excellent model for gene therapy because due to a selective amplification effect of corrected cells, even a low numbers of transgenic cells are capable of reconstituting the immune system. Also alteration of cells via the introduction of a corrected copy of the relevant gene, will not elicit an immunogenic response in the background of SCID. 17 V. A History of Progress Since the initial identification and cloning of genes responsible for human genetic disease, new methods for the introduction of genetic material into mammalian cells have evolved. Early gene therapy trials performed in the 1990s did not produce the revolutionary success initially anticipated but they have laid the foundation for important gene therapy research. ADA deficient SCID was one of the first monogenic diseases for which gene therapy was a possibility because the human ADA gene had been cloned since the early 1980s 52 and the disorder was well characterized both genetically and biochemically 37. In 1990 at the National Institute of Health (NIH) in the United States, two girls with ADA deficient SCID were infused with genetically modified matured Tcells, transduced with a -retrovirus encoding the ADA cDNA 53. Although no complications arose from this procedure, no discernable clinical benefits were achieved. The procedure included several cycles of leukopheresis, transduction of the ADA gene into isolated T-cells, and cell reinfusion. During the procedure the two patients remained on ADA enzyme replacement therapy, which may have negated the selective proliferation advantage to the corrected cells 54. Subsequent trials focused on transference of the ADA gene into a hematopoietic CD34+ progenitor population. While these trials were ostensibly ineffective due to inefficient transduction of target T-cells, continued enzyme replacement therapy, and no ablation prior to transplantation 55, 56, 57, they provided a foundation for improvement in techniques for isolating, genetically modifying, and ex vivo culturing of human HSCs. Vectors were produced at higher titers increasing gene transfer efficiency and cell scaffolding material and cytokines were used in culturing to improved cell survival. In 1999, a gene therapy trial for SCID-X1 was initiated at Necker-Enfants Malades Hospital in Paris, France. SCID-X1 serves as an excellent model for gene therapy, in part because of the potential proliferative advantage conferred to genetically corrected cells. Once functional, cytokine 18 receptors are able to transmit survival and proliferation signals to lymphoid progenitors. This has been corroborated by an unusual event in which a SCID-X1 patient exhibited a spontaneous reversion of a mutant c gene which led to partial and sustained correction of their T-cell deficiency58. In 2000 an ADA deficient SCID gene therapy trials began in Milan, Italy at the San Raffaele Telethon Institute for Gene therapy. The -retrovirus vector was used to stably express ADA in autologous bone marrow derived HSC from SCID patients. A low dose of the chemotherapeutic agent busulfan was utilized prior to HSC reinfusion to ablate the pre-existing marrow and improve engraftment, thereby providing a selective growth advantage to the gene corrected HSCs. The results from the 1999 Paris trial and the 2000 Milan trial were remarkable. Analysis of the first two subjects from each trial showed immunological competence in all four individuals. T-cell counts reached physiologically normal levels and lymphocytes proliferated in response to mitogens and specific antigen stimulation. Immunoglobulin levels were normal and patients no longer suffered from opportunistic infections or immunodeficiency related complications. These two trials were the first to demonstrate significant clinical benefit in treating genetic diseases with gene therapy. Beginning in 2004, in London, England, 10 SCID-X1 children were treated with CD34+ HSCs that had been transduced with the conventional -retroviral vector expressing the c transgene. As in previous SCID-X1 trials these patients received no myelosuppressive conditioning. Upon extended follow up substantial immune reconstitution was observed, notably in 9 out of 10 subjects a polyclonal T cell repertoire was achieved. Humoral immunity was only partially restored as was observable by suboptimal humoral response to antigen stimulation, low levels of immunoglobulin production, and some infection associated complications, despite this some patients were able to discontinue immunoglobulin replacement therapy. There was an initial spike in NK cell numbers across the patients post engraftment however this was not maintained, suggesting a diminished contribution level of transgenic progenitor cells to this compartment 59. 19 In 2006, the same London based group began conducting an ADA deficient SCID gene therapy trial. Six pediatric subjects were enrolled and administered HSCs transduced with the ADA cDNA after low dosages of pretransplant chemotherapy. Extended follow up of these patients demonstrated that four subjects achieved immune reconstitution between 6 and 24 months post transplantation. Three of the four patients in which gene therapy proved to be advantageous exhibited sufficient B-cell function to taper off immunoglobulin replacement therapy. In two subjects, gene therapy was ineffective: one subject received a very low dosage of HSCs while the other had a low percentage of transduced HSCs infused60. A major setback: T-ALL due to insertional mutagenesis Leukemia-like T lymphoproliferation occurred in 5 of the 20 subjects (1 in the London trial and 4 in the Paris trial) 61, 62 treated in the SCID-X1 trials between Paris and London due to insertional mutagenesis as a result of the retroviral vector integrating into proto-oncogene loci. Other genetic abnormalities were also found. After being treated with chemotherapy 4 of the 5 patients recovered fully and 1 died of refractory leukemia 61. It is more than likely that disease-associated factors influenced the outcome in these cases because similar gene transfer technology was used in the ADA deficient SCID trials and in some cases, similar LMO2 integration patterns (reviewed in 63) were observed, however none of these patients developed leukemia. A wide array of reasons has been proposed to explain this apparent discrepancy. A possible explanation is the difference in the specific transgenes, the c gene encodes a cytokine receptor chain, essential for cellular growth and proliferation versus the ADA gene, which is an essential housekeeping gene involved in purine salvage metabolism and does not induce cellular activation or proliferation. The rapid proliferation associated with progenitor rescue due to the introduction of the c gene is much more rapid than that associate with ADA rescue due in part to the fact that ADA expressing cells do not have the selective proliferation advantage seen 20 with cells expressing the c gene. This is because ADA has a compensatory effect, which benefits untransduced cells as well. In ADA deficient SCID, T-cell reconstitution takes approximately 18 months whereas SCID-X1 patients have full reconstitution within a few months of treatment. Rapid proliferation of T-cells may result in the accumulation of mutations in this population. Also since the c gene is required for T-cell development and proliferation, untransduced cells will not survive. ADA corrected cells have less of a proliferation advantage due to the fact that ADA expression affects all lymphocytes and provides cross correction to cell lacking the ADA transgene. Thymic damage also occurs during ADA deficiency, which is likely to play a compliant role in a more laconic immune recovery 64. HSCs from SCID-X1 patients may be intrinsically different than HSCs from ADA deficient patients; evidence exists to support the hypothesis that children with SCID-X1 are predisposed to cellular transformation 65. NK cells play an important role in tumor surveillance, in cases of human acute myeloid leukemia NK cells participate in clearance of leukemic cells 66 the absence of NK cells post immune recover in SCID-X1 patients may also serve as a contributing factor to the lack of tumor clearance observed in the setting of SCID. It has also been theorized that IL-2R may act cooperatively with LMO2 to induce oncogenesis 67, 68, however evidence to the contrary has also been presented 69, 70. The set back of having 25% of SCID-X1 patients treated with gene therapy develop leukemia between 3 and 6 years after treatment has inspired researchers and clinicians to proceed with cautioned enthusiasm while designing future gene therapy treatments. VI. Gene Therapy and Toxicity: The Evolution of Vectors Gene therapy has evolved over the past 20 years to treat several kinds of monogenic disorders. PIDs that can be treated with bone marrow transplantation pose as the most credible models for gene therapy because it has been established that an intact progenitor population can effectively treat these disorders. SCID is an especially 21 amiable model due to the fact that SCID patients cannot mount an immune response to the protein encoded by the transgene or immunogenic vector encoded epitopes as seen in other disorders treatable with gene therapy 71, 72. Retroviral vectors are produced through recombinant DNA techniques to act as gene delivery tools. Novel surface modifications and transgenes built using synthetic components can increase targeting specificity and efficiency 73. Vectors can integrate the transgene into chromosomal DNA of mammalian target cells with high efficiency, where it is passed on to successive generations of progeny during mitosis. Replication defective retroviral vectors have previously been based on murine oncoretroviruses (the -retrovirus), simian and human lentiviral viruses, retroviruses, and spumaviruses (also known as foamy viruses) (reviewed in , ). 16 73 The first-generation vectors that were used in these trials utilized a Maloney murine leukemia -retrovirus (MLV) backbone with viral long terminal repeats (LTRs) containing both an enhancer and promoter to drive transgene expression. In response to concerns of vector-mediated leukemogenesis, a variety of novel modifications have been made to new generation vectors to curb foreseeable risks associated with genomic integration. Self-inactivating vectors (SIN), which are able to delete the U3 enhancer and promoter in the LTR during the viral reverse transcription process, have a greatly reduced capacity to transactivate endogeneous genes after genomic integration. While the integration profile of SIN vectors is generally comparable to wild type retroviral vectors of the same type, SIN vectors demonstrate a significantly reduced level of genotoxicity 74. Additionally next generation vectors make use of promoters derived from cellular gene to drive transgene expression. Promoters from genes such as elongation factor-1 (EF1) create more physiologically typical gene transcription and reduce the strong enhancer activity associated with first generation vectors that utilize retroviral enhancer/promoters to transcribe transgenes 75. 22 Figure 5: First and second generation -retroviral vectors. First generation vectors were characterized by a region of long terminal repeats (LTR) situated at the 3’ and 5’ end of their genome. These LTRs have the capacity to promote expression of cellular oncogenes if the retroviral vector integrates in close proximity to them. Vector integration also has the capacity to silence tumor suppressor genes if it occurs within an exon of one of these genes. Second generation retroviral vectors or so called self inactivating (SIN) vectors are constructed such that following reverse transcription the viral promoter and enhancer elements including the CAAT and TATA box are deleted. Weaker promoters are also used such as human elongation factor-1 to reduce the potential for endogeneous gene transactivation. E/P, enhancer/promoter; LTR, long terminal repeats; Prom, promoter. 54 Retroviral Vector Insertional Mutagenesis in Gene Therapy The principle potential risk factor of retroviral vector mediated gene transfer is malignant transformation. Genotoxicity can result from several vector integration-associated mechanisms including: endogenous promoter activation, aberrant gene transcript truncation, and erroneous splicing. The most common cause of insertional mutagenesis is when retroviral vector insertion results in either the activation of proto-oncogenes or attenuation of tumor suppressor genes. Initially the risk factor for this was considered to be very low because it had never previously been observed in a clinical trial 76. 23 Review of the potential factors contributing to leukemogenesis suggests that insertional mutagenesis is the initiating causational event. However acquisition of secondary genetic abnormalities is essential for oncogenic transformation. Genetic analysis indicated that in 4 of the 5 patients that development clonal T-cell acute lymphoblastic leukemia (T-ALL), vector integration occurred in close proximity to the proto-oncogene LIM domain only 2 (LMO2) gene promoter and expression analysis indicated an increased level of LMO2 transcription 77, 61, 62. Integration near LMO2 caused increased transcriptional output of nearby genes and promoted clonal T-cell proliferation, however evidence of cooperative elements, such as additional genetic aberrancies, contributing to transformation were noted in the patients as well. Initially the two youngest patients (P4 and P5) were identified with uncontrolled exponential clonal out growth of mature T-cell that occurred approximately 3 years after gene therapy. The absence of replication competent retroviral vectors was confirmed by analysis of the specific leukemic-like T-cell clones. These clones did not have amphotropic envelope, reverse transcriptase, or integrase genes present. LMO2 insertions as well as other genetic aberrations were detected in both subjects. At the time of documented lymphoproliferative disease, peripheral T-cell clones exhibited a single insertion in both patients, where as prior to the onset of leukemia multiple integrations were observed in patients’ circulating T-cells. LMO2 transcript was normal as confirmed by exon specific reverse transcriptase PCR (RT-PCR) however its abundance of expression was comparable in levels to those found in mouse erythroleukemia (MEL) cell lines. Analysis of mRNA demonstrated colocalization of LMO2 and c indicating that the LMO2 allele targeted by retroviral insertion was being actively transcribed in both patients. These data confirmed retroviral cis-activation resulted in monoallelic LMO2 expression in both P4 and P5 77. P5 went into remission and recovered fully, however despite aggressive intervention P4 succumbed to refractory leukemia 61. A few years later an additional 3 patients who had developed leukemia were described 61, 62. One patient (P10) had, in addition to integration near the LMO2 24 promoter, an insertion site near the proto-oncogene BMI1. The patient (P7) lacking the LMO2 distal integration was found to have vector insertion near the promoter of CCND2, a gene known to act as a proto-oncogene in lymphoid cells. Upon analysis of patients’ blast cells, it became apparent that these cells were affected by chromosomal translocations, gain of function mutations activating NOTCH1 (P5 and P10), deletion of tumor suppressor gene CDKN2A (P4 and P7), 6q interstitial losses (P4 and P7), and SIL-TAL1 rearrangements (P5) 61. Both patients P10 and P7 recovered fully after chemotherapy. The last patient (P8) who entered into the SCID-X1 gene therapy trial at Great Ormond Street Hospital in London, England demonstrated that along with LMO2 transactivation, he also carried additional contributing genetic mutations. Other genetic abnormalities identified included chromosomal translocations, gain of function mutations activating NOTCH1 and reduced expression of tumor suppressor gene locus cyclin dependent kinase 2A (CDKN2A). The genes surrounding LMO2 were also found to be upregulated, suggesting the potent ability of the viral LTR enhancer to alter the expression of several nearby cellular genes. After administration of chemotherapy P8 recovered fully. Post chemotherapy the clone containing the LMO2 insertion was no longer detectable by linear amplification mediated (LAM) PCR or specific PCR tracking 62. Strong evidence exists that the disease environment created by SCID-X1 is supportive to transformation. Whether or not the expression of the γc chain transgene in thymocytes is a significant risk factor was previously a point of debate however evidence now exists to strongly suggest that the expression of the γc chain gene in and of itself is not permissive to oncogenesis. Instead, it is possible that there is an accumulation of cells poised to acquire genetic mutations prior to the rapid expansion of thymocytes. Once the development burden existing in SCID-X1 patients is lifted massive proliferation of these cells leads to oncogenic transformation. Another possibility is that IL-7 may be an important extrinsic factor in the support and proliferation of leukemic thymocytes, therefore overexpression of IL-7 could lead to a overriding of the normal cellular mechanism to shut down dysregulated growth 62. 25 The role of LMO2 in T-cell development. The transcription factor LMO2 contains zinc finger-like binding motifs called LIM domains and function as a bridging protein in multiprotein complexes that acts to upregulate genetic transcription 78. The LIM domain is essential for proteinprotein interaction, LMO2 cannot bind DNA directly but it has the capacity to arbitrate transcriptional activation and repression by binding to other transcription factors. While LMO2 is a T-ALL associated oncogene, it is also essential for normal hematopoiesis (reviewed in 79). LMO2 acts as a bridging molecule for GATA1, Ldb1, E2A, and TAL1 and this DNA-binding transcription regulator complex is essential for differentiation of all hematopoietic lineages 80. LMO2 is known to cause a subset of human T-cell acute lymphoblastic leukemias (T-ALL). T-ALL arises after an asymptomatic phase during which there is an accumulations of double negative thymocytes 78. Utilizing a transgenic mice model, McCormack and colleagues have demonstrated that the origin of LMO2-induced leukemia is thymocytes with T-cell differentiation capability that express several genes typical of multipotent hematopoietic progenitors. Their data supports the hypothesis that LMO2 acts to maintain or induce the self-renewal faculty of pre-leukemic progenitors and this continued long term renewal of thymocytes results in the accumulation of transforming mutations 81. During normal T-cell development in the thymus, LMO2 is down regulated during the early DN1-DN3 stages. If overexpression of LMO2 via retrovirus mediation is sustained it attenuates the differentiation of T-cells while leaving other lymphoid lineages unaffected 82. Patterns of Viral Integration Different retroviral backbones have differential patterns of integration and these insertion patterns are characterized by the epigenetic factors of the cell, nuclear translocation mechanisms, and the interaction of viral integrase with host proteins. The chromosomal integration of any vector backbone requires cellular DNA repair mechanisms. Insertion site selection is dependent upon both cellular 26 determinants and vector design, thereby giving each retroviral vector its own unique integration spectrum. The activation status and character of the target cell therefore plays a significant role in vector integration. Epigenetic profiles that favor integration have recently been identified 83. The LMO2 locus in hematopoietic progenitors has been shown to contain several features that accommodate frequent local integration. In vitro analysis of vector integration site selection has provided important information on the behavior of integrating retroviral vectors, however a homogeneous cell population cultured in isolation from biological complexities, such as selection pressure, is not predictive of an in vivo setting. In vivo, in the framework of gene therapy, transduced cell populations are subjected to post engraftment environments that influence survival, homing, and proliferation. Genome wide patterns of gene expression remained unchanged in transduced cells however analysis of the retroviral integration sites between transduced progenitors and post thymic T-cells indicate that sites of insertion influence cell survival, engraftment, and proliferation 84. -viral vectors have been shown to preferentially integrate into promoters, CpG islands, and DNase hypersensitivity sites 85. Data from the French SCID-X1, British SCID-X1, and Italian ADA-SCID trial demonstrated that when looking at transduced CD34+ progenitor cells derived from patients, over 65% of insertions are very near highly expressed genes, suggesting that vector integrations are correlated with the level of expression of genes in CD34+ target cells (reviewed in 86). This becomes problematic when these specific genes need to be downregulated during the later progressive development stages of T-cell differentiation. Genes that maintain a high expression level due to vector integration poses a high risk for insertional leukemogenesis. Lentiviral vector integration is a risk factor for the disruption of transcription units. This can occur via the introduction of aberrant cellular-vector chimeric transcripts 87, 88 or the induction of haploinsufficiency 89 because they favor integration into genes that are being actively transcribed 73. Haploinsufficency occurs when a diploid organisms who is heterozygous for a specific mutation is 27 clinically affected because only a single functional copy of the gene is incapable of providing sufficient gene product to assure normal function. SIN lentiviral vectors can also induce aberrant transcript formation since proviral integration can introduce a premature termination of transcription 87. It has also been described that SIN lentiviral vectors are susceptible, albeit at a much lower frequency than LTR containing lentiviral vectors, to transcriptional read through activity due to their tendency to integrate into genes 90. -viral vectors have the most neutral integration patterns and they can be designed such that they lack strong splice signals which could interfere with the processing of cellular mRNA 91. Foamy viruses have also been described as being less oncogenic than lenti- and retroviral vectors because they do not preferentially integrate into genes or genetic regulator units 92. Understanding preferred integration patterns of viral vectors and integration site analysis are a powerful tool for predictive analysis of potential genotoxicity. Vector integration may at some point in the future also be used as a research tool to understand epigenetic characteristics and gene expression profiles of tissues. Predicting Genotoxicity: Animal Models Despite already described issues with interspecies translation models, animal models pose as an invaluable tool for identifying risk factors and therapeutic outcomes in human disease. At this point, it is not yet possible to predict all potential severe adverse events that can occur as a result of vector integration, however animal models provide insight that would not otherwise be accessible. For example, it is known that pre-leukemic events arise in the thymus and sampling for clonality studies are based on peripheral blood, so in a preclinical setting, animal models are a salubrious solution for abstracting knowledge of leukemic development and predicting genotoxicity. Utilizing a tumor prone mouse model, Montini and colleagues were able to infer low genotoxicity from an array of vector integration sites. Cdkn2a-/- mice are highly susceptible to developing a broad range of tumor types in response to genetic lesions, researchers compared tumorigenesis as a result of lenti versus classical 28 retroviral integration. Retroviruses integration resulted in a dose dependant acceleration of tumor development based on LTR activity and insertion in oncogenes and cell cycle associated genes were enriched in early onset tumors. Transformation was unaffected by lentiviral vectors and no specific integration patterns were enriched for in tumors 93. High through put screening of insertional mutagenesis by replication competent retroviruses was utilized as a tool to identify potential oncogenes in mouse models of tumorigenesis and create a cancer gene database 94. These results are also useful for identifying integration sites that are common across different tumor types and for addressing, which genetic lesions contribute to transformation. To assess unique risk factors that the SCID environment imparts upon the subject, Shou et al development an SCID-X1 mouse model lacking both the Arf tumor suppressor gene and the c gene. In comparing Arf-deficient immunocompetent mice with Arf-deficient SCID-X1 mice, they found that the SCID background was required for the high rate of T-cell transformation associated with insertional mutagenesis. In vitro immortalization assays (IVIM) serve to drastically decrease the number of animals necessary for assessing genotoxicity. The IVIM assay relies on the induction of a proliferative, survival advantage conferred by insertional mutagenic activation of cellular oncogenes, which becomes clear during in vitro expansion when transduced cells are plated with cytokines that induce differentiation in a limiting dilution assay95. Mutants are also resistant to differentiating in response to a myeloid growth factor cocktail, therefore tremendous importance is placed upon growing conditions of the cells since slight variation could impact the sensitivity of the assay and potentially the types of mutants that can be isolated. Specifically the IVIM sensitively detects insertional regulation of Evi1 and Prdm16 via enhancer-related mechanisms in myeloid progenitors. Utilizing the IVIM assay, Modlich and colleagues have shown that relocation of the -retroviral enhancer promoter sequence from the LTR to an internal 29 position, thus creating the SIN vector, reduces the fitness of mutants. Mutations in transcription factor binding sites that reduce enhancer activity and the use of insulators also decreases transformation capacity. Certain cellular promoters when used in SIN vectors reduce the genotoxic risk of transformation below detection level 75. The IVIM assay has been used to demonstrate that the post-translational regulatory element of the woodchuck hepatitis virus (WPRE) does not affect insertional transformation, however it has been shown previously to improve vector generated transcription termination, thereby decreasing read through transcripts, and increase vector titration when placed up stream of the polyadenylation signal of the transgene 90. Lentiviral vector integration patterns demonstrate a substantially reduced risk of insertional mutagenesis when compared to -retroviral vectors in the IVIM assay. Zychlinksi and colleagues also demonstrated that specific cellular promoters reduce the risk of insertional mutagenesis when compared to viral promoters 75 and different insulator elements have significantly different functional capacity 96. Chromatin insulators are additional regulatory elements that can be utilized to decrease both vector silencing as a result of chromosomal position and genotoxicty. Upon utilizing the IVIM to test a battery of different insulators Baum and colleagues found that only a subset were potent enough to reduce the transforming potential of strong enhancer crosstalk capacity to any significant degree. VII. Future treatment Stem cell-based therapy is a quickly evolving field of medicine that makes use of our growing understanding of genetics to cure previously untreatable disease. Progress in viral vector designs provides an appreciable advancement in the therapeutic treatment of monogenic diseases. Integrating gene delivery systems allow for stable and sustained gene expression, however continued efforts are being made to increase precision and decrease risks associated with genomic insertion. SIN vectors offer distinct safety advantages compared with their wild type counterparts (Figure 30 7). Research has shown that they substantially less likely to interact with neighboring cellular genes 97, read through transcripts are significantly reduced 90, and multi-lineage lymphoid reconstitution, as seen in murine models of SCID-X1 and phase I clinical trials of Wiskott-Aldrich Syndrome (WAS) and adrenoleukodystrophy (ALD) (reviewed in 98), is similar to those achieved with LTR driven transgene expression 99. They nevertheless require the addition of promoters and enhancers within the body of the vector to attain high levels of vector expression and these elements potentially possess the capacity to alter the expression of adjacent cellular genes. Tissue specific regulatory elements have been shown to reduce this risk 75. Chromatin insulators are naturally occurring DNA regulatory units block the interaction between vectors and the surrounding host genome by forming boundaries between adjacent chromatin domains and can be used to mitigate vector silences and insertional mutagenesis due to vector mediated gene activation (Figure 7). The addition of suicide genes to vectors could be utilized to subvert vector activation in the event of a serious adverse reaction such as abnormal clonal outgrowth or malignant transformation. This technique has been under investigation in fields of cancer therapy and regenerative medicine. It has been proven effective in cases of graft versus host disease post adoptive cell therapy. Transgenic herpes simplex thymidine kinase (HSV-TK) expression in donor cells has been effectively utilized as a safety switch in patients receiving cellular therapy. Significant drawbacks of this system exist as the mechanism of interference requires alterations in DNA synthesis so cell suicide can take several days and is not 100% effective in eliciting cell death 100. HSV-TK is also potentially immunogenic as it is virally derived. The antiviral drug ganciclovir is necessary for suicide gene activation, which makes this class of antiviral drugs no longer available for therapeutic use in these patients. In an investigation of the effectiveness of a different suicide gene to abrogate adverse events associated with cell transfer therapies; Di Stasi and colleagues utilized an inducible T-cell safety switch based on the fusion of human caspase-9 to a modified human forkhead binding protein. A synthetic dimerization drug could be 31 administered in the event of graft versus host symptoms, which could activate the caspase-9 fusion protein leading to rapid apoptosis of cells expressing the construct 101. Previous studies indicated that the use of T-cells depleted of alloreactive progenitor cells provide immune protection against viral disease during recovery from HSCT 102, this technique also spares leukemia reactive cells 103. The addition of inducible caspase-9 to donor T-cells allows for rapid destruction of these cells in the event of graft versus host disease. The additional of a suicide gene, such as inducible caspase-9, to the vectors used in gene therapy would allow for the destruction of transduced cells in the event of monoclonal outgrowth or transformation. HSV-TK would not be an ideal choice as a suicide gene due to the factor that the class of antiviral drug used to activate the suicide gene is an important therapeutic agent used in immunocompromised individuals due to their extreme susceptibility to viral infection and the prevalence of herpes simplex and herpes varicella. Antibodies could also be used to eradicate transduced cells. In a mouse model of SCID-X1, Scheumann and colleagues transduced murine HSCs with a c myc-tag chimeric transgene. The transcription of this gene resulted in a myc tagged c fusion protein that could be targeted with myc antibodies and depleted in the presence of complement activity 104. This strategy could be potentially used in SCID however it could not be effectively used as a safety strategy in other disorders treated with gene therapy due to the immunogenicity of the myc tagged protein. Addition of the myc tag could also alter the intended functional activity of the c chain subunit. Genomic editing The ability to apply site-specific genomic manipulation provides a platform for genetic research and therapeutic intervention. Homologous recombination is the process by which cells are able to resolve stalled DNA replication forks, repair double stranded DNA breaks, and foster genetic recombination 105. Gene targeting is accomplished by utilizing an exogenous template DNA molecule that is introduced into a cell to replace a corresponding chromosomal segment via homologous 32 recombination, this process represents a directed and specific way of altering the genome. Two recently developed designer nucleases are Transcription ActivatorLike Effector Nucleases (TALENS) and Zinc finger nucleases (ZFN). TALENS are synthetic restriction enzymes made up of a transcription activator-like effector DNA binding domain fused to a DNA cleavage domain that can be engineered to targeted to any specific site within the genome for genetic editing. Figure 6: Gene editing utilizing designer endonucleases. ZFN made up of a zinc finger DNA recognition domain and a FokI endonuclease domain joined by a short linker bind the genomic DNA target site, which initiates the dimerization of the nuclease domain. Dimerization induces the enzyme to become catalytically active and it cleaves the genomic DNA, generating a double stranded DNA break. The double stranded DNA break can be repair via NHEJ pathway resulting in gene disruption, or homology directed repair. Homology directed repair can either lead to gene correction of transgene cassette insertion. Homology directed repair is homology driven because the two sister chromatids are in close proximity to each other. If the donor template contains homology to the DNA sequences on either side of the break, the exogeneous sequence can be incorporated at the site allowing for transgene insertion or mutation correction 98. Both TALENS and ZFN mediate site-specific gene addition by introducing double stranded DNA breaks, which results in gene integration due to homologydirected repair (HDR) utilizing the supplied DNA fragment as a template. In the 33 absence of a supplied DNA template ZFN induced double stranded DNA breaks stimulate the endogenous error prone NHEJ repair pathway, which results in gene disruption. DNA specific ZFN and template DNA for gene correction can be incorporated into separate integrase-deficient lentiviral vectors and targeted to affected cells. Transiently expressed ZFN made up of a zinc finger DNA recognition domain and a FokI endonuclease domain joined by a short linker bind the genomic DNA target site, which initiates the dimerization of the nuclease domain. Dimerization induces the enzyme to become catalytically active and it cleaves the genomic DNA, generating a double stranded DNA break (Figure 6). Cellular mechanisms then induce the activation of exonucleases, which cuts the 5’ end from the broken ends, leaving single stranded 3’ sticky ends. The donor DNA template complex can then anneal to their homologous sequences within the genomic DNA and act as a template for DNA synthesis upon recruitment of DNA polymerase. The site of the double stranded DNA break is thereby repaired via DNA synthesis utilizing the donor DNA as a template resulting in the correction of the disease causing mutation. ZFN provide genetic correction in function as well as controlled expression. Due to direct genomic DNA editing the corrected gene is under the control of endogenous regulatory elements. This type of correction has the added benefited of leaving the rest of the genome unperturbed. However, co-delivery of the template DNA and the ZFN represents a major hurdle to exploiting the use of ZFN mediated genetic manipulation. Also genomic instability as a potential result of ZFN gene targeting needs to be more fully understood. There is a low efficiency of correction associated with ZFN gene targeting however, in instances of correcting genes like the c chain, the resolution of the mutation will give these cells a strong selective growth advantage, such that a low percentage of corrected cells will be permissive to immune recovery, at least in theory. Control of vector site integration can also be achieved with the integrase binding cellular protein lens epithelium derived growth factor (LEDGF). The Cterminal portion of LEDGF interacts with lentiviral integrase. Tethering of viral 34 integrase results in directed integration and in the presence of LEDGF viral integration into active genes is reduced. Introduction of chimeras composed of LEDGF integrase-binding domains fused to alternate chromatin binding domains that program integration outside of transcription units can be used to obviate random gene insertion 106 35 Figure 7: Future implements for improved safety and efficacy of HSC-based gene therapy. The implementation of SIN vectors in gene therapy has been a substantial step towards improving the safety of vectors used in for transgene incorporation. It is also necessary to ensure that the corrective gene is expressed at physiologically relevant levels and can persist in the progeny of transduced cells. Physiological regulation of transgene expression via cellular promoters as well as the addition of chromatin insulators has lead to a decreased likelihood of genomic perturbation by promoter transactivation or by positional silencing. Selection of gene integration sites could potentially lead to better transgene transfer and reduced risk by obviating random genomic insertion. Targeting of such sites with designer endonucleases can lead to site directed genetic correction via induced homologous recombination (also refered to as homology directed repair). Non-chemotherapy based clearing using agents such as monoclonal antibodies can ablate bone marrow and lead to improved engraftment. 107 36 VIII. Discussion Exceptional advances have been made in the therapeutic treatment of mongenic disorders (Figure 7). Improvements in vector safety and efficiency have provided momentum for increasing the accessibility of gene therapy for a variety of disease types including immunological and lysosomal storage related disorders, as well as neurodegenerative diseases and cancer. Currently HSCT is a curative therapy for SCID and other immunological primary immunodeficiencies. Despite this, its inaccessibility to many patients and its several life threatening complications render it a suboptimal intervention, therefore alterative treatment options are necessary. Symptom-alleviating enzyme replacement therapy is available for certain monogenic diseases such as metabolic disorders and various lysosomal storage disorders, however the cost of sustaining patients over the course of their lifetime is astronomically high and in some situation impossible. Gene therapy serves as a wide platform for the curative venture of an extensive array of diseases that were previously considered insurmountable. SCID is an ideal disorder for modeling gene therapy due to the fact that HSCT is curative for individuals afflicted with SCID, and these patients do not have the immune capacity to reject transduced HSCs. However a number of obstacles and safety concerns exist with gene therapy, such as insertional mutagenesis and vector immunogenicity in disorders other than SCID. Insertional mutagensis is of particular concern with SCID because the genetic landscape of this disorder is particularly permissive to oncogenic transformation. SCID patients are predisposed to various cancers due to a variety of factors. The absence of NK cells as seen in approximately 70% of SCID cases 108 results in insufficient tumor surveillance. SCID is also often observed in the backdrop of other genetic abnormalities, so when transformation occurs there is not a cellular system or tumor suppressor-signaling pathway in place to subvert oncogenesis. Murine models of SCID demonstrate an increased population of bone marrow lymphoid progenitors, which may be posed for transformation once the differentiation block is lifted. 37 Understanding viral vector integration patterns in a variety of cell types is essential for optimal vector backbone selection. As HIV infection has not culminated in oncogenic transformation it is reasonable to hypothesize that lentiviral vectors might be safer alternatives to oncogenic retroviral vectors. Lentiviral vectors have not been associated with insertional mutagenesis in pre-clinical research or clinical trials, however an instance of monoclonal outgrowth has been observed in one patient from a -thalassemia trial (reviewed in 109). SIN -viruses and foamy viruses have also recently been shown to have a non-oncogenic pattern of integration, as they do not preferentially target transcriptional regulatory sites. While targeted vector integration is a progressive and promising mode of overcoming insertional mutagenesis, additional research must be done to benefit from the full potential of technologies such as designer endonucleases. Targeted integration requires that vectors accurately home to a specific genomic site that is permissive to robust transgene expression, not susceptible to insertional mutagenesis, epigenetically not conducive to vector silencing, and resistant to transcriptional disruption of the surrounding genome. Issues associated with off target sites of genomic instability may also arise due to the fact that nucleases create double stranded DNA breaks. These double stranded DNA breaks result in the activation of intrinsic DNA repair mechanisms, however nonspecific DNA cleavage could result in the unintended disruption of genes. Integration tethering protein lens epithelium–derived growth factor (LEDGF) could act as a potential alternative for integration targeting, as it has previously been associated with reduced integration into genes. The cellular transcriptional coactivator LEDGF/p75 is a cellular factor harnessed by HIV for chromosomal integration. The HIV viral integrase tethers to the chromatin via the LEDGF/p75, which thereby increases the efficiency of targeted integration into transcriptional units 110. The engineering of LEDGF integrase binding domains fused to specific chromatin binding domains could act to direct viral integration into specific predetermined sites. 38 An additional potential resource of precise genomic editing is the RNAguided nuclease technology known as clustered regularly interspaced short palindromic repeats (CRISPR)/Cas system. The CRISPR/Cas is a part of the type II prokaryotic adaptive immune system, which aids in RNA-guided site-specific DNA cleavage. Cong and colleagues recently demonstrated that in mammalian cells, the Cas9 nucleases can induce highly precise cuts at endogenous genomic loci via the guidance of short RNAs. Several different guide sequences can be loaded into a single CRISPR array, which allows for simultaneous editing of several genomic sites 111 . Utilizing RNA to direct specific genomic editing poses as a powerful tool for biotechnology and genomic manipulation. Induced pluripotent stem (IPS) cells represent an interesting potential future prospect for gene therapy. While several safety concerns could potentially arise due to the insertional mutagenesis and the proto-oncogenes used for cellular reprogramming, IPS cells pose as a great source for disease modeling. IPS cells are created with viral vectors and have induced expression of factors associated with pluripotency, this represent a potential hazard due to the fact that these genes are well established oncogenes. These cells can be derived from patient tissue, reprogrammed into pluripotent progenitors, and then differentiation into hematopoietic precursors to be used for the modeling of individual patients. Disease modeling in this context could be used to test viable therapies in the future. IPS cells have already been generated from individuals with Parkinson's disease, amyotrophic lateral sclerosis (ALS), and β-thalassaemia to further investigate mechanisms of these diseases. Genetic engineering is in the early stages of investigating potential mechanisms of immune resistance to pathologies such as cancer and HIV. T-cell engineering could lead to novel immune functions as oppose to simply correcting specific defects. HIV leads to the progressive destruction of CD4+ T-cells, as these levels decline, patients progress towards AIDS. If it were possible to create a population of T-cells resistance to HIV mediated CD4+ T-cell destruction, patients would be protected against immune decline. Genomic editing is one method that could be used to modify the T-cell genome. The use of retroviruses to express anti39 HIV genes that inhibit steps in the viral infection or replication cycle or the introduction of small interfering RNA molecules could be used to prevent infection of cells 112. ZFN could also be used to modify the viral genome directly and knock out essential genes required for viral replication. Genetic modification of T-cells could provide treatment against specific tumor types. Genetically engineered T-cells have shown impressive efficacy and clinical benefit in human anti-cancer therapy trials 113. Modified antigen receptors could be highly effective in directing T-cells to mount a strong immune response again a number of different tumor types. Recent research has suggested that the tumor microenvironment plays a central role in oncogenic immune evasion 114. Tcells programmed to be unsusceptible to this inactivation could ensure effective tumor eradication. An important consideration however would be to ensure that these T-cells do not create an autoimmune event due to their inability to be shut down by normal immunosuppressive mechanisms. Genetically engineered, epitope specific programmed T-cells could be a potent tool for overcoming specific immune evasion events associated not only with cancer but with other pathologies as well. In conclusion, with its continuous evolution, and the furthered understanding of potential adverse effects associated with gene therapy, this field offers great hope for the eradication of a wide variety of previously debilitating diseases. 40 IX. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. References Tonegawa, S. Somatic generation of antibody diversity. Nature 302, 575– 581 (1983). Ferrari, S. et al. Mutations of CD40 gene cause an autosomal recessive form of immunodeficiency with hyper IgM. Proceedings of the National Academy of Sciences of the United States of America 98, 12614–12619 (2001). Conley, M. E., Mathias, D., Treadaway, J., Minegishi, Y. & Rohrer, J. Mutations in btk in patients with presumed X-linked agammaglobulinemia. Am. J. Hum. Genet. 62, 1034–1043 (1998). Mohamed, A. J. et al. Bruton's tyrosine kinase (Btk): function, regulation, and transformation with special emphasis on the PH domain. Immunol. Rev. 228, 58–73 (2009). Conley, M. E. Defects in early B-cell development: comparing the consequencesof abnormalities in pre-BCR signaling in the humanand the mouse. Immunol. Rev. 1–16 (2000). Cancro, M. P. et al. xid mice reveal the interplay of homeostasis and Bruton's tyrosine kinase-mediated selection at multiple stages of B cell development. International immunology 13, 1501–1514 (2001). Peschon, J. J. et al. Early lymphocyte expansion is severely impaired in interleukin 7 receptor-deficient mice. J. Exp. Med. 180, 1955–1960 (1994). Freeden-Jeffry, von, U. et al. Lymphopenia in interleukin (IL)-7 gene-deleted mice identifies IL-7 as a nonredundant cytokine. J. Exp. Med. 181, 1519– 1526 (1995). Cunningham-Rundles, C. The many faces of common variable immunodeficiency. Hematology Am Soc Hematol Educ Program 2012, 301– 305 (2012). Baldovino, S. et al. Common variable immunodeficiency: Crossroads between infections, inflammation and autoimmunity. Autoimmunity Reviews 1–6 (2012). doi:10.1016/j.autrev.2012.11.003 Maul, R. W. et al. Uracil residues dependent on the deaminase AID in immunoglobulin gene variable and switch regions. Nature Publishing Group 12, 70–76 (2010). Petersen-Mahrt, S. K., Harris, R. S. & Neuberger, M. S. AID mutates E. coli suggesting a DNA deamination mechanism for antibody diversification. Nature 418, 99–103 (2002). Perez-Duran, P. et al. UNG shapes the specificity of AID-induced somatic hypermutation. Journal of Experimental Medicine 209, 1379–1389 (2012). Imai, K. et al. Human uracil–DNA glycosylase deficiency associated with profoundly impaired immunoglobulin class-switch recombination. Nat Immunol 4, 1023–1028 (2003). Ta, V.-T. et al. AID mutant analyses indicate requirement for class-switchspecific cofactors. Nat Immunol 4, 843–848 (2003). Fischer, A. Human primary immunodeficiency diseases: a perspective. Nat Immunol 5, 23–30 (2003). 41 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. Buckley, R. H. et al. Human severe combined immunodeficiency: genetic, phenotypic, and functional diversity in one hundred eight infants. J. Pediatr. 130, 378–387 (1997). Leonard, W. J. Cytokines and immunodeficiency diseases. Nat Rev Immunol 1, 200–208 (2001). Weerkamp, F., Pike-Overzet, K. & Staal, F. J. T. T-sing progenitors to commit. Trends in Immunology 27, 125–131 (2006). Takahama, Y. Journey through the thymus: stromal guides for T-cell development and selection. Nat Rev Immunol 6, 127–135 (2006). Dik, W. A. New insights on human T cell development by quantitative T cell receptor gene rearrangement studies and gene expression profiling. Journal of Experimental Medicine 201, 1715–1723 (2005). Rothenberg, E. V., Moore, J. E. & Yui, M. A. Launching the T-cell-lineage developmental programme. Nat Rev Immunol 8, 9–21 (2008). Notarangelo, L. D. Functional T Cell Immunodeficiencies (with T Cells Present). Annu. Rev. Immunol. 31, 130108114109008 (2012). HRSA. EVIDENCE REVIEW: Severe Combined Immunodeficiency (SCID). 1– 80 (2009). Noguchi, M. et al. Interleukin-2 receptor gamma chain mutation results in Xlinked severe combined immunodeficiency in humans. Cell 73, 147–157 (1993). Buckley, R. H. M olecularD efects inH umanS evereC ombinedI mmunodeficiency andA pproaches toI mmuneR econstitution. Annu. Rev. Immunol. 22, 625–655 (2004). Kovanen, P. E. & Leonard, W. J. Cytokines and immunodeficiency diseases: critical roles of the γc‐dependent cytokines interleukins 2, 4, 7, 9, 15, and 21, and their signaling pathways. Immunol. Rev. 202, 67–83 (2004). Puel, A., Ziegler, S. F., Buckley, R. H. & Leonard, W. J. Defective IL7R expression in T(-)B(+)NK(+) severe combined immunodeficiency. Nat Genet 20, 394–397 (1998). Lodolce, J. P. et al. IL-15 Receptor Maintains Lymphoid Homeostasisby Supporting Lymphocyte Homing and Proliferation. Immunity 1–8 (1998). Kennedy, M. K. et al. Reversible defects in natural killer and memory CD8 T cell lineages in interleukin 15-deficient mice. J. Exp. Med. 191, 771–780 (2000). Macchi, P. et al. Mutations of Jak-3 gene in patients with autosomal severe combined immune deficiency (SCID). Nature 377, 65–68 (1995). Notarangelo, L. D. et al. Mutations in severe combined immune deficiency (SCID) due to JAK3 deficiency. Hum. Mutat. 18, 255–263 (2001). Fischer, A. et al. Severe combined immunodeficiency. A model disease for molecular immunology and therapy. Immunol. Rev. 203, 98–109 (2005). Cavazzana-Calvo, M., André-Schmutz, I. & Fischer, A. Haematopoietic stem cell transplantation for SCID patients: where do we stand? Br J Haematol 160, 146–152 (2012). Aiuti, A. et al. Gene therapy for immunodeficiency due to adenosine deaminase deficiency. N. Engl. J. Med. 360, 447–458 (2009). 42 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. Valerio, D., Duyvesteyn, M. G. C., Ormondt, H. V., Khan, P. M. & van der Eb, A. J. Adenosine deaminase (ADA) deficiency in cells derived from humans with severe combined immunodetficiency is due to an aberration of the ADA protein. Nucleic Acids Research 12, 1015–1024 (1984). Giblett, E. R., Anderson, J. E. & Cohen, F. Pillars article: Adenosine-deaminase deficiency in two patients with severely impaired cellular immunity. The Lancet. 1972. 300: 1067-1069. … (Baltimore (2012). Schwarz, K., Ma, Y., Pannicke, U. & Lieber, M. R. Human severe combined immune deficiency and DNA repair. Bioessays 25, 1061–1070 (2003). Ma, Y. et al. The DNA-dependent protein kinase catalytic subunit phosphorylation sites in human Artemis. J. Biol. Chem. 280, 33839–33846 (2005). O'Driscoll, M. et al. DNA ligase IV mutations identified in patients exhibiting developmental delay and immunodeficiency. Molecular Cell 8, 1175–1185 (2001). Enders, A. et al. A severe form of human combined immunodeficiency due to mutations in DNA ligase IV. J. Immunol. 176, 5060–5068 (2006). van der Burg, M. A new type of radiosensitive T-B-NK+ severe combined immunodeficiency caused by a LIG4 mutation. J. Clin. Invest. 116, 137–145 (2005). Arnaiz-Villena, A. et al. Brief report: primary immunodeficiency caused by mutations in the gene encoding the CD3-gamma subunit of the Tlymphocyte receptor. N. Engl. J. Med. 327, 529–533 (1992). Dadi, H. K., Simon, A. J. & Roifman, C. M. Effect of CD3delta deficiency on maturation of alpha/beta and gamma/delta T-cell lineages in severe combined immunodeficiency. N. Engl. J. Med. 349, 1821–1828 (2003). Cossu, F. Genetics of SCID. Italian Journal of Pediatrics 36, 76 (2010). Wada, T. Oligoclonal expansion of T lymphocytes with multiple second-site mutations leads to Omenn syndrome in a patient with RAG1-deficient severe combined immunodeficiency. Blood 106, 2099–2101 (2005). Aleman, K., Noordzij, J. G., de Groot, R., van Dongen, J. J. & Hartwig, N. G. Reviewing Omenn syndrome. European journal of pediatrics 160, 718–725 (2001). Buckley, R. H. et al. Hematopoietic stem-cell transplantation for the treatment of severe combined immunodeficiency. N. Engl. J. Med. 340, 508– 516 (1999). Candotti, F. et al. Gene therapy for adenosine deaminase-deficient severe combined immune deficiency: clinical comparison of retroviral vectors and treatment plans. Blood 120, 3635–3646 (2012). Vicente, R., Adjali, O., Jacquet, C., Zimmermann, V. S. & Taylor, N. Intrathymic transplantation of bone marrow-derived progenitors provides long-term thymopoiesis. Blood 115, 1913–1920 (2010). Chan, B. et al. Long-term efficacy of enzyme replacement therapy for Adenosine deaminase (ADA)-deficient Severe Combined Immunodeficiency (SCID). Clinical Immunology 117, 133–143 (2005). WIGINTON, D. A., ADRIAN, G. S., FRIEDMANt, R. L., SUTTLE, D. P. & HUTTON, 43 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. A. J. J. Cloning of cDNA sequences of human adenosine deaminase. Proceedings of the National Academy of Sciences of the United States of America 80, 7481–7485 (1983). Blaese, R. M. et al. T lymphocyte-directed gene therapy for ADA- SCID: initial trial results after 4 years. Science 270, 475–480 (1995). Shaw, K. L. & Kohn, D. B. A tale of two SCIDs. Science Translational Medicine 3, 97ps36 (2011). Aiuti, A. et al. Immune reconstitution in ADA-SCID after PBL gene therapy and discontinuation of enzyme replacement. Nat Med 8, 423–425 (2002). Onodera, M. et al. Successful Peripheral T-Lymphocyte−Directed Gene Transfer for a PatientWith Severe Combined Immune Deficiency Caused by Adenosine Deaminase Deficiency. 1–8 (1997). Aiuti, A. Correction of ADA-SCID by Stem Cell Gene Therapy Combined with Nonmyeloablative Conditioning. Science 296, 2410–2413 (2002). Stephan, V. et al. Atypical X-linked severe combined immunodeficiency due to possible spontaneous reversion of the genetic defect in T cells. N. Engl. J. Med. 335, 1563–1567 (1996). Gaspar, H. B. et al. Long-Term Persistence of a Polyclonal T Cell Repertoire After Gene Therapy for X-Linked Severe Combined Immunodeficiency. Science Translational Medicine 3, 97ra79–97ra79 (2011). Gaspar, H. B. et al. Hematopoietic Stem Cell Gene Therapy for Adenosine Deaminase-Deficient Severe Combined Immunodeficiency Leads to LongTerm Immunological Recovery and Metabolic Correction. Science Translational Medicine 3, 97ra80–97ra80 (2011). Hacein-Bey-Abina, S. et al. Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J. Clin. Invest. 118, 3132–3142 (2008). Howe, S. J. et al. Insertional mutagenesis combined with acquired somatic mutations causes leukemogenesis following gene therapy of SCID-X1 patients. J. Clin. Invest. 118, 3143–3150 (2008). Qasim, W., Gaspar, H. B. & Thrasher, A. J. Progress and prospects: gene therapy for inherited immunodeficiencies. Gene Ther. 16, 1285–1291 (2009). Thompson, L. F. et al. Metabolites from apoptotic thymocytes inhibit thymopoiesis in adenosine deaminase-deficient fetal thymic organ cultures. J. Clin. Invest. 106, 1149–1157 (2000). Shou, Y., Ma, Z., Lu, T. & Sorrentino, B. P. Unique risk factors for insertional mutagenesis in a mouse model of XSCID gene therapy. Proceedings of the National Academy of Sciences of the United States of America 103, 11730– 11735 (2006). Fauriat, C. et al. Deficient expression of NCR in NK cells from acute myeloid leukemia: evolution during leukemia treatment and impact of leukemia cells in NCRdull phenotype induction. Blood 109, 323–330 (2007). Woods, N.-B., Bottero, V., Schmidt, M., Kalle, von, C. & Verma, I. M. Gene therapy: Therapeutic gene causing lymphoma. Nat Cell Biol 440, 1123–1123 (2006). 44 68. 69. 70. 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. Davé, U. P., Jenkins, N. A. & Copeland, N. G. Gene Therapy Insertional Mutagenesis Insights. Science 303, 333 (2004). Pike-Overzet, K. et al. Gene therapy: Is IL2RG oncogenic in T-cell development? Nature 443, E5–E5 (2006). Thrasher, A. J. et al. Gene therapy: X-SCID transgene leukaemogenicity. Nature 443, E5–6– discussion E6–7 (2006). Lamers, C. H. J. et al. Immune responses to transgene and retroviral vector in patients treated with ex vivo-engineered T cells. Blood 117, 72–82 (2011). Kondo, E. et al. Retroviral vector backbone immunogenicity: identification of cytotoxic T-cell epitopes in retroviral vector-packaging sequences. Gene Ther. 12, 252–258 (2004). Suerth, J. D., Schambach, A. & Baum, C. Genetic modification of lymphocytes by retrovirus-based vectors. Current Opinion in Immunology 24, 598–608 (2012). Moiani, A. et al. Deletion of the LTR Enhancer/Promoter Has No Impact on the Integration Profile of MLV Vectors in Human Hematopoietic Progenitors. PLoS ONE 8, e55721 (2013). Zychlinski, D. et al. Physiological Promoters Reduce the Genotoxic Risk of Integrating Gene Vectors. Mol Ther 16, 718–725 (2008). Hacein-Bey-Abina, S. et al. A serious adverse event after successful gene therapy for X-linked severe combined immunodeficiency. N. Engl. J. Med. 348, 255–256 (2003). Hacein-Bey-Abina, S. LMO2-Associated Clonal T Cell Proliferation in Two Patients after Gene Therapy for SCID-X1. Science 302, 415–419 (2003). Grutz, G. G. et al. The oncogenic T cell LIM-protein Lmo2 forms part of a DNA-binding complex specifically in immatureT cells. EMBO J. 17, 4594– 4605 (1998). NAM, C. & RABBITTS, T. The Role of LMO2 in Development and in T Cell Leukemia After Chromosomal Translocation or Retroviral Insertion. Mol Ther 13, 15–25 (2006). Omari, El, K. et al. Structure of the leukemia oncogene LMO2: implications for the assembly of a hematopoietic transcription factor complex. Blood 117, 2146–2156 (2011). McCormack, M. P. et al. The Lmo2 Oncogene Initiates Leukemia in Mice by Inducing Thymocyte Self-Renewal. Science 327, 879–883 (2010). Pike-Overzet, K. et al. Ectopic retroviral expression of LMO2, but not IL2Rγ, blocks human T-cell development from CD34+ cells: implications for leukemogenesis in gene therapy. Leukemia (2007). doi:10.1038/sj.leu.2404563 Santoni, F. A., Hartley, O. & Luban, J. Deciphering the Code for Retroviral Integration Target Site Selection. PLoS Comput Biol 6, e1001008 (2010). Schwarzwaelder, K. et al. Gammaretrovirus-mediated correction of SCID-X1 is associated with skewed vector integration site distribution in vivo. J. Clin. Invest. 117, 2241–2249 (2007). Biasco, L. et al. Integration profile of retroviral vector in gene therapy treated patients is cell-specific according to gene expression and chromatin 45 86. 87. 88. 89. 90. 91. 92. 93. 94. 95. 96. 97. 98. 99. 100. 101. 102. conformation of target cell. EMBO Mol Med 3, 89–101 (2011). Pike-Overzet, K., van der Burg, M., Wagemaker, G., van Dongen, J. J. & Staal, F. J. New Insights and Unresolved Issues Regarding Insertional Mutagenesis in X-linked SCID Gene Therapy. Mol Ther 15, 1910–1916 (2007). Cesana, D. et al. Whole transcriptome characterization of aberrant splicing events induced by lentiviral vector integrations. J. Clin. Invest. 122, 1667– 1676 (2012). Moiani, A. et al. Lentiviral vector integration in the human genome induces alternative splicing and generates aberrant transcripts. J. Clin. Invest. 122, 1653–1666 (2012). Heckl, D. et al. Lentiviral Vector Induced Insertional Haploinsufficiency of Ebf1 Causes Murine Leukemia. Mol Ther 20, 1187–1195 (2009). Higashimoto, T. et al. The woodchuck hepatitis virus post-transcriptional regulatory element reduces readthrough transcription from retroviral vectors. Gene Ther. 14, 1298–1304 (2007). Suerth, J. D. et al. Alpharetroviral Self-inactivating Vectors: Long-term Transgene Expression in Murine Hematopoietic Cells and Low Genotoxicity. Mol Ther 20, 1022–1032 (2012). Deyle, D. R., Khan, I. F., Ren, G. & Russell, D. W. Lack of genotoxicity due to foamy virus vector integration in human iPSCs. Gene Ther. 1–6 (2013). doi:10.1038/gt.2013.6 Montini, E. et al. Hematopoietic stem cell gene transfer in a tumor-prone mouse model uncovers low genotoxicity of lentiviral vector integration. Nat. Biotechnol. 24, 687–696 (2006). Akagi, K. RTCGD: retroviral tagged cancer gene database. Nucleic Acids Research 32, 523D–527 (2004). Modlich, U. et al. Cell-culture assays reveal the importance of retroviral vector design for insertional genotoxicity. Blood 108, 2545–2553 (2006). Gaussin, A. et al. CTF/NF1 transcription factors act as potent genetic insulators for integrating gene transfer vectors. Gene Ther. 19, 15–24 (2011). Zhou, S. et al. A self-inactivating lentiviral vector for SCID-X1 gene therapy that does not activate LMO2 expression in human T cells. Blood 116, 900– 908 (2010). Naldini, L. Ex vivo gene transfer and correction for cell-based therapies. Nature Publishing Group 12, 301–315 (2011). Thornhill, S. I. et al. Self-inactivating Gammaretroviral Vectors for Gene Therapy of X-linked Severe Combined Immunodeficiency. Mol Ther 16, 590– 598 (2008). Ciceri, F. et al. Infusion of suicide-gene-engineered donor lymphocytes after family haploidentical haemopoietic stem-cell transplantation for leukaemia (the TK007 trial): a non-randomised phase I–II study. Lancet Oncology 10, 489–500 (2009). Di Stasi, A. et al. Inducible apoptosis as a safety switch for adoptive cell therapy. N. Engl. J. Med. 365, 1673–1683 (2011). Amrolia, P. J. Adoptive immunotherapy with allodepleted donor T-cells 46 103. 104. 105. 106. 107. 108. 109. 110. 111. 112. 113. 114. improves immune reconstitution after haploidentical stem cell transplantation. Blood 108, 1797–1808 (2006). Amrolia, P. J. Selective depletion of donor alloreactive T cells without loss of antiviral or antileukemic responses. Blood 102, 2292–2299 (2003). Scheumann, N., Kieback, E. & Uckert, W. Safety Modality for X-linked Severe Combined Immunodeficiency Gene Therapy. J Cell Sci Ther 03, (2012). Lombardo, A. et al. Gene editing in human stem cells using zinc finger nucleases and integrase-defective lentiviral vector delivery. Nat. Biotechnol. 25, 1298–1306 (2007). Brady, T. & Bushman, F. D. Nondividing Cells: A Safer Bet for Integrating Vectors? Mol Ther 19, 640–641 (2009). Kohn, D. B. & Candotti, F. Gene therapy fulfilling its promise. N. Engl. J. Med. 360, 518–521 (2009). Mikkers, H., Pike-Overzet, K. & Staal, F. J. T. Induced pluripotent stem cells and severe combined immunodeficiency: merely disease modeling or potentially a novel cure? Pediatr Res 71, 427–432 (2012). Persons, D. A. Hematopoietic stem cell gene transfer for the treatment of hemoglobin disorders. Hematology Am Soc Hematol Educ Program 690–697 (2009). doi:10.1182/asheducation-2009.1.690 Llano, M. et al. An Essential Role for LEDGF/p75 in HIV Integration. Science 314, 461–464 (2006). Cong, L. et al. Multiplex Genome Engineering Using CRISPR/Cas Systems. Science 339, 819–823 (2013). Burnett, J. C., Zaia, J. A. & Rossi, J. J. Creating genetic resistance to HIV. Current Opinion in Immunology 24, 625–632 (2012). Porteus, M. H. & Fischer, A. Engineering the immune system to cure genetic diseases, HIV, and cancer. Current Opinion in Immunology 24, 576–579 (2012). Raaijmakers, M. H. G. P. Niche contributions to oncogenesis: emerging concepts and implications for the hematopoietic system. Haematologica 96, 1041–1048 (2011). 47