CARDIOVASCULAR SYSTEM STUDY GUIDE 2 (Pp. 334 – 339)
advertisement

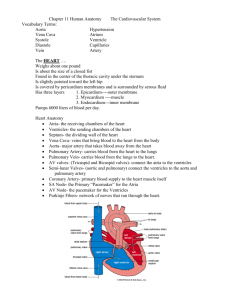
3rd 9 weeks Review: Anatomy Study Guide Senses-Cardiovascular System (Ch 8-11) Study: NB p. 1-23 Focus on Endocrine/Blood Concept Map, Note Summaries and Labeling Diagrams KEY FOR SENSES 1 & 2 nose-chemo, tongue-thermo and chemo, eye-photo, ear- mechanoreceptors 3. DEAFNESS: Auditory nerves are damaged, CATARACTS: lens is cloudy, GLAUCOMA: increase in pressure of the eye, 4. PATHWAY OF EAR pinna, auditory canal, eardrum, malleus, incus, stapes, oval window, fluid in cochlear canals (upper and middle/ lower) 5. hammer, anvil, stirrup 6. EARDRUM middle, AUDITORY CANAL outer and inner OSSICLES EYE: A-Iris B-Lens-C- Cornea D- Sclera D2 Retina E-Optic Nerve F-Optic Disk (Blindspot) EAR: Auditory/Eustachian Tube, B) Cochlea C) Semicircular D) Incus/Anvil E) Malleus/Hammer F) Pinna/Auricle G) Vestibule H Stapes I-Eardrum (Tympanic Membrane) J Ex. Auditory Canal 1. Ch 8 Senses: What types of receptors are found in: Nose, Tongue, Eye, Ear Choices include (chemo, thermo, photo and mechanoreceptors) 2. Anatomically describe what happens when someone is affected by: 3. Deafness, Cataracts, Glaucoma, Myopia 4. Look at your (Senses Labeling Sheet p. 2)Trace the pathway of sound through the ear. Remember to include auditory Ossicles (malleus, incus, stapes). 5. What is the common name for each of the three Ossicles above? 6. Where would you find the: Tympanic Membrane, Auditory Canal, Cochlea Ossicles (Outer, Middle, Inner Ear)? a. Sclera, Cornea, Vitreous Humor, Optic Nerve, Fovea Centralis LABELING: Label & provide function for ear & eye: Ch 9 Endocrine System: Look at your Endocrine Concept Map and list hormones for the following glands: Gland Thyroid Hormones T3, T4, Calcitonin Functions METABOLIC RATE Parathyroid PTH (Parathyroid)/ Bone Density DISORDER Goiter-Cyst/Bulge in Neck (Iodine Deficency) OSTEOMALACIA, OSTEOPOROSIS Hypothalamus Adrenal Gland Pituitary Gland Thymus Pancreas Ch 10 Blood : List all leukocytes and their functions. 1. What is the trick to remember their order of abundance? Never LET MONKEYS EAT BANANAS NEUTROPHILS-MOST ABUNDANT, MONOCYTES, EOSINOPHILS, BASOPHILS (LEAST ABUNDANT) 2. How many leukocytes does one have in comparison to red blood cells (erythrocytes)? 1 FOR EVERY 100 RBC. 3. What is the typical lifespan of a red blood cell? 100-120 DAYS 4. What are WBC, RBC & platelet clinical names? LEUKOCYTES;ERYTHROCYTES, THROMBOCYTES 5. Platelets are fragments of which leukocyte? MEGAKARYOCYTES 6. Using Figure 10.1 Trace the Pathway of Blood Cell development. 7. What type of blood cell gives rise to almost all of the leukocytes, erythrocytes, platelets? MYELOID 8. What type of stem cell produces lymphocytes? LYMPHOID Ch 11: Cardiovascular System: The Superior Vena Cava drains into which chamber….RIGHT ATRIUM CARDIOVASCULAR SYSTEM STUDY GUIDE 1 (Pp. 328 – 334) 1. Simply stated, what is the major function of the cardiovascular system? TO TRANSPORT GASES AND NUTRIENTS THROUGHOUT THE BODY 2. What is the cardiovascular system's transport vehicle? THE HEART & VESSELS 3. List 4 categories of materials carried in the blood. FORMED ELEMENTS, 4. What provides the force needed to move blood around the body? BLOOD PRESSURE 5. What is the approximate size of the human heart? 1 FIST (APROX 1 LB) 6. Describe the location of the heart. IN THE THORACIC CAVITY (5TH INTERCOSTAL SPACEPERICARDIUM) 7. What is the more pointed part of the heart called? In which direction does it point? APEX; LEFT HIP 8. Where does one place a stethoscope to count the heart rate? AT THE BASE 9. Where is the base of the heart? ANTERIOR OF HEART (TOP) 10. What is the pericardium? Of which type of tissue is it made? SAC MADE OF CONNECTIVE TISSUE 11. What is the purpose of the fluid produced by the pericardial membranes? SYNOVIAL FLUID REDUCES FRICTION 12. What name is given to an inflammation of the pericardium? PERICARDITIS 13. What dangerous situation can result? INFECTION; DEATH 14. Describe the construction of the semilunar valves. MOON-LIKE STRUCTURE 15. Under what conditions are the semilunar valves open? DURING SYSTOLE (HIGH PRESSURE 16. What causes the semilunar valves to close? Why is this important? 17. Describe the timing of the opening and closing of the 4 valves. 18. What problem results from an incompetent valve? BLOOD LOSS 19. What is valvular stenosis and what causes it? HARDENING OF VALVES- AGE/DIET 20. What treatment is there for valves that do not work properly? VALVE REPACEMENT (BALOON AORTIC REPLACEMENT-REMOVE CLOTS) 21. Of what use to the heart muscle is the blood that flows through its chambers? NONE THIS BLOOD DOESN’T NOURISH THE HEART 22. How, then, does the heart muscle get oxygen and nutrients? CAROTID SINUS 23. Why is it unhealthy for the heart to beat too fast? DEREGULATES CARDIAC CYCLE 24. What is angina? What is a myocardial infarction? ANGINA PECTORIS-CHEST PAIN LACK OF BLOOD/OXYGEN TO HEART. MYOCARDIAL INFARCTION-CLINICAL TERM FOR HEART ATTACK MYOCARDIAL TISSUE DIES. 25. What distinguishes Pulmonary Veins from other veins in the body? ONLY OXYGEN RICH VEINS IN BODY CARDIOVASCULAR SYSTEM STUDY GUIDE 2 (Pp. 334 – 339) 1. How many times per day are the 6 L of blood circulated through the body? 3x/MIN ( 60 MIN x 24 HRS 4320 TIMES /DAY) 2. What is the responsibility of the autonomic nervous system to the heart? CONTROL BLOOD PRESSURE 3. What is the responsibility of the intrinsic conduction system of the hearT? SEND ELECTRICAL IMPULSES 4. Why is the intrinsic conduction system not like tissue found anywhere else in the body? NERVE BUNDLES ARE SEGMENTED 5. In which direction does the heart muscle depolarize? UNIDIRECTIONAL (ATRIA-VENTRICLE) TOP DOWN 6. What is the average contraction rate of a normal healthy heart? 70 BPM 7. What is the function of the SA node? REGULATE CARDIAC CYCLE 8. What is the common name of the SA node? PACEMAKER 9. Explain what would happen to the heart's beating if the AV node was damaged. What is this condition called? FIBRILLATION 10. Under what conditions might an artificial pacemaker be required? WHEN MYOCARDIUM IS DAMAGED/ HEART ATTACK 11. Define ischemia. DECREASED BLOOD FLOW TO HEART 12. What happens when the heart is in fibrillation? IRREGULAR HEART IMPULSES 13. Why is fibrillation dangerous? BLOOD CAN’T CIRCULATE THROUGH HEART/CHAMBERS CAN’T FILL 14. Define tachycardia. RAPID HR GREATER THAN 100 BPM (BEATS PER MIN) 15. Define bradycardia. SLOWER THAN 40 BPM 16. How does the timing of the contraction of the atria compare to each other? THEY SERVE AS A DUAL PUMP AND LEFT ATRIA CONTRACT ALMOST SIMULTANEOUSLY (REVIEW CARDIAC CYCLE TABLE BELOW) 17. Define systole and diatole. To the action of which chambers do these words refer? SYSTOLE-VENTRICULAR CONTRACTION; DIASTOLE-LOWER PRESSURE ATRIA RELAX 18. What is the length of one cardiac cycle? (0.8 SEC) 19. What 2 syllables describe the heart sounds? LUB DUP 20. What causes each of the sounds that the heart makes? LUB-VENTRICLES CLOSING DUP- SHARPER NOISES EJECTS BLOOD INTO THE AORTA-SYSTEMIC & PULMONARY CIRCUIT 21. What is a heart murmur? MITRAL VALVE DOESN’T CLOSE ALL THE WAY 22. What causes the blood to make sounds when there is a murmur? BLOOD LEAKAGE 23. In which people (ages) are heart murmurs fairly common? Why is this so? 24. Define cardiac output. AMOUNT OF BLOOD EJECT THROUGH EACH CHAMBER x HEART RATE 25. Define stroke volume. AMOUNT OF BLOD EJECTED /CHAMBER 26. What causes the stroke volume to increase? STROKE VOLUME- HEART RATE, EXTERNAL STRESSORS 27. What percent of the blood in the ventricles is pumped out at a time? 28. What does Starling's law say is the critical factor that controls the stroke volume? 29. What factor determines how much the heart muscle is stretched? EXERCISE, STRESSORS 30. Name a factor that changes that affects venous return. HORMONAL, AUTONOMIC NERVOUS SYSTEM 31. Name 2 factors that will decrease stroke volume. HEART SIZE, OVERLOAD 32. Name 4 factors that influence heart rate. DISEASE, ANEMIA, METABOLISM, ORGAN ISSUES 33. What is the effect of physical or emotional stress on the heart? OVERWORKS THE HEART 34. Name 2 hormones that affect heart rate. ANGIOTENSIN; ADH, RENIN 35. What can a deficiency of calcium do to the heart? AFFECTS THE Q-T INTERVAL; HYPOTENSION What about hypercalcemia? HYPERTENSION (HIGH BLOOD PRESSURE) 36. How might the heart respond to a deficiency of potassium? DYSRHYTHMIAS, PALPITATIONS 37. What is the resting heart rate range of a fetus? 110-160- BPM 38. What is the average heart rate of females? 60-70 BPM 39. What is the average heart rate of males? 90-100 BPM 40. Why does your heart rate increase when you have a fever? YOU ARE FIGHTING AN INFECTION 41. Under what circumstances does congestive heart failure occur? ARTERIAL BLOCKAGE 42. Define atherosclerosis. HARDENING OF THE ARTERIES 43. List 3 factors that can weaken the heart and lead to congestive heart failure. BLOCKAGE, HYPERTENSION, HIGH CHOLESTEROL 44. Why does a person who has failure of the left side of the heart have difficulty breathing? ISSUES WITH AORTIC output 45. Why does a person who has failure of the right side of the heart have edema (swelling) of the feet and ankles, etc? Issues with blood flow to the pulmonary circuit (oxygen deficiency) 46. What is the highest oxygen concentration vessel in fetal circulation? UMBILICAL VEIN 47. Which hormone is responsible for blood cell formation? ERYTHROPOEITIN Which chemical starts hemostasis (blood clotting)? SEROTONIN 48. Which vessels are found under the a) arm, SUBCLAVIAN b) hip region ILLIAC c), abdominal region ABDOMINAL AORTA d) liver VESSELS e) foot ? DORSAL PEDALIS 49. Name the 3 layers of the heart. Which one would contain heart muscle? EPICARDIUM, MYOCARDIUM, ENDOCARDIUM; MUSCLE: MYOCARDIUM VESSELS: TUNICA EXTERNA, TUNICA MEDIA (MUSCLE- THICKER IN ARTERIES THAN VEINS), TUNICA INTERNA (EPITHELIUM) 50. What is the clinical term for the “pacemaker”? SINOATRIAL NODE [3] 51. Stages of the cardiac cycle [edit] AV Semilunar valves* valves† Status of ventricles and atria • Atria contract and pump blood 1. Atrial Systole open closed 2. Isovolumetric Contraction closed closed • Ventricles, already partially filled from phase 5, receive last ~30% of blood, for a final resting volume of approximately 130mL. • Ventricles begin to contract. Ventricular muscle initially shortens only a little, but intraventricular pressure rises sharply • Ventricular volume unchanged • Pressures in left and right Ventricle exceed pressures in Aorta (80mmHg) and Pulmonary Artery (10mmHg). Ejection is rapid at first, slowing down as systole progresses. 3. Ventricular Ejection closed 4. Isovolumetric Relaxation closed open closed • Amount ejected each ventricle per stroke at rest is 70-90mL. Approximately 50mL of blood remains in each ventricle at the end of systole • Valves close as Ventricles relax and pressure within Ventricles drops below 120mmHg. This ends once Ventricular Pressure falls below Atrial pressure and AV valves open • pump blood to rest of body • ventricles relaxed 5. Ventricular Filling open closed • ventricles passively fill with approximately 70% of their final volume. As the ventricles fill, rate of filling decreases and the AV valves drift towards closing • atria expand and are filling * AV (atrioventricular) valves: 1) mitral valve – between the left atrium and the left ventricle 2) tricuspid valve – between the right atrium and the right ventricle † Semilunar valves: 1) aortic valve – between the left ventricle and the aorta 2) pulmonic valve – between the right ventricle and the pulmonary artery ADDITIONAL PRACTICE KEY Cardiovascular Study Guide Isengard-Anatomy CP Learning Objectives: RBC & WBC Formation (Red Blood Cell terms, reticulocyte, granulocyte, myeloid stem cells) Red blood cells are formed with reticulocytes. They originate in bone marrow and will be recycled in the spleen. Various hormones are required for RBC formation. Erythropoeitin is one of the main hormones. -White Blood Cells are categorized as granulocytes or agranulocytes (possessing no granules). Most WBCs arise from myeloid stem cells with the exception of the lymphocytes. Granulocytes include neutrophils, eosinophils & basophils Agranulocytes are the monocytes ,lymphocytes Steps of Hemostasis (Blood Stoppage) 1) Vascular Spasms (Serotonin Secretion) 2) Platelet Plug- Prothrombin Activator-forms plug 3) Fibrinogen will generate fibrin ( a tissue that will cover the injury) Steps of Clotting Cascade (Diagram these steps below) Prothrombin, Thrombin, etc. http://memorize.com/blood-human-anat-and-phys-7th-ed-marieb Name the hormones responsible for producing: Erythrocytes-Erythropoeitin Leukocytes-Interleukins &Colony Stimulating Factors (CSFs) Platelets-Thrombopoeitin Distinguish the differences between antibodies and antigens. Antigens are markers that identify the blood type as a person’s own(for example, Type A blood would possess A antigens. Antibodies are generated as an immune response to protect blood from foreign agents. For example,Type A blood would produce B antibodies and vice versa. Identify these in the table below List the steps of the cardiac cycle f c d e a e a h g g b b b 1. Location and Size Use the letters to label the heart image above a. Atria (2) e. Pulmonary Veins b. Ventricles (2) f. Aorta c. h. g. (AV) Valves (What are their names & how many flaps are in each one?) Pulmonary Bicuspid-2 Left / Tricuspid 3 flaps right Semilunar Valves- pulmonary leads to lungs/ aortic leads to aorta (main artery of the body). 5. Cardiac Circulation- blood flows from the atria to the ventricles. Valves do not allow backflow. B. Physiology of the Heart (pp. 368–374) 1. Intrinsic Conduction System of the Heart: Setting the Basic Rhythm a. Intrinsic Conduction System- Vena d. Trunk Sup. and Inf. Electrical impulses through nerve signals control heart rate. SA Node & AV node signal contraction in a healthy heart. ii. iii. impulses). Ischemia-Dead heart tissue usually resulting from a heart attack Fibrillation Heart rhythms become out of sync (Defibrillators are used to restart the heart 2. Cardiac Cycle and Heart Sounds- Lub Dub Noises are generated when blood exits the atria (Lub) and then passes through the through the semilunar valves AORTA- & PULMONARY (Dub). Murmurs-Additional sounds from the lub dub rhythm may indicate backflow from one of the AV valves that close improperly. Calculating Cardiac Output (CO) CO= HR (Heartrate)X SV (Amount of blood pumped through the heart in one time). a. Regulation of Stroke Volume (SV) AV and Semilunar Valves typically control stroke volume. b. Factors Modifying Basic Heart Rate (HR)-Stressful situations can lead to an increase in angiotension, vasoconstrictors, and other hormones that would speed up or slow down the heart rate to accommodate to one’s environment. II. BLOOD VESSELS (pp. 374–395) A. Microscopic Anatomy of Blood Vessels (pp. 374–377) 1. Tunics- Tunica Interna- Inner lining of vessel-very slick to reduce friction in bloodflow Tunica Media (composed of involuntary smooth muscle) Tunica Externa-Strong outer layer of vessels 2. Structural Differences between Arteries, Veins, and Capillaries More muscular in arteries for blood pumping Vessels are folded inward in veins preventing backflow ii. Left Common Carotid Artery iii. Left Subclavian Artery c. Arterial Branches of the Thoracic i. Intercostal Arteries ii. Bronchial Arteries iii. Esophageal Arteries iv. Phrenic Arteries d. Arterial Branches of the Abdominal Aorta B. Gross Anatomy of Blood Vessels (pp. 378– 386) (Key attached separately on webpage as an Adobe document) 1. Major Arteries of the Systemic Circulation (Figure 11.12) a. Arterial Branches of the Ascending i. Right and Left Coronary Arteries i. Celiac Trunk b. Arterial Branches of the Aortic Arch ii. Superior Mesenteric Artery i. Brachiocephalic Trunk iii. Renal Arteries Aorta Aorta iv. Gonadal Arteries vi. Inferior Mesenteric Artery v. Lumbar Arteries vii. Common Iliac Arteries 2. Major Veins of the Systemic Circulation (Figure 11.13) a. Veins Draining into the Superior Vena Cava i. Radial and Ulnar ii. Cephalic Vein iii. Common Iliac iv. Subclavian Vein v. Vertebral Vein vi. vii. Internal Jugular Brachiocephalic viii. Azygos Vein ix. Tibial & Fibular Veins x. Great Saphenous Veins xi. Gonadal Veins xii. Renal Veins xiii. Hepatic Portal xiv. Hepatic veins 3. Special Circulations (Figures 11.14–11.17) a. Arterial Supply of the Brain and the Circle of Willis (Pictured to the right; is responsible for circulating blood through the brain from the central nervous system to the peripheral nervous system). Fetal Circulation This process shuttles blood from the mother to the developing fetus with several important steps. The placenta (site of nourishment-similar to a yolk sac) will transfer blood flow to the baby’s developing liver. All oxygen poor blood will then travel to the baby’s heart through the DUCTUS VENOSUS and then pass through the heart. DUCTUS ARTERIOSUS delivers blood back to the fetus after maternal circulation. One important step in this process is that blood flow does not enter pulmonary circulation but rather bypasses it through the FORAMEN OVALE ( a hole between the two atria). This important step happens because the baby’s lungs are NOT fully functional and therefore they do not require pulmonary circulation. c. Hepatic Portal Circulation This process is important for digestion. It delivers necessary nutrients from digestive tract to the blood for circulation throughout the body. Hepatic refers to the liver (Hepatitis-Inflammation of the Liver)