Pria – Principles of Cancer Treatment
advertisement

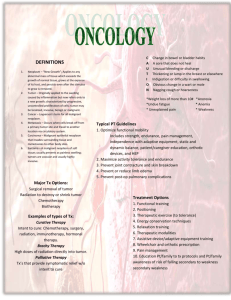
VELEZ COLLEGE DEPARTMENT OF OCCUPATIONAL THERAPY F.RAMOS ST. CEBU CITY Principles of Cancer Treatment SUBMITTED BY: CHIONGBIAN, APRIL GRACE A. BSOT-IV SUBMITTED TO: DR. GERRARD DENNIS UY, MD The goal of cancer treatment: eradicate the cancer. If this primarygoal cannot be accomplished, the goal of cancer treatment shifts to palliation, the amelioration of symptoms, and preservation of quality of life while striving to extend life. When cure of cancer is possible, cancer treatments may be undertaken despite the certainty ofsevere and perhaps life-threatening toxicities. Every cancer treatment has the potential to cause harm, and treatment may be given that producestoxicity with no benefit. The therapeutic index of many interventionsis quite narrow, and most treatments are given to the point of toxicity. When the goal is palliation, careful attention to minimizing the toxicity of potentially toxic treatments becomesa significant goal. Irrespective of the clinical scenario, the guidingprinciple of cancer treatment should be primum succerrere,, “first hasten to help.” Radical surgical procedures, large-field hyperfractionated radiation therapy, high-dose chemotherapy, and maximum tolerable doses of cytokines such as interleukin (IL) 2 are all used in certain settingswhere 100% of the patients will experience toxicity and side effectsfrom the intervention and only a fraction of the patients willexperience benefit. One of the challenges of cancer treatment is to use the various treatment modalities alone and together in a fashion that maximizes the chances for patient benefits Cancer treatments divided into four main types: Surgery Radiation therapy Chemotherapy Biologic therapy modalities are often used in combination, and agents in one category can act by several mechanisms. Oncology, the study of tumors including treatment approaches, is a multidisciplinary effortwith surgical-, radiotherapy-, and internal medicine–related areasof expertise. Treatments for patients with hematologic malignanciesare often shared by hematologists and medical oncologists. Cancer mimics an organ attempting to regulate an own growth. Cancers have no limit on how much growth should be permitted. Normal organs and cancers share the same properties: Population of cells in cycle and actively renewing Population of cells not in cycle cancer stem cells, Properties are being elucidated. The stem cell fraction may define new targets for therapies that will retard their ability to reenter the cell cycle. PRINCIPLES OF CANCER THERAPY Prophylaxis Cancer can be prevented by surgery in people who have premalignantlesions resected Those who are at increased risk of cancer from either an underlyingdisease Presence of genetic lesions or a developmental anomaly Prophylactic surgery is more radical than surgeries used to treat after the cancer develops The assessment of risk involves many factors andshould be undertaken with care before advising a patient to undergosuch a major procedure. Diagnosis Obtain as much tissue safety as possible light-microscopic inspection of a tumor for pattern of growth, degree of cellular atypia, invasiveness, and morphologic features that aid in the differential diagnosis Histologically similar tumors may have very different gene expression patterns when assessed by such techniques as microarray analysis using gene chips goals are best met by an excisional biopsy in which the entire tumor mass is removed with a small margin of normal tissue surrounding it If an excisional biopsy cannot be performed, incisional biopsy is the procedure of second choice. A wedge of tissue is removed, and an effort is made to include the majority of the cross-sectional diameter of the tumor in the biopsy to minimize sampling error. Core-needle biopsy usually obtains considerably less tissue, but this procedure often provides enough information to plan a definitive surgical procedure. Fine-needle aspiration generally obtains only a suspension of cells from within a mass. Staging important component of patient management is defining the extent of disease. Radiographic and other imaging tests can be helpful in defining the clinical stage; Pathologic staging requires defining the extent of involvement by documenting the histologic presence of tumor in tissue biopsies obtained through a surgical procedure. Treatment Surgery is the most effective means of treating cancer removal of tumor can obtain important benefits, including local control of tumor, preservation of organ function, debulking that permits subsequent therapy to work better, and staging information on extent of involvement. laparoscopic approaches are being used to address primary abdominal and pelvic tumors. Lymph node spread may be assessed using the sentinel node approach, in which the first draining lymph node a spreading Tumor would encounter is defined by injecting a dye into the tumor site at operation and then resecting the first node to turn blue chemotherapy and/or radiation therapy is delivered to reduce the size of the tumor and clinically control undetected metastatic disease. Such therapy is followed by a surgical procedure to remove residual masses; this is called neoadjuvant therapy Palliation Surgery is employed in a number of ways for supportive care Surgical bypass of gastrointestinal, urinary tract, or biliary tree obstruction can alleviate symptoms and prolong survival. Rehabilitation Assure proper ambulation PRINCIPLES OF RADIATION THERAPY Physical properties and biologic effects Radiation is a physical form of treatment that damages any tissue in its path; selectivity for cancer cells may be due to defects in a cancer cell’s ability to repair sublethal DNA and their damage. Therapeutic radiation is delivered in three ways: (1) teletherapy, with beams of radiation generated at a distance and aimed at the tumor within the patient; (2) brachytherapy, with encapsulated sources of radiation implanted directly into or adjacent to tumor tissues; (3) systemic therapy, with radionuclides targeted in some fashion to a site of tumor. - X-rays and gamma rays are the forms of radiation most commonly used to treat cancer. - orbital electron ejection is called ionization. - waves behave biologically as packets of energy, called photons tissues that the beam passes through to get to the tumor are called the transit volume Radiation is quantitated on the basis of the amount of radiation absorbed in the patient APPLICATION TO PATIENTS Teletherapy Radiation therapy can be used alone or together with chemotherapy to produce cure of localized tumors and control of the primary site of disease in tumors that have disseminated Individualized treatment planning employs lead shielding tailored to shape the field and limit the radiation exposure of normaltissue. Brachytherapy placing a sealed source of radiation into or adjacent to the tumor and withdrawing the radiation source after a period of time precisely calculated to deliver a chosen dose of radiation to the tumor. Radionuclides and Radioimmunotherapy Nuclear medicine physicians or radiation oncologists may administer radionuclides with therapeutic effects. Iodine 131 is used to treat thyroid cancer since iodine is naturally taken up preferentially by the thyroid Monoclonal antibodies and other ligands can be attached to radioisotopes by conjugation Photodynamic Therapy Some chemical structures (porphyrins, phthalocyanines) are selectively taken up by cancer cells by mechanisms not fully defined. When light, usually delivered by a laser, is shone on cells containing these compounds, free radicals are generated and the cells die. Hematoporphyrins and light are being used with increasing frequency TOXICITY Though radiation therapy is most often administered to a local region, systemic effects, including fatigue, anorexia, nausea, and vomiting, may develop that are related in part to the volume of tissue irradiated, dose fractionation, radiation fields, and individual susceptibility. Bone is among the most radioresistant organs, radiation effects being manifested mainly in children through premature fusion of the epiphyseal growth plate. - Chronic toxicities are more serious. Radiation of the head and neck region often produces thyroid failure. Cataracts and retinal damage can lead to blindness. Salivary glands stop making saliva, which leads to dental caries and poor dentition. PRINCIPLES OF CHEMOTHERAPY Medical oncology subspecialty of internal medicine that cares for and designs treatment approaches to patients with cancer, in conjunction with surgical and radiation oncologists. END POINTS OF DRUG ACTION Chemotherapy agents may be used for the treatment of active, clinically apparent cancer eradicate a local tumor or as part of multimodality approaches to offer primary treatment to a clinically localized tumor. Chemotherapy is routinely used in “conventional” dose regimens potentially life-threatening complications that require intensive support, usually in the form of hematopoietic stem cell support from the patient (autologous) or from donors matched for histocompatibility loci (allogeneic) CANCER DRUGS: OVERVIEW AND PRINCIPLES FOR USE 4 broad types: conventional therapy agent targeted agents hormonal therapies biologic therapies 2 valuable outcomes of therapies mentioned: induce cancer cell death induce cancer cell differentiation cell death: necrosis o cell death induced, for example, by physical damage with the hallmarks of cell swelling and membrane disruption apoptosis o highly ordered process whereby cells respond to defined stimuli by dying, and it recapitulates the necessary cell death observed during the ontogeny of the organism. Anoikis o refers to the death of epithelial cells after removal from the normal milieu of substrate, particularly from cell-to-cell contact. Chemotherapeutic agents used in cancer treatment Direct DNA-interactive agents Synthesis or s-phase of the cycle divided into “phase-nonspecific” agents, which can act in any phase of the cell cycle, and “phasespecific” agents, which require the cell to be at a particular cell cycle phase to cause greatest effect. Formation of Covalent DNA adducts Alkylating agents as a class are cell cycle phasenonspecific agents. Broken” or cross-linked DNA is intrinsically unable to complete normal replication or cell division; further activates cell-signaling pathways that can precipitate apoptosis Cyclophosphamide is inactive unless metabolized by the liver to 4-hydroxy-cyclophosphamide, which decomposes into an alkylating species, as well as to chloroacetaldehyde and acrolein. Ifosfamide is a cyclophosphamide analogue also activated in the liver, Nitrogen mustard (mechlorethamine) is the prototypic agent of this class, decomposing rapidly in aqueous solution to potentially yield a bifunctional carbonium ion Chlorambucil causes predictable myelosuppresion, azoospermia, nausea and pulmonary side effects. Busulfan causes profound myelosuppression, alopecia and pulmonary toxicity but is relatively lymphocyte sparing Procarbazine is metabolized in the liver and possibly in tumor cells to yield a variety of free radical and alkylating specieas Cisplatin requires administration with adequate hydration, including forced diuresis with mannitol to prevent kidney damage Hypomagnesemia attends cisplatin use and can lead to hypocalcemian and tetany Carboplatin displays less nephro- , oto-, and neurotoxicity. Oxaliplatin is a platinum analog with noteworthy activity in colon cancers refractory to other treatments. ANTITUMOR ANTIBIOTICS AND TOPOISOMERASE POISONS Antitumor antibiotics - Substances produced by bacteria that appear to provide a chemical defense against other hostile microorganisms. Topoisomerase poisons Natural products or semisynthetic species derived ultimately from plants and modify enzymes that regulate the capacity of DNA to unwind to allow normal replication or transcription. Topoisomerase I o Creates sing-strand breaks that then rejoins following the passage of other DNA strand Topoisomerase II o Double strand breaks through which another segment of DNA duplex passes before rjoining Doxorubicin Intercalate into DNA altering DNA structure, replication and topoisomerase II function. Undergo reduction reaction Causes predictable yelosuppresion, alopecia, nausea and mucositis. Bleomycin Mixture of glycopeptides that have the unique feature of forming complexes with iron whil also bound to DNA Cleared rapidly but augmented skin and pulmonary toxicity in the presence of renal failure Vesicant and can be administered intravenously, intramuscularly of subcutaneously Mitomycin C Undergoes reduction of its quinone function to generate a bifunctional DNA alkulataing agent Active anti-neoplastic agent with a number of unpredictable toxicities including: o Delayed bronchospasm 12-24h after dose and chronic fibrosis syndrome more frequent at doses 50-60mg/ m2 Mitoxantrone Synthetic compound that was designed to recapitualt features of doxorubicin but with less cardiotoxicity. Cases of actue promyelocytic leukima Etoposide Synthetically derived from the plant product podophyllotoxin. Binds directly to topoisomerase II and DNA in a reversibleternary complex Alkali-labile DNA bond Camptothecin Extracts of a Chinese tree and had notable antileukemia activity INDIRECT EFFECTORS OF DNA FUNCTION: Antimetabolites Antimetabolites Compounds with structural similarity to precursors of purines or pyrimidines, or compounds that interfere with purine or pyrimidine synthesis. Cause DNA damage indirectly abnormal timing or progression through DNA synthesis, or altered function of pyrimidine and purine biosynthetic enzymes. Methotrexate Inhibits dihydrofolate reductase Cleared by the kidney bia both glomerular filtration and tubular section Bone marrow suppression and mucosal irritation and renal failure at high doses owing to crystallization in renal tubules Low-dose cause hepatic fibrosis Pemetrexed novel folate-directed antimetabolite multitargeted inhibiting the activity of several enzymes. Received along with low-dose folate and vitamin B12 supplementation. Cytosine arabinoside Incorporated into DNA after formation of ara-CTP, resulting S-phase-related toxicity Adverse effects include nausea, diarrhea, stomatitis, chemical conjunctivitis and cerebellar ataxia. Fludarabine phosphate Prorug of F-adnine arabinoside Designed to diminish the susceptibility of ara-A to adenoside deaminase Causes inhibition of ribonucleotide reductase and susceptibility to apoptosis Renal failure and CNS dysfunctions are notable toxicities Asparaginase Bacterial enzyme that causes breakdown of extra-cellular aspargine required for protein synthesis - Effectively stops tumor cell DNA synthesis Hypersensitivity reactions are common Mitotic Spindle Inhibitors Vincristine is metabolized by the liver, and dose adjustment in the presence of hepatic dysfunction is require. o Neuropathic effects: jaw pain, paralytic ileus, urinary retention, and the syndrome of inappropriate antidiuretic hormone secretion Vinorelbine is a vinca alkaloid that appears to have differences in resistance patterns in comparison to vincristine and vinblastine; it may be administered orally. taxanes stabilize microtubules against depolymerization. “stabilized” microtubules function abnormally and are not able to undergo the normal dynamic changes of microtubule structure and function necessary for cell cycle completion Taxanes include: o Paclitaxel o docetaxel Estramustine was originally synthesized as a mustard derivative that might be useful in neoplasms that possessed estrogen receptors. Hormonal Agents Glucocorticoids are generally given in “pulsed” high doses in leukemias and lymphomas, where they induce apoptosis in tumor cells. o Cushing’s syndrome or inadvertent adrenal suppression o Pneumocystis pneumonia Tamoxifen is a partial estrogen receptor antagonist; it has a tenfold greater antitumor activity in breast cancer patients whose tumors express estrogen receptors than in those who have low or no levels of expression Aromatase refers to a family of enzymes that catalyze the formation of estrogen in various issues, including the ovary and peripheral adipose tissue and some tumor cells. Diethylstilbestrol (DES) acting as an estrogen at the level of the hypothalamus to downregulate hypothalamic luteinizing hormone (LH) production results in decreased elaboration of testosterone by the testicle. Total Androgen Blockade o Combined use orchiectomy or leuprolide plus flutamide Targeted therapies Hematopoietic Neoplasms o Imatinib Targets the ATP binding site of protein tyrosine kinase that is formed as the result of the chromosome 9,22 translocation producing the Philadelphia chromosome in CML o Nilotinib Tyrosine protein kinase inhibitor with a similar spectrum of activity to imatinib, but with increased potency and perhaps better tolerance by certain patients. o All-trans-retinoic acid Targets the OML retinoic acid receptor alpha fusion protein Adverse effects: Headaches with or without pseudotumor cerebri Gastrointestinal cutaneous toxicities o Bortezomib Inhibitor of the proteasome, the multi-subunit assembly of protease activities responsible for the selective degradation of proteins important in regulating activation of transcription factores. o Vorniostat Inhibitor of histone deactylases, responsible for maintaining the proper orientation of histones on DNA, with resulting capacity for transcription factors and therefore increased expression of genes that are selectively repressed in tumors. o DNA methyltransferase inhibitors Increase transcription of genes silenced during the pathogenesis of a tumor by causing demethylation of the methylated cytosines that are acquired as an epigenetic modification of DNA - Solid tumors o Small-molecule epidermal growth factor antagonists Act at the ATP binding site of the EGF receptor tyrosine kinase. o o Gefitinib showed evidence of responses in a small fractions of patients with nonsmall cell lunch cancer. Multitargeted kinase antagonists Small-molecule ATP site-directed antagonists that inhibit more than one protein kinase. Hand-foot syndrome Erythema and desquamtation of the distal extremities Acute Complications of Cancer Chemotherapy Myelosuppresion o Common cytotoxic chemotherapeutic agents almost invariably affect bone marrow function o Complications result from the predictable sequelae of the missing cells’ function o Febrile neutropenia Clinical presentation of fever in a neutropenic patient with an uncontrolled neoplasm involving the bone marrow or, more usually, in a patient undergoing treatment with cytotoxic agents. Management: empirical coverage with antibiotics for the duration of neutropenia o Primary prophylaxis G-CSF to patients receiving cytotoxic regiments is associated with 20% incidence of febrile neutropenia Nausea and vomiting o Most common side effect of chemotherapy administration o Acute: within 24 hours o Delayed: >24 hours o Antineoplastic agents vary in their capacity to cause nausea and vomiting o Emesis – reflex caused by stimulation of the vomiting center in the medulla - Diarrhea o Regimens that include fluorouracil infusions and/or irinotecan o Immediate or delayed (48-72 hours) - Mucositis o Irritation nd inflammation of the mucous membranes particularly afflicting the oral and anal mucosa o Due to damage to the proliferating cells at the base of the mucosal squamous epithelia or in the intestinal crypts. - Alopecia o Antimetabloites more variably associated with alopecia - Gonadal dysfunction and pregnancy o Cessation of ovulation and azospermia reliably result from alkylating agents o Female – experience amenorrhea with anovulation after alkylating agent therapy BIOLOGIC EFFECTS Immune mediators of antitumor effects Tumors have variety of means of avoiding immune system: 1. Often only subtly different from their normal counterparts 2. They are capable of downregulating their major histocompatibility complex angtigens 3. Inefficient at presenting antigens to the immune system 4. Cloak themselves in a protective shell of fibrin to minimize contact with surveillance mechanisms 5. Produce a range of solumbe molecules including potential immune targets Cell Mediated Immunity 1. Allogeneic T cells are transferred to cancer-bearing hosts in 3 major settings a. Allogeneic bone marrow transplantation b. Pure lymphocyte transfusions following bone marrow recovery c. Pure lymphocyte transfusions following immunosuppressive therapy 2. Autologous T cells are removed from the tumor-bearing host, manipulated in several ways in vitro and given back to the patient. 2 major classes a. To develop tumor antigen-specific T cells and expand them to large numbers over many weeks ex vivo before administration b. To activate the cells with polyclonal stimulaters 3. Tumor vaccines are aimed at boosting T cell immunity. Antibodies Not very effective at killing cancer cells Easier for the tumors to fend off. Antibodies to CD52 are active in chronic lymphoid leukemia and T cell malignancies EGF-R directed antibodies have activity in colorectal cancer Anti-VEGF antibody bevacizumab shows little evidence of anti-tumor effect when used alone, but with chemotherapeutic agents, it improves the magnitude of tumor shrinkage and time to deases progression Side effects: o Infusion-related hypersensitivity reactions o Acneiform rash Cytokines Greater than 70 separate proteins and glycoproteins with biologic effects in humans. Interferon alpha beta and gamma o Not curative for any tumor but can induce partial responses in follicular lymphoma, hairy cell leukemia, CML melanoma, and Kaposi’s sarcoma IL – 1 through 29 o IL-2 exer its antitumor effects indirectly through augmentation of immune function o IL-2 associated with myriad clinical side effects: Intra vascular volume depletion Capillary leak syndrome Adult respiratory distress syndrome Hypotension Fever Chills Skin rash Impaired renal and liver function GENE THERAPY No gene therapy has been approved for routine clinical use -