Case study
advertisement

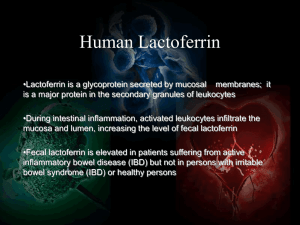
Maria Chavez Case Number 11-Inflammatory Bowel Disease: Crohn’s Please answer the following questions from your lab text on Mr. Sims: 1. What is inflammation bowel disease? What does current medical literature indicate regarding its etiology? Inflammatory bowel disease (IBD) involves chronic inflammation of all or part of the digestive tract. IBD primarily includes ulcerative colitis and Crohn's disease. Both usually involve severe diarrhea, pain, fatigue, and weight loss. The etiology/causes of IBD are unknown. One possible cause is an immune system malfunction 2. Mr. Sims was initially diagnosed with ulcerative colitis and then diagnosed with Crohn’s. how could this happen? What are the similarities and differences between Crohn’s disease and ulceration colitis? The only way to be diagnosed with ulcerative colitis and then diagnosed with Crohn’s is by being misdiagnose in the first place. Ulcerative colitis is an inflammatory bowel disease that causes long-lasting inflammation and ulcers in the innermost lining of your large intestine and rectum. The ulcerative colitis inflammation is continuous compared to Crohn’s that may have segments of healthy and inflamed portions. Crohn's disease, inflammation often spreads deep into affected tissues. The inflammation can involve different areas of the digestive tract (the large intestine, small intestine or both.) Also all the layers of the mucosa are affected. Both ulcerative colitis and Crohn’s have the same symptoms; diarrhea, pain, fatigue, and weight lost. 9. is Mr. Sims a likely candidate for short bowel syndrome? Define short bowel syndrome, and provide a rationale for your answer. Since the patient has gone a bowel resection, the main cause of short bowel syndrome is bowel resection. Therefore, the patient could be a candidate for short bowel syndrome. however, the amount of bowel removed does not qualify him to have short bowel syndrome. Short bowel syndrome is a condition in which nutrients are not properly absorbed (malabsorption) because a large part of the small intestine is missing or has been surgically removed. When medications are no longer effective at controlling the inflammation and managing the symptoms of Crohn’s disease, or when complications develop, treatment sometimes includes the removal of affected sections in which nutrients could be not properly absorbed. Therefore the patient could be a candidate for short bowel syndrome. 10. What type of adaptation can the small intestine make after resection? For some people, short bowel syndrome is a temporary problem. Even after extensive surgery, the remaining small intestine is sometimes able to adjust to the short bowel length by working harder than before. Although intestinal adaptation may begin soon after the onset of short bowel syndrome, it may take as long as two years before the small intestine has fully adjusted. True intestinal adaptation is achieved when a person can successfully digest and absorb all necessary nutrients through the GI tract. 14. Mr. Sims underwent resection of 200 cm of jejunum and proximal ileum with placement of jejunostomy. The ileocecal valve was preserved. Mr.Sims did not have an ileostomy, and his entire colon remains intact. How long is the small intestine, and how significant is this resection? Since the small intestine is about 6 meters (600cm), the patient now has about 400cm left. Overall, the patient lost about 1/3 of this small intestine. This resection is significant, but it doesn’t qualify him to have short bowel syndrome since an individual needs to lose about ½ of the bowel to be qualified. 19. Identify any significant and/or abnormal laboratory measurements from both his hematology and his chemical labs. For hematology: Hemoglobin (12.9 g/dL) and Hematocrit (38%) are low compared to normal values respectively (14-17g/dL and 40-54%). This is due since the patient has an ulceration which he is losing blood. For chemistry Protein is lab values (5.5 g/dL) are lower than normal values (6-8g/dL). Protein is low in this patient due to malnutrition and inflammation. Albumin (3.2 g/dL) and prealbumin (11mg/dL) are also lower than the normal levels (3.5-5g/dL and 16-35mg/dL). These values are low due to the inflammation that the patient is currently at C-reactive protein is another inflammation marker. C-reactive protein value (2.8mg/dL) is higher than normal value (<1.0 mg/dL) HDL the patient levels of HDL (38mg/dL) could be lower than normal (120-199mg/dL) since the patient has lost significant amount of weight and has affected the fat storage include his cholesterol. What are Mr. Sims Estimated needs for energy, protein and fluid? Energy= used Harris Benedict formula with activity factor of 1.2 and injury factor of 1.3; 1,568.82 kcals/day Protein=1.2-1.5 grams of PRO/kg; 76.32-95.4 Fluid= 35ml/kg/day; 2,226ml/day 23. What is refeeding syndrome? Is Mr. Sims at risk for this syndrome? How can it be prevented? %Usual wt =Current weight/usuall weight X100= 83.33%. Based on his usual weight percentage, the patient is in mild degree of malnutrition. Although, the degree of malnutrition is not severe, the patient can still be at risk for refeeding syndrome. The patient is at risk since the patient hasn’t being able to eat in a while, is in tube feeding and his laboratory results indicate malnutrition and vitamin deficiencies. In addition, the patient needs to have a special diet due to his recent surgery stating with clear liquids and progressed into small frequent meals if adequate. To prevent this syndrome, the individual needs to start with small frequent meals and small amounts of food and drink. 24. I agree with the team’s decision to initiate parenteral nutrition since it is unknown how long will the patient will need PN. The PN will meet his estimated needs and more. Compared the estimated needs versus the PN, the patient is receiving more kcals and more fluid. Also, the patient is meeting the estimated amount of protein through the parenteral nutrition. For treatment: 85ml/hr X24 hrs=2040ml total Protein: 2040ml /X=1000,ml/42.5 grams 86.7 grams of protein for the day CHO: 2040/X=1000ml/200grams 408 grams of CHO (dextrose) for the day Fat: 2040ml/X=1000ml/30g 61.2 grams of fat for the day Total Kcals: 2,343.6 kcals are provided by the PN 86.7 that by 4 to protein344.4 kcals 408 that by 3.4 for CHO1,387.2 kcals 61.2 that by 10grams612 kcals 26. Please see article on Blackboard in course documents. What does this information tell you about Mr. Sims? There is a table on pg 124 The oxygen consumption and the CO2 production tells me the patient’s energy expenditure by measuring O2 and CO2. Based upon the information provided by the table and the equation on the article, the patient estimated needs are 2,091.3 Kcals/day. The RQ (respiratory quotient) tells me the ratio between C02 and O2. The RQ can help determine the net substrate utilization and can also serve as a quality control indicator. Also the RQ value can suggest the presence of technical errors in measurement. However, the patient’s value is within good values (0.67-1.2). RMR (resting metabolic rate) tells me how many calories the patient is burning without doing anything but rest. 30. Evaluate the following 24 hour urine data: 24 hr urinary nitrogen for 12/20: 18.4 grams. By using the daily input/output record for 12/20 that records the amount of PN received, calculate Mr. Sims’ nitrogen balance on postoperative day 4. How would you interpret this information? Should you be concerned? Are there problems with the accuracy of nitrogen balance studies? Explain. 86.7 grams protein divided by 6.25 grams N2=13.8 grams N2 13.8grams-18.4 grams+3.4 grams N2 insensibl losses= - 7.36 grams so, negative nitrogen balance This means that the intake of nitrogen into the body is greater than the loss of nitrogen from the body, so there is an increase in the total body pool of protein. A negative value can be associated with several causes including serious injuries and during periods of fasting/starvation. Excess nitrogen can be toxic to the body, however, I don’t think we should be concern with that since the goal is to improve the patient’s health by improving his diet and having extra nitrogen won’t hurt him. Since the patient is malnourish, the patient will utilize protein more efficiently than those who are normally replete and hence give an overestimate of normal nitrogen retention/balance. There are many problems with the accuracy of nitrogen balance since every detail needs to be precise in order to have accuracy including recording protein intake appropriately and measure urination just to name a few. 31. Client Education Material on Blackboard in course documents. On post-op day 10, Mr.Sims’ team notes he has had bowel sounds for the previous 48 hours and had his first bowel movement. The nutrition support team recommends consideration of an oral diet. What should MR. Sims be allowed to try first? What would you monitor for tolerance? If successful, when can the parenteral nutrition be weaned? The patient will be allowed to try first clear foods such apple juice, Gatorade, and gelatin since they will get absorbed in the stomach but will make the small intestine start working. I will monitor for physical signs such as the patient not having discomfort such as diarrhea, vomiting, bloating and cramping. Also I will continue monitoring bowel movement and glucose. In addition, monitor weight to determine if patient still losing weight or gaining weight. 32. What would be the primary concerns as MR. Sims prepared for rehabilitation after his discharge? Be sure to address his need for supplementation of any vitamins and minerals. Identify two nutritional outcomes with specific measures for evaluation. First nutritional outcome and concern is to progress to full texture food and eat the amount of kcals needed to have an adequate nutrition (approximately 2091.3 kcals based upon IC) Second nutritional outcome is to normalize lab values such as hemoglobin and hematocrit, In addition, the patient will need to take a multivitamin, iron, and folate supplementation.