Bret Conrad March Case Study Adenocarcinoma of the Rectum
advertisement

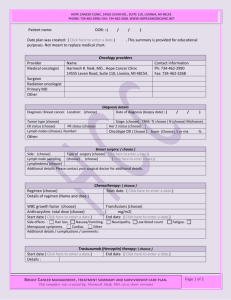
1 Bret Conrad March Case Study Adenocarcinoma of the Rectum Case Study History of Present Illness: LR is a 65 year old female seen for consultation for infiltrating moderately differentiated adenocarcinoma of the distal rectum. She presented to her primary care physician for a routine physical and was found to have a mass in her rectum. She had noticed some streaking on toilet paper but thought it was due to hemorrhoids. She denied any abdominal pain, hematochezia, or changes in bowel habits. She had not had any weight changes or decreased energy. She had a colonoscopy 10 years ago and was due for another when the mass was found. She then had a colonoscopy on 1/17/2013 which revealed a mass just above the dentate line approximately 3 centimeters (cm) in size. The biopsy samples were reviewed at Loyola Medical Center and were consistent with infiltrating moderately differentiated adenocarcinoma. Endoscopic Ultrasound (EUS) was performed on 1/25/2013 which revealed a non-circumferential mass in the posterior rectal wall invading through the muscularis propria. Two malignant appearing peritumoral nodes were seen on the EUS. A Computed Tomography (CT) of the chest, abdomen, and pelvis was performed on 1/18/2013 and showed rectal wall thickening but no other suggestions of malignancies. The patient presented for oncologic evaluation regarding radiation therapy for her Stage 3B cancer. Past Medical History: LR has had an appendectomy, knee surgery, and tubal ligation. Social History: The patient is married with 2 children. She is a non-smoker and drinks alcohol socially. She is retired and worked as a secretary. Medications: The medications the patient takes includes Alprazolam, Xeloda, Prochlorperazine, Sertraline, and multi-vitamins. Diagnostic Imaging: LR underwent a colonoscopy with biopsy on 1/17/2013 which revealed the rectal mass. She also underwent a CT of the chest, abdomen, and pelvis that showed rectal wall thickening for no evidence of malignancy. Radiation Oncologist Recommendations: The patient’s case was addressed as part of multidisciplinary clinic where management options were discussed. The radiation oncologist recommended neoadjuvant concurrent chemoradiation therapy to the rectum to improve local control and increase survival. The rationale for radiation therapy was discussed with the patient 2 along with its potential risks, benefits, short and long term side effects, and complications. Risks discussed included bleeding, pain, stricture formation, fatigue, diarrhea, and skin irritation. The Plan (Prescription): The prescription was to give LR preoperative radiation with concurrent Xeloda. The first Planning Target Volume (PTV) was treated to 4500 centigray (cGy) and included the rectal tumor and at risk lymph nodes. A boost was given to the second PTV of 540 cGy that included the rectal tumor and the mesorectum. A daily dose of 180 cGy was given with a total dose of 5040 cGy to the tumor. Patient Setup/ Immobilization: The patient underwent a CT simulation on the Philips CT scanner. She was positioned prone on the table. Prone positioning was used so that the lateral ports can adequately cover the posterior portion of the sacrum.1 She was lying on a belly board so that the bowel can fall out of the treatment field. An Alpha Cradle was used to mold around her legs to keep her legs from moving during the treatments (Figure 1). A blue Duncan mask was used to support her head while lying in the prone position. A blue sponge was put under her ankles for comfort and a three point set-up was used. Anatomical Contouring: The critical structures that were contoured in this case include the right and left femoral heads, bladder, bowel, and the rectum. After all of the structures were contoured the radiation oncologist contoured a Gross Tumor Volume (GTV), PTV which will receive 4500 cGy, and a PTV that will receive a boost up to 5040 cGy. Beam Isocenter / Arrangement: For the CT simulation, a 3 point set-up was used. The lasers in the CT room were used to put crosshairs on the patient’s pelvis and BBs were put on these marks so they could be observed on the scan (Figure 2). During treatment planning, the reference points for both the initial treatment and the boost were put at the isocenter. The same isocenter was used for both plans to make is easier for the radiation therapists. For this case, a standard 3 field beam arrangement was used. Both the initial plan and the boost used a Posterior-Anterior (PA) beam, right lateral, and left lateral. There was no couch or collimator rotations needed for this case. The plan created actually used multiple energies for both of the plans. The PA beam used a 10 Megavoltage (MV) beam and the laterals used 15 MV beams, for both the initial plan and the boost. This was done since the PTV was so posterior that a 15 MV beam on the PA field was penetrating too deep. The dose distributions were much better using a 10 MV beam on the PA field. The field size for the initial plan was 15.3 cm by 16.3 cm for the PA and 15.1 cm by 17.7 3 cm for the laterals. The field size for the boost plan was 12.4 cm by 7.8 cm for the PA field and 9.7 cm by 8.4 cm for the lateral fields. This plan was treated on the Varian True Beam machine. Treatment Planning: After the radiation oncologist contoured the GTV and PTVs then the treatment planning process begun. The planning was done in the Eclipse planning system. The algorithm that was used was the Anisotrophic Analytical Algorithm (AAA). As stated earlier, a 3 field technique was used for this case. Usually a 3 field technique is used to allow a homogenous dose to the tumor bed while sparing the anterior structures.2 If an AP field was added then the small bowel and bladder would receive much more dose. The standard gantry angles were used for both plans with the PA being at 0 degrees, right lateral at 90 degrees, and the left lateral at 270 degrees. Everything is opposite because the patient is in the prone position. A Multi-Leaf Collimator (MLC) was used to conform the treatment fields to avoid treating normal structures while including the entire PTV. Wedges were also used for both the initial plan and the boost plan. All of the lateral fields had a 45 degree wedge placed in the path of the beam. The heels of the wedge were on the side of the PA field so it would pull the dose more anterior and lower the hotspot. Since there is no AP beam, the wedges help pull the dose anteriorly. On the initial plan the beams were also weighted. The PA field was given 52 % of the dose while the laterals only gave 24 % each. This was done so the hot spot was more posterior and away from the bowel (Figures 3 and 4). The boost plan used equal weighting since it was a smaller field with no bowel involvement (Figures 5 and 6). The hot spot for the initial plan was 109.1 % and the hot spot for the boost plan was 103.1 %. The Dose Volume Histogram (DVH) for the entire plan showed the normal structures were kept under tolerance (Figure 7). Quality Assurance/ Physics Check: The plan was reviewed by the dosimetrist by checking the prescription page and also putting the information into Rad Calc 6.0 computer program. The Rad Calc program showed that both the initial plan and boost plan were 0.3 % different than the monitor units I calculated. This is a very low differential which is very good. The radiation oncologist then checked the prescription and signed off on the final plan. Then the physicist checked the entire plan and signed off on every field in the treatment. Finally, before the first treatment the radiation therapists took films of every field and double checked the monitor units. Conclusion: I had to be very careful with this case when labeling the treatment fields. Since the patient was prone, all of the fields are opposite. I had to double check a couple times that all my fields and images were labeled correctly. I also adjusted the weighting a lot on the initial plan 4 before I was happy with the outcome. I was finally told it is good to have the hot spot be as close to the GTV as possible, instead of in a normal structure. The weighting was also an important factor in keeping my normal structures at a low enough dose. The PTV for the initial plan was very large as seen by the large field sizes. This was also the first plan that I used more than 1 energy on a plan. The plan was just not looking good with all 10 MV or all 15 MV beams, so I was told to use both energies. This was a good learning case for me, and I will be better prepared for the next prone patient I plan. 5 Figures Figure 1: Patient Set-up in the CT Simulation Figure 2: Patient Crosshair used for Shifting 6 Figure 3: Transverse View of Isodose Lines in Initial Plan Figure 4: Sagittal View of Isodose Lines in Initial Plan 7 Figure 5: Transverse View of Isodose Lines in Boost Plan Figure 6: Sagittal View of Isodose Lines in Boost Plan 8 Figure 7: DVH for Both Plans Combined 9 References 1. Vann AM, Dasher BG, Chestnut SK, Wiggers NH. Portal Design in Radiation Therapy. 2nd ed. Columbia, SC: The R.L. Bryan Company; 2006. 2. Washington CM, Leaver D. Principles and Practices of Radiation Therapy.2nd ed. Philadelphia, PA: Mosby; 2004.