new-local anaethetic
advertisement
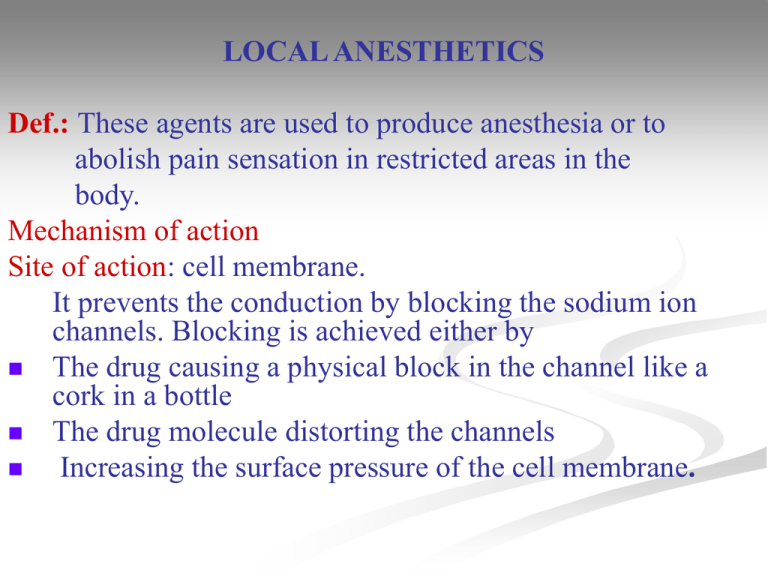
LOCAL ANESTHETICS Def.: These agents are used to produce anesthesia or to abolish pain sensation in restricted areas in the body. Mechanism of action Site of action: cell membrane. It prevents the conduction by blocking the sodium ion channels. Blocking is achieved either by The drug causing a physical block in the channel like a cork in a bottle The drug molecule distorting the channels Increasing the surface pressure of the cell membrane. Ideal Local Anesthetic It must have the following characters: 1) Nontoxic 2) Nonirritant 3) Produce vasoconstriction 4) Effective either topically or parenterally. 5) Reversible: means reversible blockade of sensory nerve fibers with minimal effect on the motor fibers. 6) Rapid onset with sufficient duration of action. Adverse Reactions As a result of overdose and its complete systemic absorption, it can cause: • CNS effects: Vomiting, nausea, convulsions coma with respiratory and heart failure. • CVS effects: Bradycardia, hypotension and shocklike state. • Some local reactions of allergic nature e.g. edema, pain, skin discoloration and neuritis. Treatment (Antidote): ultrashort-acting or short-acting barbiturate History Local anesthetics were derived from natural sources. A) Cocaine In 1532, the anesthetic properties of coca leaves became known to Europeans from the natives of Peru, who chewed the leaves for a general feeling of well-being and to prevent hunger. Later, the alkaloid cocaine was obtained from the coca leaves which causes anesthetic effect on the tongue. Carbomethoxy group H3C N H3C COOCH3 N COOH hy droly sis O H Tropin e moit y OH hot dil. acid. or alkali O Ecgonine Benzoy l group H (Tropine carboxy lic acid) COOH + + CH3OH 2 1 COOCH3 H 3C N No carbomethoxy group (no addicting liability ) 7 H3C N 3 8 6 5 H 4 Cocaine O O O O Benzoyl tropine Ecgonine = piperidine and pyrrolidine rings. The dotted portion of cocaine has been found to represent the anesthesiophoric function group. Cocaine was the first potent local anesthetic used clinically. Cocaine can not penetrate intact skin but is absorbed from mucous membranes. Cocaine blocks uptake of catecholamines (C.A.) at adrenergic nerve endings and so it is considered potent vasoconstrictor. This account for ulceration of nasal septum after administration of cocaine for long periods in higher dose. Cocaine has many disadvantages such as addiction, tissue irritations, poor stability in aqueous solutions and decomposition on sterilization. H 3C N No carbomethoxy group (no addicting liability ) O H O Benzoyl tropine Later, benzoyl esters of amino alcohols were synthesized, such as benzoyltropine. Benzoyltropine exhibited strong local anesthetic properties without any addicting liability. Thus, removal of the 2carbomethoxy group of cocaine also abolished the addiction. After that, esters of p-aminobenzoic acid e.g. procaine were discovered which not have severe local and systemic toxicity of cocaine. Synthetic compounds A) Ester-type or amino-esters or cocaine-type ( procaine-type). O They are classified into: H2N I] p-Aminobenzoate derivatives O CH2CH3 1)Benzocaine Ethyl 4-aminobenzoate Assay: Diazometrically. Disadvantages: its low aqueous solubility limited its usefulness as injectable agent. Uses: topically for surface anesthesia of mucous membrane. Unlike others, benzocaine not possess aliphatic amino gp required for salt formation. The free electrons on the aromatic amino gp are delocalized by the ring. Thus, formation of water soluble salt is not possible. O2N CH3 p-nitrotoluene Oxid. O2N 1) esterf ication Benzocaine COOH 2) reduction 2) Procaine hydrochloride O Et H2N 2 O 1 N . HCl Et 2-Diethylaminoethyl-4-aminobenzoate hydrochloride 1. 2. Procaine is the least toxic and widely used. Unlike benzocaine, procaine containing a basic amino group from which water soluble salts were prepared. In contrast to cocaine,it not causes vasoconstriction, so it is rapidly absorbed from site of inj. Most ester-type are used in a solution containing a vasoconstrictor as epinephrine to serve a dual purpose: The first one is to decrease the rate of absorption. Thus, localize the local anesthetic at the desired site to limit systemic toxicity. The second one is to prolong duration of action. 1) H2N Preparation: Cl + HN O C2H5 O C2H5 2) H2N + OH N HO conc. H2SO4 Procaine C2H5 Assay: Diazometrically. CH 120 - 130 C O 3) H N N + Procaine is used to form an insoluble salt with CH ONa Cl penicillin G. The low solubility accounts for the prolonged action of this salt. The amide derivative of procaine (procainamide HCl) is a cardiac depressant. 3) Chloroprocaine hydrochloride 2-Diethylamino-4-amino-2-chloro O C2H5 benzoate hydrochloride H2N N . HCl Assay: Non-aqueous titration. O CH o 2 5 2 5 2 2 5 Cl 4) Propoxycaine Hydrochloride It is 2-(Diethylamino) ethyl-4-amino -2-propoxybenzoate hydrochloride It is not stable to autoclaving. It has quicker onset and longer duration of action and more potent than procaine. It is used by injection for nerve block and infiltration anesthesia. O H2N C2H5 N O OC3H7 . HCl C2H5 5) Amethocaine (tetracaine) Hydrochloride: O HN N O C4H9 Preparation: . HCl CH3 2-(Dimethylamino)ethyl-4-butylaminobenzoate HCl H2N COOEt CH3CH2CH2CH2Br Na2CO3 CH3 N HO CH3 CH3 Trans esterfication NaOEt Assay: alkaloidal assay. Compound HN C4H9 COOEt • Tetracaine is one of the most easily absorbed drugs due to the presence of nonpolar n-butyl group. • Its solutions are more stable to hydrolysis than procaine and it may be sterilized by boiling. • *Mixture of sulfonamide and p-aminobenzoic acid local anesthetics should be avoided because of their hydrolysis led to p-aminobenzoic acid (PABA). Sulfonamides are considered competitive inhibitors of PABA in the biosynthesis of dihydrofolate. CH3 O II] Benzoate Derivatives C N CH2 CH2 CH3 . HCl 1) Meprylcaine HCl O CH3 • 2-Methyl-2-(propylamino)-1propanol benzoate HCl • It can be sterilized by autoclaving without decomposition. • It is used in dentistry in 2% solution containing epinephrine as an infiltration and nerve block anesthetic. 2) Cyclomethycaine sulfate (sufacaine) Assay: Spectrophotometrically. O 2 O O 1 3 CH3 N . H2SO4 3-(2-Methylpiperidino) propyl-4-(cyclohexyloxy) benzoate sulfate Uses: topically on burns(sunburns) and mucosa of rectum in 0.25-1%. not used for mucous membranes of upper respiratory system or eye. O CH3 3) Piperocaine HCl (Metycaine HCl) . HCl O N It differs from cyclomethycaine in the absence of cyclohexyloxy group. Its aqueous solutions are stable to sterilization by autoclaving. It is recommended for eye, nose and throat. Structure activity relationship The general structure of ester- type local anesthetics is as follows: O R Ar Et 1 O (CH2)n H2N O N 2 R Lipophilic Intermediate Hy drophilic portion chain portion N Et O reversed ester The lipophilic portion: It is essential for activity.This is a portion of aromatic acid whereas benzoic and p-amino-benzoic acids are the preferred ones. The carbonyl group must be conjugated with an aromatic nucleus whereas reversed esters have no local anesthetic activity. The esters of cinnamic acid are more active than those of phenyl acetic acid due to interruption of the extended conjugation by methylene gp between the aromatic ring and carbonyl gp. O OR OR O Conjugated Cinnamic acid OR O not conjugated phenyl acetic acid not conjugated b-phenyl propionic acid Introduction of electron-donating gps in the ortho or para positions of the ring increases conjugation and binding of drug to the receptor prolonging the action. NH2 (procaine),an alkylamino (tetracaine) or an alkoxy gp (propoxycaine) increase electron density to the aromatic ring by both resonance and inductive effects, While the opposite occur in case of electron-withdrawing (NO2, CO and CN). Tetracaine is 50-fold more potent than procaine. This may be due to the n-butyl gp increase lipid solubility propoxycaine, the presence of o-propoxy gp increase duration of action due to protection of ester gp from hydrolysis due to plasma esterases This is contrary to chloroprocaine which has shorter duration of action due to negative inductive effect of ochloro gp which pulls the electron density away from the carbonyl function. The intermediate chain It is alkyl chain of amino alcohol involved in the esters. The propylene gp –(CH2)3– provides the most active compounds, next ethylene, –(CH2)2– while methylene gp, – CH2–, makes the compounds too irritant. The branching with small alkyl gp around the ester function (e.g. meprylcaine) also hinders esterase catalysed hydrolysis prolonging the duration of action. The hydrophilic portion It is amine part of amino alcohols used to esterifies aromatic acids. Its advantage is its ability to form salts with inorganic acids producing water soluble compounds. It is observed that benzocaine which lacks the basic aliphatic amine, has potent local anesthetic activity. Thus, 3ry amine is needed for formation of water soluble salts, suitable for pharmaceutical preparations. The anesthetic activity increases with the size of the alkyl gps (R1, R2), the maximum being at C3-C4. R1 and R2 may be identical, unsaturated groups or hydrogen and alkyl group. 3ry amines useful local anesthetics. 2ry amines long acting but irritant. 1ry amines not active. B) Isogramine In 1930, the discovery of the local anesthetic activity of isogramine (isomer of alkaloid gramine,3-derivative) led to the synthesis of lidocaine (anilide or reversed amide). Lidocaine(xylocaine) is the first non-irritating, amide-type local anesthetic agent with lesser allergic reactions than esters. Its aqueous solution is stable because of the stablility of amide functionality. Structurally, lidocaine can be viewed as an open-chain analog of isogramine and thus is a bioisosteric analog of isogramine. CH3 O N H N(CH3)2 N CH3 H Isogramine Lidocaine 2-(Dimethylaminomethyl)indole N(C2H5)2 B)amino-amides or isogramine-type (lidocaine-type). 1) Lidocaine HCl or lignocaine HCl (Xylocaine) O HN H 3C Et N O Et O HN CH3 H 3C CH3 . HCl 2-(Diethylamino)-N-(2,6-dimethyl phenyl)acetamide HN N CH3 . HCl Mepivacaine HCl H 3C N CH3 C 4H 9 . HCl Bupivacaine N-(2,6-Dimethylphenyl)-1-methyl or butyl -2piperidinecarboxamide HCl Assay: non aqueous titration. Use: The salt is used for infiltration, peripheral nerve block and epidural anesthesia. Lidocaine is effective as antiarrhythmics. 2) Mepivacaine HCl (Carbocaine) Its duration of action is longer than lidocaine. 3) Bupivacaine HCl (Marcaine) Its duration of action is 2-3 times longer than lidocaine or mepivacaine. H 4) Dibucaine HCl (Cinchocaine HCl) Nupercaine O N Et N Assay: non aqueous titration. Et It is the most potent, toxic and . HCl CH longest acting one N O Used topically and in 2-Butoxy-4-[2-(diethylamino) spinal anesthesia. ethyl]cinchonamide Structure Activity Relationship: (amino amide series) The general structure of local anesthetic can be represented as follow: 4 Lipophilic portion Intermediate chain 9 Hy rophilic portion Lipophilic portion: The lipophilic portion is essential for activity and consists of phenyl group attached to CO function (sp2 carbon) through NH gp. Thus, the COOH gp of the amino-ester series is replaced by its isosteric NHCO moiety in amino-amide series. Substitution of the phenyl with a methyl gp in the 2- or 2- and 6position enhances activity. The amide bond is more stable to hydrolysis than the ester. In addition, o,o`-methyl substituents provide steric hindrance to the hydrolysis of the amide bond. The intermediate chain In lidocaine series, lengthening of the alkylene chain from one to two or three increases pKa from 7.7 to 9.0 or 9.5, respectively reducing local anesthetic potency. Here, branching around the amide function (etidocaine), also hinders amidase catalyzed hydrolysis prolonging the duration of action. Advantages of lidocaine derivatives over procaine ones 1. More stable to hydrolysis. 2. Can be sterilized by autoclaving. 3. More potent. 4. Lower side effects: less local irritation than procaine type. 5. Used as alternatives for patients sensitive to procaine type local anesthetic. 6. 7. Effective without vasoconstrictors. It used for patient sensitive to epinephrin. Lidocaine derivatives undergo enzymatic degradation not in plasma but primarily in the liver through degradation of amide bond. N.B.: Patient possessing a genetic deficiency in the enzyme pseudocholinesterases is unable to hydrolyze ester-type local anesthetic agents and show reduced tolerance to these drugs. Thus, amide-type agents are preferable. On the other hand, patients with liver diseases may show reduced tolerance to amide-type agents due to they are mainly metabolized in liver. Thus, ester-type drugs are preferable. Most of clinically used local anesthetics have pKa 89.5. Drugs with higher pKa values are almost completely ionized at physiological pH and therefore are hindered in reaching the receptor sites. For this same reason, local anesthetics can be ineffective in inflammation areas because in these areas, pH being lower, facilitates ionization of their molecules and consequently hinders their penetration into nerve fibers. On the other side, compounds with lower pKa values are not sufficiently ionized and although they reach the target are less potent.