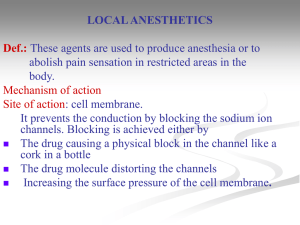
Local Anesthetics
Dr. Nadia Haress
Local Anesthetics
Local anesthetics are drugs that when given topically or parenterally to a localized area, produce a state of local anesthesia by reversibly blocking the
nerve conduction that transmit the feeling of pain from this area to the brain.
As their action is reversible, so after their use, it is followed by complete recovery in nerve functions with no risk of structural damage to nerve fiberes of the cells.
History:
Cocaine: First natural local anesthetic which was isolated from Coca leaves but it has disadvantages of euphoria and addiction.
Procaine: First synthetic local anesthetic (LA) but it has slow onset,
short duration of action and causes allergy.
Lidocaine: First modern LA. It is the most widely used LA today but it causes vasodilatation at the site of application ⇒ duration of action, increases ↑ heart rate and palpitation. So, it is taken with epinephrine ⇒
vasoconstriction ⇒ absorption and ↑ duration of action.
Mepivacaine and Prilocaine: They vasodilatation effect so, used without epinephrine for hypertensive patients.
1
Mechanism of Action: They prevent the conduction and formation of
action potential by either fully or partially blocking the sodium Na + ion channels ⇒ no significant change in the membrane potential ⇒ conduction of action potential along the neuron would be prevented.
N.B.: Action potential = the ability of nerve cells to be excited.
Characteristics for an Ideal LA :
1.
It should produce reversible block of sensory nerve fibres with minimal effect on the motor fibres.
2.
It should have rapid onset with sufficient duration of action without systemic toxicities.
3.
It should be non-irritating to tissues.
4.
It should be effective upon injection or local action.
2
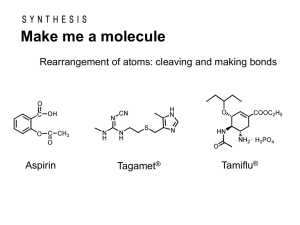
Structure-Activity Relationships (SAR):
According to Lofgren’s classification, the LA has 3-parts:
A) Liphophilic Portion (Aryl Group):
The lipophilic portion of the molecule is essential for L.A. activity because it is responsible for penetration into the cell membrane.
1- Electron-donating group on ortho or para positions ⇒ ↑ anesthetic activity. e.g.:
p-Amino group (NH
2
) in procaine and butacaine.
p-Butylamino group in tetracaine.
p-Propanoxy group in proparacaine.
2- Electron-withdrawing group (-NO
2
, -CO, -CN) ⇒ anesthetic activity.
3
3- o,o-Dimethyl substitution ⇒ protection against amide or ester hydrolysis.
4- Insertion of a methylene group (CH
2
) between the aromatic moiety and the carbonyl function ⇒ LA activity and ↑ anticholinergic activity due to prohibiting the formation of zwitter ion (in procaine).
B) Intermediate Chain:
The intermediate chain is responsible for the onset of action.
↑ pKa ⇒ LA activity (pKa must be 7.5-9).
1Short carbon chain(- 3C) in length: ↑ length ⇒ ↑ pKa ⇒ LA activity.
2Presence of small alkyl groups around the ester or amido ⇒ hydrolysis by esterase or amidase ⇒ ↑ duration of action (as in etidocaine).
3Thioester ⇒ dermatitis but more active than normal esters.
4Amino-amide LA ⇒ hydrolysis ⇒ ↑ duration of action. Also, they facilitate the formation of zwitter ion ⇒ ↑ anesthetic activity.
5Generally, L.A. with ↑ lipid solubility and pKa values ⇒ ↑ onset and toxicity.
4
C) Hydrophilic Portion:
The hydrophilic portion is responsible for water solubility and binding to the receptor.
1The tertiary alkylamine function is needed as :
It forms water-soluble salts ⇒ pharmaceutical formulation.
Onium ions produced by protonation of the 3ary amine group ⇒ ↑ binding to the receptors.
2The hydrophilic group can be in the form of a secondary amine or part of a heterocycle but 2ary amines are more irritating to the tissues and 1ary amines ⇒ LA activity.
Binding of Ester-Type LA to Receptor Sites (Prototype)
1.
Van der Waals’ forces.
2.
Electrostatic attraction (ionic bond).
3.
Dipole-dipole attraction.
5
Classification of LAs:
1.
Amino Esters.
2.
Amino Amides (Lidocaine Derivatives).
3.
Miscellaneous.
1. Amino Esters LAs
Disadvantages:
Short duration due to rapid hydrolysis by esterases.
Allergenicity due to its metabolism (hydrolysis by cholinesterase)into p-aminobenzoic acid (PABA) which causes allergy.
Cocaine
The parent (natural) drug.
It is the alkaloid isolated from coca leaves.
6
Procaine (Novocain)
2-(N,N-Diethylamino)ethyl-4-aminobenzoate
It is the first synthetic LA (prototype).
It has tissue penetration ⇒ LA activity.
Chloroprocaine
2-(N,N-Diethylamino)ethyl-4-amino-2-chlorobenzoate
The presence of Cl ortho to the carbonyl of the ester function ↑ its rate of hydrolysis by cholinesterase 3 times more than procaine and benzocaine (very short duration of action).
7
Benzocaine
It has LA activity.
Ethyl p-aminobenzoate
Tetracaine
2-(Diethylaminoethyl)-4-(butylamino)benzoate.
It has an ↑ LA activity.
Benoxinate
2-(Diethylaminoethyl)-4-amino-3-(butyloxy)benzoate
8
Butacaine
Hexylcaine
1-(Cyclohexylamino)-2-propanol benzoate
9
General Synthesis of Ester Derivatives:
H
2
N COOH
C
4
H
9
X
C
4
H
9
COOH
HO
N(CH
3
)
2
O
2
N CH
3
Ox.
O
2
N COOH
EtOH
H
+
O
2
N
Tetracaine
COOEt
HO
N
Red.
Benzocaine
Red.
Procaine
O
2
N
2- Amino Amides LAs
Lidocaine (Xylocaine, Lignocaine)
COO
N
2-(Diethylamino)-N-(2,6-dimethylphenyl)acetamide
It is very lipid soluble ⇒ ↑ onset and ↑ duration of action than procaine and tetracaine.
10
It makes vasodilatation ⇒ needs to be administered with a vasoconstrictor such as adrenaline (epinephrine).
Mepivacaine (Carbocaine)
N-(2,6-Dimethylphenyl)-1-methylpiperidine-2-carboxamide
It is similar to lidocaine except that it has a slightly longer duration of action and lacks the vasodilator activity of lidocaine. So, no need to be administered with a vasoconstrictor.
Bupivacaine (Marcaine)
CH
3
H
N
O
CH
3
N
C
4
H
9
N-(2,6-Dimethylphenyl)-1-butylpiperidine-2-carboxamide
The duration of action of bupivacaine is 2 to 3 times longer than that of lidocaine or mepivacaine.
11
Tocainide and Tolycaine
H
3
C
HN
O CH
3
C
NH
2
CH
3
H
3
C
HN
CH
3
O
N CH
3
COOCH
3
Tocainide Tolycaine
To minimize the unwanted CNS side effects (CNS depression, convulsions) these two drugs have been prepared and found to possess ↑ LA activity without CNS side effects.
Synthesis of Lidocaine
CH
3
NH
2
CH
3
Cl
O
Cl
CH
3 O
N
H
CH
3
Cl
HN
CH
3 O
N
H
CH
3
Lidocaine
N
12
3- Miscellaneous LAs
Phencaine
Dimethisoquin
Dyclonine
Benzyl Alcohol
13
Amino ketones phenols
Eugenol
Phenol
phenols phenols
14