File - Brittany Check
advertisement
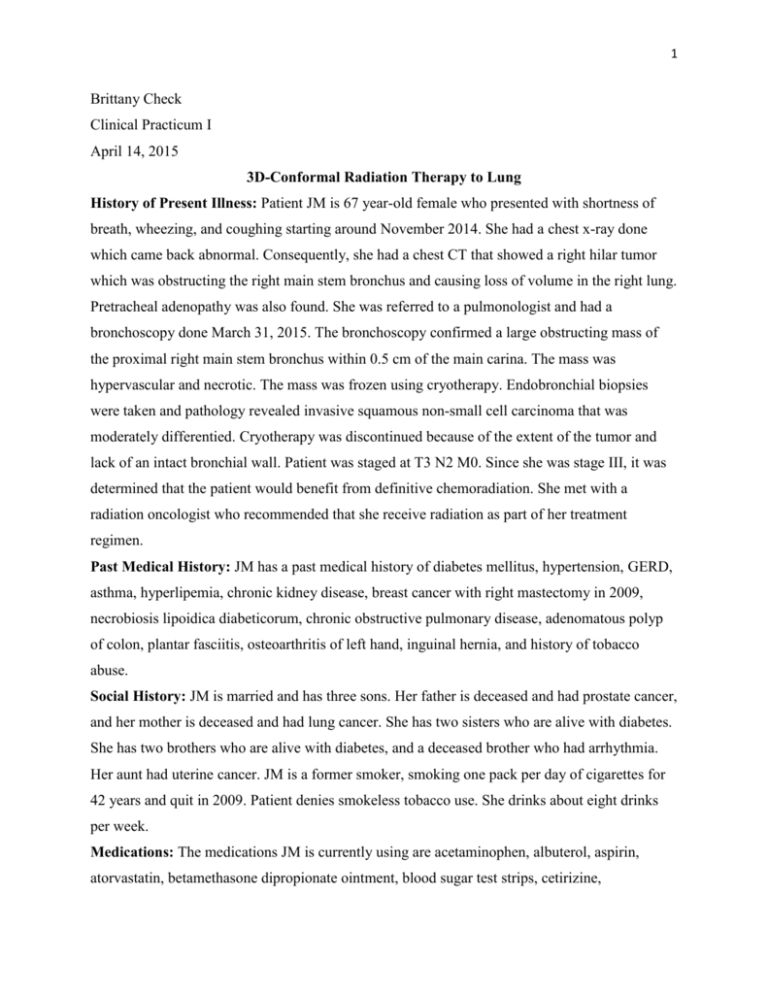
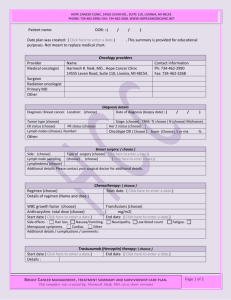
1 Brittany Check Clinical Practicum I April 14, 2015 3D-Conformal Radiation Therapy to Lung History of Present Illness: Patient JM is 67 year-old female who presented with shortness of breath, wheezing, and coughing starting around November 2014. She had a chest x-ray done which came back abnormal. Consequently, she had a chest CT that showed a right hilar tumor which was obstructing the right main stem bronchus and causing loss of volume in the right lung. Pretracheal adenopathy was also found. She was referred to a pulmonologist and had a bronchoscopy done March 31, 2015. The bronchoscopy confirmed a large obstructing mass of the proximal right main stem bronchus within 0.5 cm of the main carina. The mass was hypervascular and necrotic. The mass was frozen using cryotherapy. Endobronchial biopsies were taken and pathology revealed invasive squamous non-small cell carcinoma that was moderately differentied. Cryotherapy was discontinued because of the extent of the tumor and lack of an intact bronchial wall. Patient was staged at T3 N2 M0. Since she was stage III, it was determined that the patient would benefit from definitive chemoradiation. She met with a radiation oncologist who recommended that she receive radiation as part of her treatment regimen. Past Medical History: JM has a past medical history of diabetes mellitus, hypertension, GERD, asthma, hyperlipemia, chronic kidney disease, breast cancer with right mastectomy in 2009, necrobiosis lipoidica diabeticorum, chronic obstructive pulmonary disease, adenomatous polyp of colon, plantar fasciitis, osteoarthritis of left hand, inguinal hernia, and history of tobacco abuse. Social History: JM is married and has three sons. Her father is deceased and had prostate cancer, and her mother is deceased and had lung cancer. She has two sisters who are alive with diabetes. She has two brothers who are alive with diabetes, and a deceased brother who had arrhythmia. Her aunt had uterine cancer. JM is a former smoker, smoking one pack per day of cigarettes for 42 years and quit in 2009. Patient denies smokeless tobacco use. She drinks about eight drinks per week. Medications: The medications JM is currently using are acetaminophen, albuterol, aspirin, atorvastatin, betamethasone dipropionate ointment, blood sugar test strips, cetirizine, 2 cholecalciferol, esomeprazole, fluticasone-salmeteral, guaiFENesin, hydrochlorothiazide, Lisinopril, metformin, metoprolol-XL, multivitamin tablet, and raloxifene. Diagnostic Imaging: JM had a chest x-ray which was abnormal. She had a bronchoscopy which showed a large obstructing mass of the proximal right main stem bronchus within 0.5 cm of the main carina that was hypervascular and necrotic. On March 25, 2015 she had a chest CT that revealed an ill-defined 4 cm right hilar mass. Volume loss in the right lung was seen along with mucus plugging multiple segmental bronchi. Reticular and nodular opacity was noted in the right lung which was thought to be related to atelectasis and small airway obstruction. On March 27, 2015 she had a PET scan that demonstrated a large mass in the right hilum positive for uptake along with an enlarged precarinal lymph node with uptake. A nodule negative for uptake in the right upper lobe was believed to be benign. Radiation Oncologist Recommendations: JM was recommended definitive chemoradiation for her stage III disease. She signed an informed consent form after discussing external beam radiation therapy with the radiation oncologist. He discussed a 6.5 week regimen of therapy. Acute effects were discussed which included fatigue, dysphagia, odynophagia, cough, chest pain, shortness of breath, skin erythema, dermatitis, and desquamation. Late effects were also discussed such as secondary malignancies, lung scarring, heart scarring, esophageal scarring, and spinal cord damage. Patient decided to move forward with radiation therapy. Prior to her treatment, the radiation oncologist recommended a brain MRI. If metastases were found in the brain, radiation would have been palliative. Since the MRI was negative, the patient underwent curative radiation therapy treatments. The Plan (prescription): The radiation oncologist prescribed 6600 cGy in 33 fractions to a lung planning target volume (PTV). Her treatment was designed using 3D conformal technique. If constraints to organs at risk could not be met with 3D conformal technique, the radiation oncologist noted that he would have used an intensity modulated radiation therapy (IMRT) plan. She was treated once each day, five days each week. The radiation oncologist prescribed 6 MV photons beams to be used. He also indicated that a heterogeneous dose calculation was to be used. Patient Setup/Immobilization: JM underwent a 4D CT simulation on April 3, 2015. For the CT simulation, the patient was positioned supine with her arms over her head in a vac-loc within a wingboard (Figure 1). She was straightened prior to the scan. A reference isocenter was placed 3 by marking the patient with radiopaque markers. Prior to each treatment, the patient was positioned with a pair of orthogonal kV image using ExacTrac to register to bony anatomy to ensure proper alignment of the target. If the treatment lasted more than 15 minutes or the patient appeared to have moved, intrafraction tracking was done with ExacTrac to verify alignment. The patient received gated treatment. A box with reflective dots on the patient’s abdomen was tracked by a camera and treatment only occurred during the 30% to 70% phases of the patient’s breathing cycle. Anatomical Contouring: The 4D CT scan was transferred to MIM for fusion with the PET scan. From this fusion, the gross tumor volume (GTV), clinical treatment volume (CTV), PTV, and involved lymph node areas were delineated by the radiation oncologist. Organs at risk were also contoured including the left lung, right lung, heart, spinal cord, and esophagus. Beam Isocenter/Arrangement: JM was treated on a Varian Clinac 21EX linear accelerator with 6 MV photons. The dosimetrist placed isocenter centrally within the PTV. Gantry angles of 210˚, 300˚, 0˚, 35˚, 140˚, and 180˚ were utilized (Figure 2). Weighting was adjusted to be cover the PTV. The field arrangement was selected by the dosimetrist to adequately cover the PTV while limiting dose to critical structures when possible. For example, beams were placed sparingly on the patient’s left side to avoid treating through the contralateral lung as much as possible. The dosimetrist initially planned with five fields to avoid entering through the patient’s right breast expander, but the dose distribution was better with the use of this sixth beam. The therapists testified that the expander was not mobile and would not contribute to substantial inconsistencies in the patient’s body contour. Treatment Planning: The treatment plan was developed using the Varian Eclipse treatment planning system. The Acuros XB algorithm was utilized because of its better accuracy in heterogeneous tissue.1,2 A goal list was set by the radiation oncologist to minimize unnecessary dose to organs at risk while adequately covering disease (Figure 3). During the planning process, the radiation oncologist initially directed the dosimetrist to create an IMRT plan. After the planning process was started and dose constraints were easily met, the physician requested that the dosimetrist try a 3D conformal plan. Upon evaluation, he discussed the better conformity of the prescription isodose line to the PTV using the IMRT plan. However, adequate sparing of organs at risk were achieved by the 3D conformal plan, therefore using IMRT was not necessary. To create a homogeneous dose distribution in the 3D conformal plan, segmentation was utilized 4 for the 210˚ and 140˚ fields (Figures 4-6). On the 300˚, 0˚, and 35˚ fields, 20˚ electronic dynamic wedges were used with the heels superiorly on the patient to increase the dose on the inferior aspect of the treatment volume. All beams were 6 MV photons to best cover the tumor which was located within low-density lung tissue.3 All critical structures were spared to an acceptable degree (Figure 7). Overall, the dosimetrist was able to achieve a V20 of about 30% and a V5 of about 48% for the total lung structure. Quality Assurance/Physics Check: Secondary monitor unit checks were done using MU Check software to verify appropriate monitor units for each field. For the segmented fields, segment verification was performed by a physicist using DoseLab. Conclusion: Overall, this was an interesting case because of the decision whether or not to use IMRT. Although for most patients, including this patient, IMRT can create a more conformal and homogeneous plan, it is not always necessary. In order to justify the cost of IMRT, there should be a substantial benefit for the patient over a 3D conformal plan. In this patient’s case, the physician believed that the 3D conformal plan was sufficient in meeting critical structure constraints. In the future, it would be interesting to compare a DVH for a 3D conformal and IMRT plan for several patients to evaluate the differences, or examine further to see how the patient outcome was effected. 5 References 1. Kroon PS, Hol S, Essers M. Dosimetric Accuracy and clinical quality of Acuros XB and AAA dose calculation algorithm for stereotactic and conventional lung volumetric modulated arc therapy plans. Radiat Oncol. 2013;8(1):1-8. http://dx.doi.org/10.1186/1748-717X-8-149 2. Rana S, Roger K, Pokharel S, Cheng C. Evaluation of Acuros XB algorithm based on RTOG 0813 dosimetric criteria for SBRT lung treatment with RapidArc. J Appl Clinc Medic Phys. 2014;15(1):118-129. http://dx.doi.org/10.1120/jacmp.v15i1.4474 3. Wang L, Yorke E, Desobry G, Chui CS. Dosimetric advantage of using 6 MV over 15 MV photons in conformal therapy of lung cancer: Monte Carlo studies in patient geometries. J Appl Clin Med Phys. 2002;3(1):51-59. http://dx.doi.org/10.1120/jacmp.v3i1.2592. 6 Figures Figure 1. Patient position and immobilization for simulation and treatment. Figure 2. Isocenter and beam arrangement shown in axial view. 7 Figure 3. Dosimetry goal list assigned by radiation oncologist. Figure 4. Isodose lines shown in axial view. 8 Figure 5. Isodose lines shown in sagittal view. Figure 6. Isodose lines shown in coronal view. 9 Figure 7. Dose volume histogram for final plan.