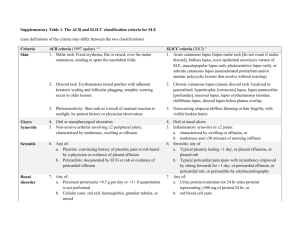
Data supplement 1
advertisement

Appendix Table 3. Questions for the literature search and results from the systematic review of the literature Q1. What are the indications and optimal timing for first renal biopsy in SLE patients and are they different compared to non-SLE patients? No. studies Design 1 References SCr ≥130 μmol/L associated with OR 2.1 for class IV LN 24 III 1-24 Abnormal urinalysis (proteinuria >0.5 g/24-hr and/or haematuria and/or cellular casts) with normal SCr is associated with class IIIIV LN Proteinuria >0.5 g/24-hr or haematuria or cellular casts: 70% class IIIIV LN at biopsy; isolated haematuria (>5 RBC/hpf) with proteinuria <0.5 g/24-hr: 22% active class III-IV LN at biopsy 26 III 1,3,6,7,9,11,13- Clinically ‘silent’ LN (proteinuria <0.3-0.5 g/24-hr, inactive urinary sediment, normal GFR) is associated with class I-II LN and a favorable outcome Prevalence of histologic class III-V LN: 86% in ‘overt’ versus 36% in ‘silent’ cases (defined as proteinuria <0.3 g/24-hr with inactive urinary sediment and GFR >70 ml/min//1.73m2) 10 III 36-45 Delay in kidney biopsy and diagnosis of LN is associated with progression of renal disease and histological lesions, reduced rates of renal remission after treatment, and increased risk for ESRD Delay >6 months is associated with adjusted HR 4.2–9.3 for ESRD 9 II 3,13,28,46-51 Item Example(s) of outcome or effect size Abnormal SCr (≥130 μmol/L [1.4 mg/dL]) and/or GFR levels (<80 ml/min/1.73m2) correlate with adverse histological forms of LN 20,23,25-35 Q2. Evaluation of the ISN/RPS 2003 classification system. What is the prognostic significance of renal biopsy findings? Item Example(s) of outcome or effect size No. studies Design References Improved inter-observer reproducibility with the ISN/RPS 2003 classification Kappa coefficient for inter-observer reproducibility is 0.53 versus 0.44 with the WHO classification; cases re-classified from WHO class III into ISN/RPS class IV had lower rates of response to therapy and increased risk for progression to ESRD 6 III 5,16,52-55 The histological class of nephritis (defined by the WHO or the ISN/RPS classification) correlates with patient and renal outcome (death, ESRD, doubling SCr, development of chronic renal insufficiency) Proliferative (class III-IV) versus non-proliferative LN is associated with RR 3.0 for death; class IV versus class III LN is associated with HR 4.3 for ESRD; class V LN has worse outcome than class I-II (abnormal renal function in 15% and ESRD in 5% during long-term follow-up); class V with superimposed proliferative lesions (class V+III-IV) has worse outcome than pure class V (ESRD rate 36% versus 12%) 52 II 1,3-6,11,14,16,28,47,48,56-96 ISN/RPS class IV-G versus IV-S is associated with more severe clinical disease and/or worse histological Increased endo-capillary hyper-cellularity, interstitial inflammation, activity lesions; no definitive difference in renal outcome 11 III 5,12,17,18,33,55,97-101 1 lesions 1,7,46,47,61,94,102-114 Prognostic significance of kidney deposits detected by immunofluorescence or electron microscopy Intensity/extension of deposits correlates with clinical & histological severity of renal disease, and renal outcome; intra-membranous electron-dense deposits are associated (RR 4.8) with death 19 II Prognostic significance of activity lesions on kidney biopsy (hypercellularity, leukocyte exudation, karyorrhexis/fibrinoid necrosis, cellular crescents, hyaline deposits, interstitial inflammation) The composite AI correlates with poor renal outcome (increased relapse rates, doubling SCr, ESRD, death; HR 1.4 per 1-unit); cellular crescents >30% of glomeruli is associated with RR 7.2 for doubling SCr; ≥25% interstitial infiltration is associated with HR 1.9 for doubling SCr or ESRD 44 II Prognostic significance of chronicity lesions on kidney biopsy (glomerular sclerosis, fibrous crescents, tubular atrophy, interstitial fibrosis) The composite CI correlates with poor response to immunosuppressive therapy, and poor long-term renal outcome (increased relapse rates, doubling SCr, ESRD, death; HR 1.18 per 1-unit for doubling Scr or death); glomerular sclerosis ≥25% glomeruli is associated (RR 3.3) with ESRD; interstitial fibrosis is associated (HR 2.0) with doubling SCr or ESRD; tubular atrophy ≥25% is associated (HR 2.4) with doubling SCr or ESRD 60 The composite tubulo-interstitial index (interstitial infiltrates + tubulorrhexis + interstitial sclerosis) is associated with higher proteinuria and SCr levels, and increased risk for ESRD (HR 72 in patients with class V LN) 15 Prognostic significance of renal vascular lesions (lupus vasculopathy, HUS/TTP/malignant hypertension-like lesions, vasculitis, arteriosclerosis) Association with higher SCr levels, increased rates of hypertension, lower 5- and 10-yr kidney survival rates (74% and 58% vs. 90% and 86% in patients without vascular lesions) 3 III 67,146,147 Additional prognostic value of renal histology to renal clinical disease severity The proportion of sclerosed glomeruli combined with SCr levels at 2 years post initiation of therapy may predict 59% of the variation in SCr levels at last follow-up in proliferative LN 4 II 23,46,47,70 Prognostic significance of tubulointerstitial lesions on kidney biopsy 1,7-9,11,13,15,25,46-48,5658,65,79,101-103,106,113,115-125 16,28,91,92,100,126-128, 50,94,110,111 II 1,3,8,10,11,13,17,23,25,28,47,48,5 6,57,61,63,65,73,75,76,79,81,84,8 7,90,92,100103,110,111,113,115,119-127,129145 II 79,15,46,47,58,79,101,102,106,115118 Q3. How well do biochemistry tests, serological tests, urinalysis, biomarkers correlate with renal biopsy findings in lupus nephritis? Item Example(s) of outcome or effect size Diagnostic value of SCr and/or GFR (estimated or measured) levels Higher SCr and/or lower GFR levels correlate with more advanced histological class (class IV>III>other; IV-G>IV-S), higher biopsy AI and CI (r = 0.27-0.46), tubulointerstitial lesions, kidney deposits, and presence of cellular crescents; in patients with SCr ≤1.4 mg/dL, those with MDRD-GFR below 60 ml/min/1.73m2 had more No. studies Design References 26 III 1-24,30,103 2 chronic lesions in renal biopsy Diagnostic value of hemoglobin levels Lower hemoglobin levels correlate with more advanced histological class (Hb <9 g/dL is associated with OR 3.2 for class IV LN) 6 III 6,7,14,17,18,33 Diagnostic value of serum complement levels Lower levels at the time of diagnosis correlate modestly with more advanced histology (proliferative < non-proliferative LN; class IV < III; IV-G < IV-S); correlation with karryorrhexis, endocapillary proliferation, and CI (r = -0.32 to 0.39); there is a single study reporting better predictive ability of serum C3 versus C4 13 III 2,4,14,18,23,30,148-154 Diagnostic value of serum anti-dsDNA antibodies Increased titers (ELISA, Crithidia, or Farr assay) at the time of diagnosis is associated with proliferative versus non-proliferative LN (OR 6.0), class IV > other; correlation with active / severe renal histology (biopsy AI, extra-capillary proliferation, karryorhexis, hyaline deposits, fibrinoid necrosis, electron-dense deposits; r coefficient ranging 0.35 to 0.81) 18 III 1,2,7,23,103,148-150,152-161 Diagnostic value of serum anti-C1q antibodies Increased titers (ELISA) are associated with active proliferative (class III-IV) LN (PPV 68%, NPV 98%); higher titers in class IV > other classes); correlation with biopsy AI and CI, glomerular infiltration, endo-capillary proliferation, fibrinoid necrosis, crescents (r coefficient ranging 0.32 to 0.56) 10 III 18,63,149,155,159,162-166 Diagnostic value of other serological tests (anti-chromatin, anti-histone, antinucleosome, anti-ribosomal P, anti-RNP, anti-Sm, ANCA, anti-endothelial cell antibodies) Limited diagnostic value; higher titers of anti-endothelial cell IgG in class IV vs. other classes of LN 19 III 17,18,149,151,156,159,160,167- Diagnostic value of proteinuria (24-hr urine collection or random spot urine protein to creatinine ratio) Higher proteinuria levels correlate with more advanced histological lesions (class IV-V > III > II; IV-G > IV-S), higher biopsy AI and CI, increased glomerular and tubulo-interstitial lesions; proteinuria >0.2 g/24-hr is associated (OR 4.4) with class IV LN; nephrotic-range proteinuria is common in class IV or V (± III-IV) LN 14 III 1,3,6,9,11,13-16,18,19,32-34 Diagnostic value of active urine sediment (haematuria >5 RBC/hpf and/or pyuria >5 WBC/hpf and/or cellular casts); see also Q1 More common in active class III-IV LN (OR 6.0), class IV-G versus IV-S, crescentic versus non-crescentic forms of LN; correlation with proteinuria levels and higher biopsy AI and CI; isolated abnormalities (in absence of proteinuria >0.5 g/24-hr) are less predictive for active class III-IV LN 11 III 1,7,9,11,15,17,19,23,29,33,35 Diagnostic value of serum biomarkers (ICAM-1, VCAM-1, fribrinolytic split products, IL-18, nitrate, IL-12p70, IFN-γ, IL-2-receptor, IFN-γ+/ΙL-4+ PBMCs [flow cytometry]) Limited diagnostic value 9 III 149,179-186 178 3 Diagnostic value of urine biomarkers (cytokines [IL-6, IL-12, IL-10, IL-2], TGFβ, ICAM-1, VCAM-1, T-bet, GATA-3, RANTES, MCP-1, proteomics) MCP-1 levels correlate with active class III-IV LN, biopsy AI and CI (n=4 studies); proteomic analysis demonstrates sensitivity 86-100% and specificity 50-100% for different histological classes of LN, and correlates with biopsy AI (r = 0.77) and CI (r = 0.87) 12 30,182,185,187-195 III Q4. What are the indications for initiating immunosuppressive therapy in lupus nephritis? Item Outcome and example(s) of effect size Class II LN Class III-IV LN Class V LN No. studies Design References Treatment with low-to-moderate doses of GC (0.25-0.5 mg/kg/day) if proteinuria exceeds 1 g/24-hr especially in presence of glomerular haematuria; immunosuppressive therapy (usually AZA; MPA and CY have also been used) is added in cases of inadequate response to GC (± HCQ), or when unable to taper their dose 6 V 59,196-200 Combination of immunosuppressive agents with GC are more effective than GC alone in prevention of ESRD or death; effect more pronounced in class IV versus III LN 4 I 201-204 13 II 57,139,205-215 9 III/IV 63,82,83,123,134,143,216,217 1 II 218 2 III 219,220 8 V 221-228 Combination of immunosuppressive agents with GC are indicated in cases with persistent proteinuria >1 g/24-hr despite optimal use of renin-angiotensin-aldosterone blockade; the use of adjunctive immunosuppression is independent predictor for remission of proteinuria in cases with nephrotic-range proteinuria Q5. What is the comparative evidence for the benefits and harms of therapeutic agents or interventions in patients with lupus nephritis and according to different histologic classes of kidney disease? Item Class II LN Outcome and example(s) of effect size Low-to-moderate doses of GC (0.25-0.5 mg/kg/day); immunosuppressive therapy can be added (usually AZA; also MPA, CY) if proteinuria exceeds 1 g/24-hr, especially in presence of glomerular haematuria Class III-IV LN: initial treatment Glucocorticoids GC-only regimens are less efficacious than the combination of GC and immunosuppressive agents in No. studies 6 Design V References 4 I 201-204 59,196-200 4 prevention of ESRD and/or death 14 II 57,139,205- III/IV 63,82,83,123,134, 215,229 9 143,216,217 Regimens used: high-dose GC (1 mg/kg/day ×4-6 wks, then tapered); or, pulses IV-MP (0.5-1 g ×3 days), followed by oral prednisone (0.5-0.7 mg/kg/day); both regimens have been used in RCTs ─ ─ ─ Benefit from the use of IV-MP pulses: may expedite the reduction of abnormal SCr and/or proteinuria levels; has been associated with improved renal outcome (increased remission rates, reduced relapse rates; extrapolation from two RCTs); has been used in severe crescentic LN 2 1 3 8 II III IV V 208,212 4 14 I II Cyclophosphamide Combination of CY (IV or oral) with GC is efficacious in stabilizing renal function (RR 0.63 for ESRD; RR 0.59 for doubling SCr); superiority over GC-only regimen becomes evident after 5 years of followup; long-term (≥10 years) follow-up data available 230 16,138,231 17,232-238 201-204 57,139,206212,214,215,229 9 III/IV 63,82,83,123,134, V 87,119,140,198,1 143,216,217 11 99,239-244 Benefit demonstrated in patients with high-risk features (high biopsy CI, impaired renal function, nephrotic syndrome, class V+IV LN, crescentic LN, rapidly progressive glomerulonephritis) 3 3 10 II III V 209,210,245 237,246,247 17,134,237,238,2 48-253 Comparable efficacy of IV-CY versus oral CY; in the long-term (7 years) follow-up of a RCT comparing immunosuppressive agents versus GC alone, only the IV-CY regimen was statistically superior in individual group comparisons; in the meta-analyses of early RCTs, results were more robust for the IV-CY regimen; a single RCT comparing intermittent IV-CY versus oral CY followed by AZA found no difference in efficacy or adverse events (trial prematurely terminated); trend for more adverse reactions (herpes zoster infections, leukopenia) with oral CY; oral CY has demonstrated efficacy in class IV LN with rapidly progressive renal failure 1 5 2 2 I II III IV Low-dose versus high-dose IV-CY. In White patients with moderate-risk features (class IV 70%; mean proteinuria 2.9-3.2 g/24-hr; mean biopsy CI 0.8-0.9), initial treatment with low-dose IV-CY (3g) has similar efficacy (prevention of ESRD; follow-up 10 years) and better toxicity profile (reduced infections) than high-dose IV-CY (NIH regimen; both regimens followed by AZA); in patients with high-risk features (class IV 85-90%; 35-50% Black; nephritic with GFR <80 ml/min or GFR >80 1 6 2 6 I II IV V 204 57,209-211,254 246,247 134,255 256 245,257-261 134,216 240,250,255,262264 5 ml/min with crescents >25%; mean proteinuria 5.0 g/24-hr; mean biopsy CI 3.7-4.4), extended course (30 months) of IV-CY was associated with lower rates of doubling SCr and of renal relapse compared to short course (6 months) IV-CY Toxicity of CY-based regimens: amenorrhea (dose- and age-dependent risk: in women aged ≥32 years D50 has been calculated to 8 g/m2), infections (particularly herpes zoster), leukopenia Azathioprine Early trials showed that the combination of AZA with GC is more efficacious than GC alone in preventing death (RR 0.6) but not ESRD In patients with class III-IV (±V) LN and moderate-risk features (70% Whites; mean SCr 109 μmol/L, mean proteinuria 3.2 g/24-hr, mean biopsy CI 2.3), the AZA/IV-MP/GC regimen had comparable rates of renal response with the IV-CY/GC regimen during the first 2 years (after a median follow-up of 6.3 years more than 80% of AZA-treated patients remained free of CY; after a median follow-up of 9.6 years there were no significant differences between the two regimens in terms of doubling SCr, ESRD, or mortality, although AZA-treated patients had HR 4.5 for renal relapse) Weak evidence-base for efficacy of AZA (prevention of ESRD) in severe forms of class III-IV LN Mycophenolic acid (mycophenolate mofetil, mycophenolate sodium) Comparable efficacy with CY regimens in terms of induction of renal remission (rates 56-81% in MPA, 52-76% in CY), prevention of ESRD and death; characteristics of patients included in the RCTs: most (53-67%) had class IV LN, relatively preserved renal function (mean SCr 1.1-1.3 mg/dL), average proteinuria 4.1-6.2 g/24-hr (except for two trials: 1.8-2.0 g/24-hr), chronic lesions in kidney biopsies (mean biopsy CI 2.8-3.9), heterogeneous ethnic background; MMF dose: 2-3 g/day A single RCT demonstrating superiority of MPA over CY included more Black patients, more patients with pure class V LN, and only 62% of patients in the CY arm received all 6 pulses of IV-CY Significant variation in renal response rates according to race (lower response rates of IV-CY in Black/Hispanics) and region (better efficacy of MPA in regions outside Asia) More favorable toxicity profile of MPA versus CY (reduced amenorrhea, leukopenia, alopecia rates; trend for lower rates of infections; increased gastrointestinal events [diarrhea] with MPA versus CY) Open-label studies have also demonstrated efficacy and histological improvement with MPA in class III-IV LN Efficacy of enteric-coated mycophenolate sodium (1440-2160 mg/day) in class III-IV LN Crescentic LN with impaired renal function: comparable efficacy of MPA versus CY (higher response rates but also more relapses with MPA) 3 IV 3 14 I II 265-267 201-204 23,139,205,206,2 09,210,213,230,2 68-273 3 9 III V 274-276 50,119,197,277282 8 7 I II 1 8 III V 256,283-289 290-296 297 49,88,199,298302 1 1 2 II III V 1 1 1 II III V 303 304 305,306 307 308 237 6 Ciclosporin A A single RCT comparing oral CsA versus IV-CY (both in combination with GC) in patients with moderate-risk features (class IV 53-67%; SCr <140 μmol/L; mean proteinuria 2.5-3.8 g/24-hr; mean biopsy CI 3.5-4.0) found comparable rates of renal response (at 9 months) and improvements in renal disease parameters (reduction in proteinuria) Toxicity: hypertension (very common); hirsuitism, dose adjustments may be needed due to SCr elevations Tacrolimus Comparable short-term efficacy of tacrolimus versus pulses IV-CY (both in combination with GC) in class III-IV LN with moderate-risk features (class IV 72%; normal SCr levels; mean proteinuria 2.2-3.0 g/24-hr; mean biopsy CI 1.0-1.2). In patients with mixed class V+IV LN (normal SCr levels; mean proteinuria 4.1-4.4 g/24-hr, mean biopsy CI 1.3-1.4; 65% had been previously treated with MPA or CY), combination therapy with tacrolimus/MMF/prednisone was associated with higher rates of complete response at 6 months compared to pulse IV-CY therapy (50% versus 5%) Plasma exchange No benefit of adding plasma exchange cycles to immunosuppressive therapy (AZA, IV-CY) in terms of renal remission or death rates (evidence from RCTs that included patients with class IV 40-100%; mean proteinuria 5.5-8.6 g/24-hr, impaired renal function) Plasma exchange / immunoadsorption cycles in combination with GC and/or cytotoxic therapy have been used in cases with rapidly progressive glomerulonephritis or crescentic class IV LN Leflunomide Single non-randomized study in mild class III-IV LN has shown comparable efficacy with low-dose pulse IV-CY; increased biopsy CI at follow-up renal biopsy Chlorambucil Oral chlorambucil in combination with GC has shown comparable efficacy with the combination of oral CY with GC in prevention of renal or patient death (active class III-IV ± V cases; histological improvements at follow-up renal biopsy) Rituximab Combination therapy with rituximab/MMF/GC was no superior than MMF/GC in terms of renal response rates (57% versus 46% at 1 year); n=8 placebo patients versus no rituximab-treated patients required CY rescue therapy (cases with moderate-risk features: White 31%; class IV 66%; mean SCr 309 1 3 II V 3 6 II V 1 3 1 2 2 I II III IV V 1 1 1 II III V 330 1 1 III V 274 2 II 334,335 310-312 129,313,314 315-320 202,203 321-324 325 326,327 328,329 331 332 333 7 Class III-IV LN: subsequent treatment 1.0 mg/dL; mean proteinuria 4.0 g/24-hr) Efficacious in small case-series of active class III-IV LN (used as first-line treatment) 3 V 336-338 Belimumab Post-hoc analysis of RCT: reduced rates of renal flares in the high-dose drug arm versus placebo 1 III 339 4 IV 134,199,340,341 15 II In class III-IV LN patients responding to initial immunosuppressive therapy (‘induction therapy’), absence or shorter duration of subsequent immunosuppressive therapy (‘maintenance therapy’) is associated with increased risk for renal relapse Cyclophosphamide Lower dose and/or less frequently administered intermittent IV-CY (quarterly pulses) or oral CY, sequentially administered after remission induction for another 12-24 months is associated with lower rates of renal relapse, doubling SCr or ESRD; experience in patients with high-risk features (nephrotic syndrome and/or impaired renal function) with remission rates up to 72% 57,139,206,208212,229,245,260, 272,309,342,343 2 2 10 III IV V 246,297 134,216 87,136,198,239,2 40,243,252,263,2 64,341 Azathioprine Used for maintenance of renal remission following successful initial treatment with CY (evidence from RCTs and uncontrolled case series); also, sequentially after initial treatment with AZA (in milder LN cases) A single retrospective controlled study in class IV LN (mean proteinuria 5.9-6.8 g/24-hr, mean SCr 122-135 μmol/L) comparing pulse IV-CY versus oral CY followed by AZA found no difference in renal relapse or doubling SCr rates 11 II 23,140,209,210,2 57259,261,272,273, 290,343 2 3 13 III IV V 247,274 133,134,217 50,140,197,242,2 44,249,250,263,2 64,278,280,281,3 05 Mycophenolic acid Used after initial treatment with CY or MPA (sequential therapy) RCT comparing quarterly pulses IV-CY (0.5-1 g/m2) versus MMF (0.5-3 g/day) versus AZA (1-3 mg/kg/day) after initial treatment with pulse IV-CY in patients with high-risk features (Hispanics 50%; class IV 68-85%; mean SCr 1.5-1.7 mg/dL; mean proteinuria 4.7-5.7 g/24-hr; mean biopsy CI 1.9-3.8): during follow-up (mean 5.5 years) there were reduced renal and patient survival rates and more relapses in the IV-CY group (40% versus 32% in AZA, 15% in MMF) 2 4 2 12 I II IV V 256,288 140,343-345 242,346 49,88,199,241,25 1,264,299301,305,347 8 ALMS trial (42% Whites, class IV ± V 72%, composite endpoint, responders after initial treatment with either IV-CY or MMF were re-randomized to study arms): reduced renal flares with MMF versus AZA (13% versus 23% during 3-year period); MAINTAIN trial (79% Whites, class IV 59%, time to flare used as endpoint, randomization upon enrollment regardless of response to initial low-dose IV-CY regimen): comparable rates of renal flares with MMF versus AZA (19% versus 25% during 3-year period) Ciclosporin A Used after initial treatment with CY or CsA (sequential therapy); efficacious in class III-IV LN with preserved renal function and moderate-risk features 2 1 II V 309,348 Tacrolimus Limited experience with prolonged (sequential) treatment of class III-IV LN 2 V 315,318 1 II 349 1 1 II III 350 5 4 II IV 126,212,343-345 2 2 6 II III V 212,245 Intravenous Ig (IVIG) Has been used after good response to initial treatment with IV-CY, with comparable efficacy with extended pulse IV-CY treatment (LN cases with moderate-risk features: White patients, class IV 2023%; single study) Plasma exchange / immunoadsorption Weak evidence-base; benefit has been demonstrated for prolonged versus short duration treatment cycles Class III-IV LN: relapsing or refractory disease Duration of subsequent immunosuppressive therapy: at least three years (by extrapolating from RCTs and retrospective cohort data); in class II-IV LN cases treated with MMF, tapering of MMF dose <2 g/day before 18 months after renal remission has been associated with increased risk (HR 6.3-6.8) for relapse 312 327 134,199,340,341 Heterogeneity in the clinical characteristics of the studied patients, the number, type, dosages and duration of prior therapies; most studies have included patients who either flared or did not respond (refractory) to immunosuppressive treatment Re-introduction or extended treatment with immunosuppressive agent CY. Evidence extrapolated from the long-term follow-up of RCTs; in patients who failed or relapsed after initial treatment with 6 monthly pulses IV-CY, extended treatment with IV-CY (0.5-1 g/m2 ×6 monthly pulses) had comparable efficacy with enteric coated MPS in terms of renal remission (34% versus 57%), prevention of ESRD, improvement in renal parameters (less adverse effects in the MPS group) 126,304 87,130,140,198,2 49,263 9 Switch to or add another immunosuppressive agent CY. Non-responders to MPA may respond to CY (but not to AZA) 2 V 298 MPA has demonstrated efficacy in class III-IV LN patients who relapsed or were refractory to CY or AZA (mean proteinuria ranging 3.3 to 5.5 g/24-hr; complete and partial renal response rates 50-60%) 5 V 351-355 CsA in combination with moderate doses of GC (prednisone 0.5 mg/kg/day) is efficacious in class IIIIV LN cases with incomplete response or proteinuric relapse while on immunosuppressive treatment with CY or AZA (response rates 50-60%; stabilization of SCr levels); maintenance CsA therapy is needed to prevent relapses; histological improvements have been shown in follow-up renal biopsies (class down-transformation, reduced biopsy AI) 5 V 310,312,356-358 Tacrolimus in combination with GC is efficacious in refractory class III-IV LN or in cases with persistent proteinuria despite immunosuppressive treatment with MMF or CY: reduction in proteinuria, stabilization of SCr levels, steroid-sparring effect; has been used as add-on therapy to MMF in cases with incomplete or no response or flare (renal response rates up to 70% after an average 11 months therapy; increased risk for infections and neurotoxicity) 6 V 315,317,318,359- IVIG. Rapid (within 1 month) anti-proteinuric effect in severe LN cases (nephrotic syndrome, impaired renal function) refractory to immunosuppressive treatment (CY); paucity of long-term data 2 V 362,363 3 V 364-366 18 V 336-338,349,367- Plasma exchange – Immunoadsorption Plasma exchange or immunoadsorption sessions added to standard immunosuppressive therapy in refractory cases with nephrotic syndrome and impaired renal function: anti-proteinuric effect and stable or improved renal function Rituximab (anti-CD20 mAb) Regimen: IV RTX (375 mg/m2 on days 1,9,16,23 or 1000 mg ×2 times 3 weeks apart) + IV-MP 250 mg + IV-CY 0.5 g/m2 (on days 1, 23); concomitant immunosuppressive treatment can be continued Efficacious in refractory or relapsing class III-IV cases (majority previously treated with CY; mean proteinuria 4.3 g/24-hr; mean serum albumin 2.4 g/dL; mean GFR 80 ml/min; mean biopsy AI 8, CI 3) with renal response rates 60% (class III), 39% (class IV), 26% (mixed V+III-IV); steroid-sparring effect; mostly used in White patients but also efficacious in case series with Black/Asian patients Predictors for poor response: baseline GFR <30 ml/min; rapidly progressive glomerulonephritis; nephrotic syndrome; Black race; no B-cell depletion after 1 month Relapses are common (27% after mean 12 months); 80% are successfully re-treated with RTX Well tolerated; mild infections 361 380 10 Other options Stem cell transplantation Immunoablative IV-CY Leflunomide Total lymphoid irradiation Pentoxifylline Infliximab Class V LN: initial treatment 7 1 1 4 1 1 V V V V V V 381-387 1 1 II III 218 1 III 219 1 2 III V 2 2 2 II III V 218,396 1 1 6 II III V 396 388 389 390-393 394 395 (evidence-base for adjunctive therapy is presented in Q7) Glucocorticoids GC-alone is less efficacious than the combination of GC with immunosuppressive agents in class V LN with high-risk features (non-White race 80%; mean proteinuria 5.7 g/24-hr) Comparable efficacy of GC versus GC in combination with immunosuppressive agents administered for 6 months in class V LN with moderate-risk features (Whites 72%; mean eGFR 77 ml/min; mean UP 3.1 g/24-hr) Chlorambucil Oral chlorambucil (0.2 mg/kg) alternating monthly with IV-MP is more efficacious (higher renal response rate; fewer relapses) than GC alone (WHO class Va/b/c; preserved renal function at baseline; mean SCr 1.6 mg/dL at last follow-up) Azathioprine Prolonged (for at least 1 year) treatment with AZA in combination with GC is efficacious in class V LN with moderate-risk features (mean proteinuria 3.9 g/24-hr; mean GFR 80 ml/min) Cyclophosphamide The combination of GC with IV-CY (0.5-1 g/m2 bimonthly ×6 pulses) is more efficacious than GC alone (complete response rates at 1 year 40% versus 13%), and is associated with fewer relapses than the combination of GC with CsA (baseline clinical characteristics: 71% non-White; GFR 80-89 ml/min; proteinuria 5.0-5.8 g/24-hr); oral CY regimen also efficacious Mycophenolic acid In a pooled analysis of two RCTs comparing MMF (2-3 g/day) versus IV-CY (pulses 0.5-1 g/m2), both in combination with GC, the two groups had comparable improvements in proteinuria at 24 wks; there was no difference within the subset of nephrotic patients (clinical characteristics of patients: 30% Blacks; mean proteinuria 5.0-5.8 g/24-hr; mean SCr 61-72 μmol/L); leukopenia and alopecia were more common with IV-CY 220 220 221,223 220,297 198,222 297 224,225,298,347, 397,398 11 Ciclosporin A The combination of GC with IV-CY (0.5-1 g/m2 bimonthly ×6 pulses) is more efficacious than GC alone (complete response rates at 1 year 40% versus 13%), and is associated with fewer relapses than the combination of GC with CsA (baseline clinical characteristics: 71% non-White; GFR 80-89 ml/min; proteinuria 5.0-5.8 g/24-hr) Efficacious in nephrotic patients with preserved renal function; dose adjustments may be needed based on SCr levels; toxicity: hypertension, metabolic adverse effects 1 II 218 3 V 226-228 1 1 III V 399 Rituximab Efficacious in small case series in class V LN (used as first-line treatment) 3 V 336-338 Low-dose GC 1 III 219 Pulses IV-CY (quarterly) in combination with low-dose GC 1 III 297 MPA (sequential therapy) in combination with low-dose GC 1 7 III V Tacrolimus Efficacious in nephrotic patients with preserved renal function Class V LN: subsequent treatment 319 297 224,225,242,298, 347,397,398 Class V LN: relapsing or refractory disease AZA in combination with low-dose GC (after initial treatment with CY) 3 V 222,223,242 CsA (sequential therapy) in combination with low-dose GC 2 V 226,227 Pulses IV-CY (after failure/relapse to glucocorticoids or CsA, AZA, MPA) 2 V 221,298 MPA (after failure or relapse to AZA, CY) CsA Tacrolimus RTX (± other concomitant immunosuppressive agent) 3 7 1 13 V V V V 221,397,400 221,353-358 221 336338,367,368,372, 12 374-380 IVIG (severe nephrotic cases with impaired renal function) Plasma exchange / immunoadsorption (severe nephrotic cases with impaired renal function) Leflunomide Other options (immunoablative dose of IV-CY; mesenchymal stem cell transplantation) 2 3 1 3 V V V V 362,363 364-366 389 383,386,388 Q6. What are the best validated definitions of therapeutic goals in lupus nephritis? Item Outcome and example(s) of effect size Renal response Renal flare No. studies Design References Failure to achieve complete renal response/remission is associated with poor long-term renal outcome (most patients with class IV LN) Heterogeneity in definitions of renal response; usually it includes normal (or improved) SCr / GFR, proteinuria below 0.3 to 1 g/24-hr, and inactive urinary sediment; lack of complete response after immunosuppressive treatment is associated with increased risk (HR 4.5 – 9.9) for ESRD 16 III 73,77,123,126,129,1 Complete response of the nephrotic syndrome (class V LN; usually defined as proteinuria below 0.250.4 g/24-hr with normal GFR, inactive urinary sediment, and normal serum albumin) is associated with favourable long-term outcome (lack of complete response is associated with HR 9.3 for ESRD) 1 III 56 1 IV 117 Patients who achieve partial renal response (usually defined as reduction in proteinuria by ≥50% but not reaching the complete response thresholds plus no deterioration in renal function) have worse prognosis than those who achieve complete complete response (RR 5.2 for doubling SCr or ESRD) 5 III 126,129,140,141,40 1 IV 405 Flares ( ‘proteinuric’ or ‘nephritic’) are associated with adverse renal outcome (both in class III-IV and class V LN) Severe nephritic flares accompanied by deterioration of renal function demonstrate the strongest association with adverse renal outcome (LR 11.8 for ESRD) Proteinuric flares also associated with worse renal outcome (increase in proteinuria by ≥2 g/24-hr or doubling if initial proteinuria was >3.5 g/24-hr is associated with OR 9.3 for doubling SCr) 8 III 73,126,133,221,403, 33,134,140,141,258, 401-403 10 IV 17,58,59,78,135,136 ,196,404-406 1 407-409 7 IV 17,117,124,135,136 13 Q7. What is the evidence for the benefits and harms of adjunct therapies in lupus nephritis? Item Outcome and example(s) of effect size No. studies Design References ACE-inhibitors (ACEi) / angiotensin receptor blockers (ARBs) Class II LN: use of ACEi (in addition to steroids) is associated with increased rates of renal response 1 IV 196 Class III–V LN: in stable renal disease with persistent proteinuria >1 g/24-hr despite steroids and immunosuppressive therapy, addition of ACEi/ARB results in reduction of proteinuria and blood pressure levels 5 II 88,218,410-412 In SLE patients with no renal involvement, use of ACEi has been associated with reduced risk (HR 0.31) for renal disease 1 III 413 Use of HCQ is associated with higher rates of renal remission, fewer renal relapses during maintenance therapy, lower risk for major renal flare (HR 0.26), and lower accrual of renal damage (HR 0.19) 8 II 49,80,298,406,414- Omega-3 fatty acid Lipid-lowering effect; no significant impact on renal function 4 Lipid-lowering therapies [See Q10] Hydroxychloroquine 417 418-421 II Q8. How do blood tests, serological tests, urinalysis/proteinuria, biomarkers, kidney histology (repeat biopsy) compare with regard to their ability to monitor lupus nephritis? Item Outcome and example(s) of effect size No. studies Design References Reproducible increases in SCr levels (≥20-30% above baseline value) and/or reduction in GFR (≥10% from baseline) Included in the definitions of active or flare of LN; specificity >80% but low sensitivity for proteinuric renal activity; 24-hr creatinine clearance is considered the ‘gold standard’ in assessing renal function (not validated in LN; single study showing unpredictable variability in serial measurements); The Cockcroft-Gault equation tends to overestimate, the MDRD equation tends to underestimate GFR; in Caucasians the accuracy for classifying patients with GFR 60-89 ml/min/1.73m2 was 82% with the Cockcroft-Gault vs. 59% with the MDRD equation 6 II 422-427 Monitoring ability of other blood tests (hemoglobin, serum albumin) Improvements during inactive versus active LN 3 II Monitoring ability of serum antidsDNA antibodies Increased titers during active/flare state versus lower titers during inactive/remission of LN; most useful in class III-V LN (lower predictive value for proteinuric flares of class V LN); have been evaluated in the context of RCTs (reductions correlating with response to therapy); sensitivity 46-89% (typically ~70%), specificity 52-98%, PPV 11- 48 II 163,212,428 ; data also from RCTs 69,129,130,149,150,152,158160,162,164,212,359,422,429-462 14 52%, high NPV (typically 86-90%); the Farr method has been most extensively studied, yielding higher sensitivity/specificity rates than ELISA Rise in titers ≥25% (within 6 months prior to flare) are 65-91% sensitive for impending renal flare (poor specificity as it may also antedate non-renal SLE flare) 6 II 130,162,434,449,455,459 Reduced levels during active/flare state versus normal titers during inactive/remission of LN; serial measurements are useful to identify active proliferative renal disease (insensitive for proteinuric flares of class V LN); studied in the context of RCTs (normalization correlating with response to therapy); low C3 (e.g. ≤ 81) has sensitivity 72-85%, specificity 51-93% (typically 70%), PPV 22-28%, and NPV 93-97% for active renal disease; low C4 (e.g. ≤ 11) has sensitivity 28-74%, specificity 50-71%, PPV 1731%, NPV 92-95%; two studies have reported superior performance of C3 versus C4, whereas data from a single RCT show that increases in C4 (not in C3) correlate with induction of LN remission 25 II 129,130,149,150,163,212,409,422,440,4 Persistently low levels (within 3-6 months prior to flare) are 75-90% sensitive for future renal flare 4 II 130,459,463,467 Increased titres are found at active versus inactive stage of proliferative LN; sensitivity 74-88%, specificity 70-92%, PPV 37-68%, NPV 91-100%; outperforms serum antidsDNA and C3/C4 (including in detecting class V proteinuric flares); combination with anti-dsDNA (Farr) further enhances sensitivity (91%) and specificity (100%) for active nephritis; have been validated against biopsy-proven active proliferative LN (PPV 68%, NPV 98%); less well studied than other serological markers in prospective controlled trials 26 II 130,149,152,159,162- Appearance or increase in titres ≥50% (within 6 months prior to flare) have sensitivity 71-76%, specificity 84-92%, PPV 50-56%, NPV 70-97% for future renal flare 3 II 162,164,455 Monitoring ability of serum antinucleosome antibodies Increased titres are found at active stage of proliferative LN; sensitivity (32-89%), specificity (22-67%), PPV (16-40%), NPV (77-88%) 9 II 158,431,432,436,439,449,454,483,484 Monitoring ability of other serological tests (anti-chromatin, anti-histone, anti-ribosomal P, antiCRP, anti-heparan sulfate, anti-αactinin, anti-endothelial cell antibodies) Changes in titres correlate with LN activity; less extensively studied or validated 19 II Monitoring ability of urine sediment ‘Active sediment’ ([re-]appearance of haematuria, pyuria, casts) included in definition of active LN; also in the context of therapeutic (controlled) trials to define remission and flare of LN; cellular casts have sensitivity 81% for flares (defined according to increases in SCr and/or proteinuria; 96% for flares with proteinuria >1 g/24-hr), and may precede Monitoring ability of serum complement (C3, C4) Monitoring ability of serum antiC1q antibodies 42,443,450,452,458,459,463-472 164,166,431,435,439441,453,455,457,473-482 130,149,151,159,160,176178,436,437,448,451,456,460,484-488 7 II 129,422,444,448,473,489,490 15 other flare signs by 10-13 weeks; haematuria (>5 RBC/hpf) has sensitivity 42% and specificity 84% for active versus inactive LN; urine cytology (lymphoblasts, plasma cells, monocytes) abnormal during renal flare Monitoring ability of proteinuria II 23,129,422,443,444,448,464,465,473,49 Should be quantified as part of monitoring lupus renal disease; urine dipstick has suboptimal performance in detecting/excluding significant proteinuria (62-86% specificity to correctly exclude proteinuria ≥0.5 g/24-hr); spot urine measurements of urine protein to creatinine ratio show very good correlation with ratios determined by 24-hr urine collection over the entire range of proteinuria (r = 0.81-0.91) but poor concordance over the range of 0.5-3.0 (r = 0.48); first morning void urine sample performs better than random spot urine sample 22 Monitoring ability of serum biomarkers (ICAM-1, VCAM-1, MCP-1, IL-2-receptor, IL-17, CXCL13, β2-microglobulin, nitrate, MMP-3, flow cytometry for various subsets of peripheral blood mononuclear cells) Limited diagnostic value 17 III 149,160,179,183,186,461,503-513 Monitoring ability of urine biomarkers (cytokines, lipocalin-2, slit diaphragm proteins, FoxP3, ICAM-1, VCAM-1, TGFβ, OPG, MCP-1, TWEAK, NGAL, proteomics) MCP-1 mRNA correlates with proteinuria, haematuria, renal SLEDAI (levels >7.5 has PPV 98% and NPV 100% for renal SLEDAI >3); TWEAK mRNA shows modest correlation with renal SLEDAI (r = 0.39-0.41; values >9.1 has PPV 93% and NPV 67% for active nephritis); NGAL (ELISA) >13.6 ng/mL has 89% sensitivity and 72% specificity for biopsy-proven active LN; Proteomics: hepcidin-20/25 (changes in levels 4 months before and at the time of renal flare) 22 III 30,187,188,190,192,193,422,438,443,44 Monitoring ability of repeat kidney biopsy In patients with proliferative LN who have responded to immunosuppressive treatment repeat biopsy shows histological class down-transformation (from III-IV to II / V), reduced AI (stable / mildly increased CI), improved immunofluorescence findings, reduced deposits; in treatment failure or severe flare there is often transformation from class II-III to class IV and from class V to mixed V+III-IV (no change in histological class in patients with class IV at initial biopsy), increased CI, scarring, glomerular sclerosis, and deposits; repeat biopsy can assist therapeutic decisions in patients with persistent non-nephrotic proteinuria (despite improved renal function) or with worsening of renal function 27 1-502 4,465,490,500,514-522 II 7,10,23,59,61,66,72,88,90,107,115,117, 118,129,196,211,255,312,403,523-530 Q9. What is the prognostic performance of biochemistry tests, serological tests, urinalysis, and biomarkers in lupus nephritis? Item Example(s) of outcome or effect size No. Design References 16 studies Prognostic value of SCr and/or GFR levels II 3,4,13,19,22-24,46- Higher baseline (and follow-up) SCr correlates with higher follow-up SCr values, higher rates of doubling of SCr or ESRD (HR 1.26 per 1-mg/dL), lower odds for response to immunosuppressive treatment, and increased risk for death (HR 5.9); reduction of initially abnormal SCr at 6 months after treatment has OR 14.9 for good long-term renal outcome; in the ALMS trial patients with baseline GFR <30 ml/min/1.73m2 had OR 0.2 for response to therapy at 24 wks 65 Prognostic value of haemoglobin (haematocrit) levels Haematocrit <26-36% or haemoglobin <11 g/dL at LN onset is associated with increased rates of chronic renal failure, doubling SCr or ESRD (OR 0.6 for renal survival per 1-g/dL decrement); persistent anaemia (haematocrit <33%) at the time of response is associated with LR 4.6 for ESRD 14 Prognostic value of platelet count Lower numbers correlate with increased rates of deterioration of renal function (thrombocytopenia <20,000/μL is associated with HR 14.2 for ESRD) 3 II 47,91,531 Prognostic value of serum albumin levels Lower values associated with adverse renal outcome in class III-V LN (HR 0.9 per 1-g/dL increment for doubling SCr/ESRD; persistently levels <3.5 g/dL after immunosuppressive therapy is associated with RR 3.3 for doubling SCr) 10 II 47,115,133,134,144,258,290,359,539, Prognostic value of serum lipids High serum total cholesterol levels correlates with ESRD (HR 1.02) and death (HR 1.20); persistent dyslipidaemia after treatment of class III-IV LN is associated with future decline in GFR 4 II 69,401,538,539 Prognostic value of serum anti-dsDNA antibodies Persistently high titres despite treatment is associated with increased risk for renal flare (RR 2.3 in class IV LN; LR 4.9 in complete responders); most associations are with anti-dsDNA measured by the Farr method 15 II 1,46,126,133,261,525,544-551 Prognostic value of serum C3 levels Low C3 (<76 mg/dL) levels is associated with lower rates of complete remission, persistent proteinuria (>1 g/24-hr), increased rates of chronic renal failure and ESRD; persistently low C3 after immunosuppressive treatment is associated with renal flares (RR 2.2) and adverse outcome (HR 2.3 for doubling SCr or ESRD or death) 15 II 19,46,103,120,121,130,133,134,464,4 Prognostic value of serum C4 levels Low C4 (<10-11 mg/dL) levels at baseline is associated with increased risk for future relapses, deterioration of renal function; low C4 at the time of response to treatment has LR 14.2 for future renal flare (follow-up of RCTs) 8 II 19,73,126,255,409,464,548,554 Prognostic value of other serological tests (antiribosomal P, anti-nucleosome, anti-Sm, anti-C1q, ANCA, anti-endothelial cell antibodies) Limited prognostic value 15 II 63,73,78,151,168,173,534,544,546,54 48,57,58,60,65,68,71-73,7679,83,84,86,88,91,101,105,115117,120-124,126,127,134136,140,141,143,145,255,258,401,40 2,404,405,464,500,531-541 II 65,68,115,120,121,126,135,136,452,5 31,532,542,543 542 68,525,547,548,552,553 9,551,555-557 17 Prognostic value of urine sediment (haematuria , pyuria, cellular casts) Active urine sediment at the time of diagnosis is associated with worse renal outcome (HR 2.6 for SCr >130 μmol/L at last follow-up visit; RR 4.0 for patient death); disappearance of sediment abnormalities following therapy is associated with favourable long-term patient prognosis 5 III 1,28,69,76,539 Prognostic value of proteinuria level Nephrotic-range proteinuria at LN onset is associated with increased risk for ESRD (OR 6.5) or death (HR 4.0); associations confirmed in both proliferative and membranous LN; there is a dose effect (in LN cases with normal GFR and proteinuria in the range of 0.25-3.5 g/24-hr, baseline proteinuria >0.5 g/24-hr [vs. <0.5 g/24-hr] is associated with HR 2.3 for future decline in GFR); persistent proteinuria >0.5 g/24-hr despite immunosuppressive treatment is associated with future deterioration of renal function (HR 2.4 for doubling SCr; LR 5.9 for ESRD); reduction in proteinuria to less than 1 g/24-hr at 6 months after treatment has PPV 87% for good long-term renal outcome 37 II 16,23,46,47,56,60,68,73,77,82,87,115 Hypertension (at baseline and/or persistent following treatment) is associated with doubling SCr (RR 6.7) and development of ESRD (HR 5.0) 27 Hypertension ,117,126,127,130,133,134,218,221,25 7,258,359,401,404,405,464,537542,554,558-560 19,47,48,58,60,65,68,69,72,77,79,83, II 86,123,130,133-136,532,539,561-566 Q10. Are effective management options for chronic kidney disease and end-stage renal disease (including renal replacement therapies) different in SLE compared to nonSLE patients? Item Outcome and example(s) of effect size No. studies Design References Dialysis in SLE patients: outcome and predictors SLE patients on HD are at increased risk for death (HR 1.17) and thrombotic microangiopathy (OR 3.7); majority of deaths are due to infections and cardiovascular disease events; high disease activity and need for immunosuppressives are predictors of adverse outcome (OR 7.3 for death); PD: increased rates of infections / peritonitis / hospitalizations due to infections (OR 6.0 versus non-diabetic controls), need for higher doses of erythropoietin to maintain similar haemoglobin levels; HD: increased rates of vascular access thrombosis (OR 3.1; risk factors are female gender, Black race, arterio-venous graft versus fistula, aPL positivity) 21 III 86,567-586 Renal activity during dialysis in SLE Often (>50%) there is clinical and to lesser extent, serological remission 16 III 570,571,577,579,580,583,587-596 Renal transplantation in SLE: outcome Overall comparable renal graft and patient outcomes with other disease controls (data from single centres); increased risk for allograft loss (HR 1.09) and death (HR 1.18 versus diabetes controls) (data from registries); Renal transplantation in SLE: predictors of Stronger evidence for recipient age, recurrent LN (HR 4.1), graft rejection (HR 2.7), ethnicity of the recipient (Black ethnicity has HR 1.6-1.7), living vs. cadaveric donor (HR 0.64), HLA mismatch (HR 1.8), delayed graft function (HR 1.7), previous renal transplantation (HR 2.3), aPL positivity; less strong evidence for 25 III 589,597-620 18 allograft loss recipient gender, recipient body mass index, panel-reactive antibodies, smoking, donor ethnicity, donor age, pregnancy history, pre-transplantation dialysis mode Post-renal transplantation immunosuppressive therapy Similar regimens with those used in non-SLE patients; calcineurin inhibitor-based triple immunosuppression is associated with improved outcomes 13 Recurrent lupus nephritis after renal transplantation Wide range of reported frequencies (from 1.9% to 30-39% in studies performing protocol kidney biopsies; typically 4.5%) 18 IV 589,590,605-609,612-615,624-630 Renal transplantation in SLE: adjunct therapy Lipid-lowering therapy. Fluvastatin (40-80 mg/day) in patients with dyslipidaemia resulted in reductions in serum LDL-cholesterol by 29% and in major cardiac events by 73% (p=0.064; follow-up 7.3 years) 1 II 631 III 589,598,602,603,608,611,615,621626 Q11. What are the prognostic and therapeutic implications of the presence of anti-phospholipid antibody serology / anti-phospholipid syndrome or histological lesions of anti-phospholipid syndrome-associated nephropathy (APSN) in patients with lupus nephritis? Item Outcome and example(s) of effect size No. studies Design References Prognostic significance of aPL antibodies in renal outcome in SLE No significant association with renal outcome (single study reporting association with chronic renal insufficiency) 8 III 632-640 Prevalence of APSN in SLE Prevalence of thrombotic microangiopathy: 6-46%; full-spectrum (thrombotic microangiopathy and chronic vascular lesions) of APSN lesions: 11-43% 6 IV 641-646 Association of aPL with APSN APSN lesions are more frequent in aPL positive (lupus anticoagulant is associated with OR 11.5, anticardiolipin antibodies are associated with OR 5.7) and in APS patients (ca. 66% versus 20-30% in SLE/aPL/non-APS patients) 18 III Association of APSN lesions with hypertension, higher SCr / lower GFR (OR 5.8) and proteinuria levels, and increased interstitial fibrosis at renal biopsy); no association with rates of renal remission, doubling SCr, or ESRD (follow-up 2-10 years) 9 Impact of APSN on renal outcome in SLE 632634,638,641,642,644655 III 633,641-648 Q12. What is the optimal management of lupus nephritis in stable pregnant patients and in case of flare during pregnancy? 19 Item Outcome and example(s) of effect size No. studies Design References Risk factors for adverse pregnancy outcomes in LN Risk factors are: a) high renal disease activity or renal flare at the time of conception (risk for miscarriage, stillbirth, pre-term delivery, IUGR, hypertension; first trimester proteinuria >0.5 g/24-hr has OR 4.1 for miscarriage; LN at remission for at least 6 months prior to and at pregnancy onset is associated with increased live birth rate [88% versus 64%]); b) high extra-renal SLE activity; c) thrombocytopenia (miscarriage, stillbirth; first trimester platelet count below 150,000/μL is associated with RR 3.3); d) hypertension (miscarriage, stillbirth, preterm delivery, IUGR); e) low serum C3/C4 (miscarriage, stillbirth, IUGR, neonatal death); f) anti-dsDNA (fetal loss); g) anti-SSA/Ro (pre-term delivery; CHB); h) anti-SSB/La (OR 11.5 for IUGR); i) aPL antibodies (miscarriage, stillbirth, preterm delivery, maternal hypertension, pre-eclampsia); j) hypo-albuminaemia (foetal loss [OR 19.1], IUGR [OR 7.0]); k) GC ≥10 mg/d prednisone (preterm delivery) 36 I 656-691 Risk factors for exacerbation of renal disease during pregnancy Renal flares occur in 16-24% of LN pregnancies (often proteinuric); predictors for flares are: a) active renal disease at pregnancy onset (partial renal remission [proteinuria >0.2 but <1 g/24-hr] is associated with RR 3.0 for renal flare during pregnancy and 12 moths post-partum), b) high extra-renal disease activity at pregnancy onset (OR 1.6), c) use of glucocorticoids (OR 1.6) and azathioprine (HR 9.1) at pregnancy onset, d) no use of HCQ (association with higher rates of renal relapse; discontinuation of HCQ is associated with constitutional or arthritis flares), e) aPL positivity (OR 12.4), f) uncontrolled hypertension (OR 6.3) 30 I 656,659,661,663,665- Management of stable renal disease during pregnancy Therapeutic agents include HCQ, GC (non-fluorinated, avoid >7.5 mg/d prednisone for more than 2 weeks), AZA, calcineurin inhibitors, aspirin; control hypertension with calcium-channel blockers, methyldopa, labetalol 4 III 668,682,683,691 Management of renal flare during pregnancy GC (up to 1 mg/kg/day and/or IV-MP pulses); AZA (≤2.5 mg/kg/day); IVIG 10 IV 658,663,665,666,671,679, Monitoring of renal disease activity during pregnancy Similar to adult non-pregnant LN patients; serial measurement of serum C3 and C4 can help differentiate between SLE flare and pre-eclampsia 667,670,671,676,678684,686,690,692-702 680,699,703,704 1 II 705 Q13. Is the management of paediatric lupus nephritis different from that in adult patients? Diagnosis, monitoring, and prognosis Item Outcome and example(s) of effect size Prevalence of paediatric LN Childhood/juvenile-onset SLE patients are at increased risk for renal involvement compared to adult-onset SLE (>60-70% prevalence; OR 1.5-2.4 for proteinuria and/or casts); nephritis is often presenting feature of paediatric SLE; accompanying manifestations at onset are fever (OR 2.6), lymphadenopathy (OR 12.3), malar rash (OR 6.1), and arthritis; paediatric- vs. adult-onset LN: more severe disease (increased renal No. studies Design References 33 I 706-738 20 damage, increased progression to chronic renal insufficiency or ESRD, increased use of immunosuppressive agents) Kidney biopsy for the diagnosis of paediatric LN ISN/RPS 2003 classification (no difference in distribution of histological classes compared to adult patients); histological class correlates with clinical severity of LN (proteinuria level, haematuria, serum albumin, hypertension and need for anti-hypertensive medication) Prognostic value of kidney biopsy findings in paediatric LN Proliferative LN is associated with worse renal outcome than non-proliferative LN; class IV LN is associated with worse outcomes compared to other classes (lower rates of response to therapy, increased damage accrual, higher rates [HR 1.8] of progression to ESRD, reduced patient survival; classes IV-G and mixed V+IV have worse prognosis; fibrinoid necrosis is associated with progression to CRF; biopsy CI correlates with progression to ESRD; tubulo-interstitial lesions correlate with the level of proteinuria, GFR, blood pressure, and progression to CRF; vascular lesions (vasculitis) are associated with increased rates of progression to CRF 21 III 707,718,721,731,736,739-754 Monitoring LN: blood, serological tests, and urinalysis Renal function tests (SCr, GFR), proteinuria, urine sediment, serum C3/C4, serum anti-dsDNA antibodies, serum anti-C1q antibodies, haemoglobin, platelet count, and serum albumin levels have monitoring ability comparable with that in adult SLE patients 14 III 732,748,750,754-764 Monitoring LN: biomarkers Urine NGAL levels show good correlation with the level of proteinuria, renal disease activity indices, kidney biopsy AI and CI (r = 0.39-0.73); urinary proteomics identify biomarkers with very good correlation with renal disease activity; weak evidence for other serum or urine biomarkers 11 III 757,758,761,762,764-770 Monitoring LN: diagnostic and prognostic value of repeat kidney biopsy Histological class transformation into milder forms (if response to therapy) or severe forms (class IV; if no response or severe flare); response to therapy correlates with improvement in pathology findings (particularly reduction in AI); persistent class IV after immunosuppressive treatment is associated with future renal flares 6 III 707,719,731,750,754,771 Prognosis of paediatric LN Increased mortality (~2-fold) (n=2 studies), damage accrual, and comorbidities (infections, cataract, avascular necrosis) compared to adult-onset LN; recently (years 2000-2011) published cohorts: 5-yr patient survival 77-98%, 10-yr rates: 65-92%; renal survival rates: 5-yr 75-94% (median 85%); 10-yr 54-90% (median 80%) 36 III Predictors of adverse outcome: younger onset of LN; male gender (HR 2.6 for patient death); non-White ethnicity (OR 3.3 for ESRD in black patients); renal histological class (worse outcome in class IV; favourable outcome in class II LN); level of proteinuria (urine protein-to-creatinine ratio >1.0 at onset is associated with OR 3.6 for ESRD); low GFR (<80 ml/min/1.73m2); hypertension (at onset or persistent; HR 1.67 for ESRD); anaemia (haemoglobin <10 g/dL) 27 Prognostic factors in paediatric LN [as above] 707,710,713,717719,721,722,727,732,733,736,7 39,740,742-745,747,751,771786 III 707,718,721,727,736,739748,751,752,754,772,777,779,7 80,782,785,787-789 Q13. Is the management of paediatric lupus nephritis different from that in adult patients? ESRD 21 Item Outcome and example(s) of effect size No. studies Design References HD in paediatric LN Increased risk for death in SLE vs. non-SLE paediatric patients on HD (HR 3.1; major causes of mortality are infections, cardiovascular events) (single study); increased risk for complications: less likely to reach target serum albumin levels (OR 0.18), and increased risk for permanent vascular catheter access (OR 2.5; instead of A-V fistulas or grafts) 4 II 582,790-792 Renal transplantation in paediatric LN Comparable renal outcomes versus disease controls (5-yr allograft survival 71% versus 77%); increased mortality in SLE (HR 1.8; 5-yr recipient survival 91% versus 98%); predictors of allograft loss are recipient age (HR 1.05 per 1-yr), female gender (HR 1.2), Black ethnicity (HR 2.0), cadaveric versus living donor transplant (HR 1.3), HLA mismatch, previous rejection (HR 3.1); predictors of recipient mortality are Black ethnicity (HR 1.6) and cadaveric versus living donor transplant (HR 1.9) 2 III 793,794 Q13. Is the management of paediatric lupus nephritis different from that in adult patients? Treatment Item Outcome and example(s) of effect size Class II LN Class III-IV LN: initial treatment No. studies Design References Oral prednisone (starting dose up to 1-2 mg/kg); addition of AZA (2-3 mg/kg/d) or MPA (MMF 300-600 mg/m2) if proteinuria exceeds 1 g/24-hr or SCr exceeds 1.0 mg/dL 1 III 795 2 IV 740,796 Combination of the immunosuppressive agent mizoribine and steroids is not superior than steroids alone in improvement of renal disease parameters or prevention of flares 1 II 797 2 IV 798,799 High-dose GC are used as part of the initial therapeutic regimen: pulses of IV-MP (30 mg/kg, maximum 1g) for 3 consecutive days, followed by oral prednisone 0.5-1 mg/kg/day; alternatively, high-dose oral prednisone (2 mg/kg/day) can be used 3 III 795,800,801 3 V 797,802,803 1 II 804 2 III 802,803 17 V 710,718,740,743,752,75 Combination of GC and CY (IV 0.5-1 g/m2 ×7 monthly pulses or oral 2 mg/kg/day) is the treatment of choice in most studies with complete response rates 50-70%; benefit over AZA in long-term (8 years) preservation of renal function and patient survival; the regimen is efficacious in steroid-refractory LN, in cases with nephrotic syndrome, abnormal GFR and/or adverse histology (crescents) 4,785,796,805-813 22 Class III-IV LN: subsequent treatment Combination of GC and MPA (MMF 300-900 mg/m2) is efficacious in class III-IV LN cases with preserved renal function; comparable short-term (6 months) efficacy with pulses IV-CY in class III LN; results from epidemiological studies suggest survival benefit since its introduction in the management of paediatric class III-IV LN 1 II 802 3 V 755,814,815 Combination of GC and AZA (2-3 mg/kg/day) is efficacious in mild LN cases 2 III 795,803 2 V 740,743 Combination of GC and calcineurin inhibitors (CsA, tacrolimus). Comparable efficacy of CsA (5 mg/kg/day) with the combination of high-dose steroids (2 mg/kg) plus oral CY (2 mg/kg) in reducing proteinuria in steroidrefractory class III-IV LN; ‘triple regimen’ (GC/MMF/CsA) has been used in severe LN cases 1 II 804 3 V 740,755,816 Combination of GC and oral mizoribine shows trend for reduced flares during 1-yr follow-up (single RCT); improvements in serology and proteinuria 1 II 797 4 V 798,799,817,818 Combination of low-dose GC with IV-CY (quarterly pulses) has been used in severe cases with low GFR, highlevel proteinuria, or crescents 2 III 802,803 7 V 754,807-811,813 Combination of low-dose GC with AZA has been used after successful induction with pulse IV-CY; relapses are common 1 III 803 3 V 752,806,811 Combination of low-dose GC with MPA is efficacious in patients who relapsed on AZA; has been used after initial treatment with either MPA or pulse IV-CY (including cases with crescentic nephritis) 1 III 802 5 V 806,808,811,814,815 Other agents: calcineurin inhibitors, mizoribine 1 II 804 5 V 755,798,816-818 23 Class V LN Refractory or relapsing LN 4 V 787,796,818,819 MPA (if failure to CY, AZA, or CsA) 2 V 814,820 Calcineurin inhibitors (CsA, tacrolimus) 3 V 816,818,821 Methotrexate (oral; combination of IV methotrexate with IV-CY); associated with significant toxicity 2 V 822,823 IVIG (400 mg/kg/d for 5 days): induction of sustained renal response; improved histology 1 V 824 Mizoribine: improvements in proteinuria and serology 3 V 818,825,826 RTX (miscellaneous regimens; 750 mg/m2 on days 1 and 15) alone or with concurrent/subsequent immunosuppression (MPA, AZA, or IV-CY): improvements in proteinuria, serum albumin levels, serology, and general SLE activity; steroid-sparring effect; complete renal remission 25-50%; partial renal remission rates 50% 3 V 827-829 Plasma exchange: used in cases of refractory class III-IV LN, rapidly progressive glomerulonephritis, concomitant micrangiopathy 3 V 740,830,831 Oral GC (0.5-2 mg/kg/day) alone or in combination with immunosuppressive agent (usually AZA; also IV-CY, calcineurin inhibitors, MPA) Abbreviations: ACEi, ACE-inhibitor; AI, activity index; aPL, antiphospholipid antibody; APS, antiphospholipid syndrome; APSN, APS-associated nephropathy; ARB, angiotensin receptor blocker; AZA, azathioprine; CI, chronicity index; CRF, chronic renal failure; CsA, ciclosporin A; CY, cyclophosphamide; ESRD, end-stage renal disease; GC, glucocorticoids; GFR, glomerular filtration rate; HCQ, hydroxychloroquine; HD, haemodialysis; HR, hazard ratio; HUS, haemolytic-uremic syndrome; ISN/RPS, International Society of Nephrology / Renal Pathology Society; IUGR, intra-uterine growth restriction; IV-CY, intravenous cyclophosphamide; IVIG, intravenous immunoglobulin; IV-MP, intravenous methyl-prednisolone; LN, lupus nephritis; LR, likelihood ratio; MDRD, Modification of Diet in Renal Disease; MPA, mycophenolic acid; NIH, National Institutes of Health; OR, odds ratio; PD, peritoneal dialysis; RBC, red blood cells; RCT, randomized controlled trial; RR, relative risk; RTX, rituximab; SCr, serum creatinine; TTP, thrombocytopenic thrombotic purpura; WBC, white blood cells; WHO, World Health Organization 1 The study design is assigned as follows: I, meta-analysis of RCTs; II, RCT (including long-term follow-up of original RCT using the same randomisation allocation); III, prospective controlled (non-randomized) study or epidemiological studies with prospective collection of data; IV, retrospective controlled or cross-sectional study, V, uncontrolled study (case series) References 24 1. Appel GB, Silva FG, Pirani CL, Meltzer JI, Estes D. Renal involvement in systemic lupud erythematosus (SLE): a study of 56 patients emphasizing histologic classification. Medicine (Baltimore) 1978;57:371-410. 2. Bhinder S, Singh A, Majithia V. Membranous (class V) renal disease in systemic lupus erythematosus may be more common than previously reported: results of a 6-year retrospective analysis. Am J Med Sci 2010;339:230-2. 3. Faurschou M, Starklint H, Halberg P, Jacobsen S. Prognostic factors in lupus nephritis: diagnostic and therapeutic delay increases the risk of terminal renal failure. J Rheumatol 2006;33:1563-9. 4. Franco C, Yoo W, Franco D, Xu Z. Predictors of end stage renal disease in African Americans with lupus nephritis. Bull NYU Hosp Jt Dis 2010;68:251-6. 5. Grootscholten C, Bajema IM, Florquin S, et al. Interobserver agreement of scoring of histopathological characteristics and classification of lupus nephritis. Nephrol Dial Transplant 2008;23:223-30. 6. Guo Q, Lu X, Miao L, Wu M, Lu S, Luo P. Analysis of clinical manifestations and pathology of lupus nephritis: a retrospective review of 82 cases. Clin Rheumatol 2010;29:1175-80. 7. Hill GS, Delahousse M, Nochy D, et al. A new morphologic index for the evaluation of renal biopsies in lupus nephritis. Kidney Int 2000;58:1160-73. 8. Hsieh C, Chang A, Brandt D, Guttikonda R, Utset TO, Clark MR. Predicting outcomes of lupus nephritis with tubulointerstitial inflammation and scarring. Arthritis Care Res (Hoboken) 2011;63:865-74. 9. Hurtado A, Asato C, Escudero E, et al. Clinicopathologic correlations in lupus nephritis in Lima, Peru. Nephron 1999;83:323-30. 10. Laitman RS, Glicklich D, Sablay LB, Grayzel AI, Barland P, Bank N. Effect of long-term normalization of serum complement levels on the course of lupus nephritis. Am J Med 1989;87:132-8. 11. Leaker B, Fairley KF, Dowling J, Kincaid-Smith P. Lupus nephritis: clinical and pathological correlation. Q J Med 1987;62:163-79. 12. Mittal B, Hurwitz S, Rennke H, Singh AK. New subcategories of class IV lupus nephritis: are there clinical, histologic, and outcome differences? Am J Kidney Dis 2004;44:1050-9. 13. Nossent HC, Henzen-Logmans SC, Vroom TM, Berden JH, Swaak TJ. Contribution of renal biopsy data in predicting outcome in lupus nephritis. Analysis of 116 patients. Arthritis Rheum 1990;33:970-7. 14. Williams W, Shah D, Sargeant LA. The clinical and epidemiologic features in 140 patients with lupus nephritis in a predominantly black population from one center in Kingston, Jamaica. Am J Med Sci 2004;327:324-9. 15. Yamamoto T, Nagase M, Hishida A, Honda N. Interstitial inflammatory and chronic tubulointerstitial lesions in lupus nephritis: comparison with those in IgA nephropathy. Lupus 1993;2:261-8. 16. Yokoyama H, Wada T, Hara A, et al. The outcome and a new ISN/RPS 2003 classification of lupus nephritis in Japanese. Kidney Int 2004;66:2382-8. 17. Yu F, Tan Y, Liu G, Wang SX, Zou WZ, Zhao MH. Clinicopathological characteristics and outcomes of patients with crescentic lupus nephritis. Kidney Int 2009;76:307-17. 18. Yu F, Tan Y, Wu LH, Zhu SN, Liu G, Zhao MH. Class IV-G and IV-S lupus nephritis in Chinese patients: a large cohort study from a single center. Lupus 2009;18:1073-81. 19. Al Durahim H, Al Ghamdi G, Al Seraya A, Alkhiari R, Al Sayyari A. Predictors of mortality and end stage renal disease in Saudi patients with lupus nephritis. Lupus 2011;20:1329-35. 20. Godfrey T, Cuadrado MJ, Fofi C, et al. Chromium-51 ethylenediamine tetraacetic acid glomerular filtration rate: a better predictor than glomerular filtration rate calculated by the Cockcroft-Gault formula for renal involvement in systemic lupus erythematosus patients. Rheumatology (Oxford) 2001;40:324-8. 21. Khajehdehi P, Rajaee A, Jalali GA, Behzadi S. Lupus nephritis in patients of Iranian origin: differences in clinical and histopathological features at initial presentation. Nephrol Dial Transplant 1997;12:363-4. 22. Patel SB, Korbet SM, Lewis EJ. The prognosis of severe lupus nephritis based on the Modification of Diet in Renal Disease (MDRD) study estimated glomerular filtration rate. Lupus 2011;20:256-64. 23. Grootscholten C, Bajema IM, Florquin S, et al. Treatment with cyclophosphamide delays the progression of chronic lesions more effectively than does treatment with azathioprine plus methylprednisolone in patients with proliferative lupus nephritis. Arthritis Rheum 2007;56:924-37. 24. Chen T, Ding X, Chen B. Value of the RIFLE classification for acute kidney injury in diffuse proliferative lupus nephritis. Nephrol Dial Transplant 2009;24:3115-20. 25 25. Banfi G, Mazzucco G, Barbiano di Belgiojoso G, et al. Morphological parameters in lupus nephritis: their relevance for classification and relationship with clinical and histological findings and outcome. Q J Med 1985;55:153-68. 26. Cavallo T, Cameron WR, Lapenas D. Immunopathology of early and clinically silent lupus nephropathy. Am J Pathol 1977;87:1-18. 27. Gladman DD, Urowitz MB, Cole E, Ritchie S, Chang CH, Churg J. Kidney biopsy in SLE. I. A clinical-morphologic evaluation. Q J Med 1989;73:1125-33. 28. Jacobsen S, Starklint H, Petersen J, et al. Prognostic value of renal biopsy and clinical variables in patients with lupus nephritis and normal serum creatinine. Scand J Rheumatol 1999;28:288-99. 29. Appenzeller S, Clark A, Pineau C, Vasilevsky M, Bernatsky S. Isolated pyuria in systemic lupus erythematosus. Lupus 2010;19:793-6. 30. Abd-Elkareem MI, Al Tamimy HM, Khamis OA, Abdellatif SS, Hussein MR. Increased urinary levels of the leukocyte adhesion molecules ICAM-1 and VCAM-1 in human lupus nephritis with advanced renal histological changes: preliminary findings. Clin Exp Nephrol 2010;14:548-57. 31. Christopher-Stine L, Siedner M, Lin J, et al. Renal biopsy in lupus patients with low levels of proteinuria. J Rheumatol 2007;34:332-5. 32. Hill GS, Delahousse M, Nochy D, Mandet C, Bariety J. Proteinuria and tubulointerstitial lesions in lupus nephritis. Kidney Int 2001;60:1893-903. 33. Hill GS, Delahousse M, Nochy D, Bariety J. Class IV-S versus class IV-G lupus nephritis: clinical and morphologic differences suggesting different pathogenesis. Kidney Int 2005;68:2288-97. 34. Monga G, Mazzucco G, Castello R. Glomerular monocyte infiltration in human nephropathies: prevalence and correlation with clinical and morphological variables. Virchows Arch A Pathol Anat Histopathol 1985;405:483-96. 35. Rahman P, Gladman DD, Ibanez D, Urowitz MB. Significance of isolated haematuria and isolated pyuria in systemic lupus erythematosus. Lupus 2001;10:418-23. 36. Valente de Almeida R, Rocha de Carvalho JG, de Azevedo VF, et al. Microalbuminuria and renal morphology in the evaluation of subclinical lupus nephritis. Clin Nephrol 1999;52:218-29. 37. Font J, Torras A, Cervera R, Darnell A, Revert L, Ingelmo M. Silent renal disease in systemic lupus erythematosus. Clin Nephrol 1987;27:283-8. 38. Stamenkovic I, Favre H, Donath A, Assimacopoulos A, Chatelanat F. Renal biopsy in SLE irrespective of clinical findings: long-term follow-up. Clin Nephrol 1986;26:109-15. 39. Bennett WM, Bardana EJ, Norman DJ, Houghton DC. Natural history of "silent" lupus nephritis. Am J Kidney Dis 1982;1:359-63. 40. Leehey DJ, Katz AI, Azaran AH, Aronson AJ, Spargo BH. Silent diffuse lupus nephritis: long-term follow-up. Am J Kidney Dis 1982;2:188-96. 41. Mahajan SK, Ordonez NG, Feitelson PJ, Lim VS, Spargo BH, Katz AI. Lupus nephropathy without clinical renal involvement. Medicine (Baltimore) 1977;56:493-501. 42. O'Dell JR, Hays RC, Guggenheim SJ, Steigerwald JC. Systemic lupus erythematosus without clinical renal abnormalities: renal biopsy findings and clinical course. Ann Rheum Dis 1985;44:415-9. 43. Wada Y, Ito S, Ueno M, Nakano M, Arakawa M, Gejyo F. Renal outcome and predictors of clinical renal involvement in patients with silent lupus nephritis. Nephron Clin Pract 2004;98:c105-11. 44. Zabaleta-Lanz M, Vargas-Arenas RE, Tapanes F, Daboin I, Atahualpa Pinto J, Bianco NE. Silent nephritis in systemic lupus erythematosus. Lupus 2003;12:26-30. 45. Zabaleta-Lanz ME, Munoz LE, Tapanes FJ, et al. Further description of early clinically silent lupus nephritis. Lupus 2006;15:845-51. 46. Esdaile JM, Levinton C, Federgreen W, Hayslett JP, Kashgarian M. The clinical and renal biopsy predictors of long-term outcome in lupus nephritis: a study of 87 patients and review of the literature. Q J Med 1989;72:779-833. 47. Esdaile JM, Federgreen W, Quintal H, Suissa S, Hayslett JP, Kashgarian M. Predictors of one year outcome in lupus nephritis: the importance of renal biopsy. Q J Med 1991;81:907-18. 48. Faurschou M, Dreyer L, Kamper AL, Starklint H, Jacobsen S. Long-term mortality and renal outcome in a cohort of 100 patients with lupus nephritis. Arthritis Care Res (Hoboken) 2010;62:873-80. 49. Elyan M, Ballou S. The effectiveness and safety of mycophenolate mofetil in lupus nephritis. Clin Rheumatol 2009;28:835-40. 50. Lindeman RD, Pederson JA, Matter BJ, Laughlin LO, Mandal AK. Long-term azathioprine-corticosteroid therapy in lupus nephritis and idiopathic nephrotic syndrome. J Chronic Dis 1976;29:189-204. 51. Esdaile JM, Joseph L, MacKenzie T, Kashgarian M, Hayslett JP. The benefit of early treatment with immunosuppressive agents in lupus nephritis. J Rheumatol 1994;21:204651. 52. Weening JJ, D'Agati VD, Schwartz MM, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. J Am Soc Nephrol 2004;15:241-50. 26 53. Furness PN, Taub N. Interobserver reproducibility and application of the ISN/RPS classification of lupus nephritis-a UK-wide study. Am J Surg Pathol 2006;30:1030-5. 54. Hwang J, Kim HJ, Oh JM, et al. Outcome of reclassification of World Health Organization (WHO) class III under International Society of Nephrology-Renal Pathology Society (ISN-RPS) classification: retrospective observational study. Rheumatol Int 2011. 55. Schwartz MM, Korbet SM, Lewis EJ. The prognosis and pathogenesis of severe lupus glomerulonephritis. Nephrol Dial Transplant 2008;23:1298-306. 56. Appel GB, Cohen DJ, Pirani CL, Meltzer JI, Estes D. Long-term follow-up of patients with lupus nephritis. A study based on the classification of the World Health Organization. Am J Med 1987;83:877-85. 57. Austin HA, 3rd, Muenz LR, Joyce KM, et al. Prognostic factors in lupus nephritis. Contribution of renal histologic data. Am J Med 1983;75:382-91. 58. Ayodele OE, Okpechi IG, Swanepoel CR. Predictors of poor renal outcome in patients with biopsy-proven lupus nephritis. Nephrology (Carlton) 2010;15:482-90. 59. Baldwin DS, Gluck MC, Lowenstein J, Gallo GR. Lupus nephritis. Clinical course as related to morphologic forms and their transitions. Am J Med 1977;62:12-30. 60. Barr RG, Seliger S, Appel GB, et al. Prognosis in proliferative lupus nephritis: the role of socio-economic status and race/ethnicity. Nephrol Dial Transplant 2003;18:2039-46. 61. Blanco FJ, De la Mata J, Lopez-Fernandez JI, Gomez-Reino JJ. Light, immunofluorescence and electron microscopy renal biopsy findings as predictors of mortality in eightyfive Spanish patients with systemic lupus erythematosus. Br J Rheumatol 1994;33:260-6. 62. Bujan S, Ordi-Ros J, Paredes J, et al. Contribution of the initial features of systemic lupus erythematosus to the clinical evolution and survival of a cohort of Mediterranean patients. Ann Rheum Dis 2003;62:859-65. 63. Cai X, Yang X, Lian F, et al. Correlation between serum anti-C1q antibody levels and renal pathological characteristics and prognostic significance of anti-C1q antibody in lupus nephritis. J Rheumatol 2010;37:759-65. 64. Cheatum DE, Hurd ER, Strunk SW, Ziff M. Renal histology and clinical course of systemic lupus erythematosus. A prospective study. Arthritis Rheum 1973;16:670-6. 65. Contreras G, Pardo V, Cely C, et al. Factors associated with poor outcomes in patients with lupus nephritis. Lupus 2005;14:890-5. 66. Derksen RH, Hene RJ, Kater L. The long-term clinical outcome of 56 patients with biopsy-proven lupus nephritis followed at a single center. Lupus 1992;1:97-103. 67. Descombes E, Droz D, Drouet L, Grunfeld JP, Lesavre P. Renal vascular lesions in lupus nephritis. Medicine (Baltimore) 1997;76:355-68. 68. Donadio JV, Jr., Hart GM, Bergstralh EJ, Holley KE. Prognostic determinants in lupus nephritis: a long-term clinicopathologic study. Lupus 1995;4:109-15. 69. Font J, Ramos-Casals M, Cervera R, et al. Cardiovascular risk factors and the long-term outcome of lupus nephritis. Qjm 2001;94:19-26. 70. Fries JF, Porta J, Liang MH. Marginal benefit of renal biopsy in systemic lupus erythematosus. Arch Intern Med 1978;138:1386-9. 71. Howie AJ, Turhan N, Adu D. Powerful morphometric indicator of prognosis in lupus nephritis. Qjm 2003;96:411-20. 72. Huong DL, Papo T, Beaufils H, et al. Renal involvement in systemic lupus erythematosus. A study of 180 patients from a single center. Medicine (Baltimore) 1999;78:148-66. 73. Korbet SM, Lewis EJ, Schwartz MM, Reichlin M, Evans J, Rohde RD. Factors predictive of outcome in severe lupus nephritis. Lupus Nephritis Collaborative Study Group. Am J Kidney Dis 2000;35:904-14. 74. Magil AB, Ballon HS, Rae A. Focal proliferative lupus nephritis. A clinicopathologic study using the W.H.O. classification. Am J Med 1982;72:620-30. 75. McLaughlin J, Gladman DD, Urowitz MB, Bombardier C, Farewell VT, Cole E. Kidney biopsy in systemic lupus erythematosus. II. Survival analyses according to biopsy results. Arthritis Rheum 1991;34:1268-73. 76. McLaughlin JR, Bombardier C, Farewell VT, Gladman DD, Urowitz MB. Kidney biopsy in systemic lupus erythematosus. III. Survival analysis controlling for clinical and laboratory variables. Arthritis Rheum 1994;37:559-67. 77. Mok CC, Wong RW, Lau CS. Lupus nephritis in Southern Chinese patients: clinicopathologic findings and long-term outcome. Am J Kidney Dis 1999;34:315-23. 78. Najafi CC, Korbet SM, Lewis EJ, Schwartz MM, Reichlin M, Evans J. Significance of histologic patterns of glomerular injury upon long-term prognosis in severe lupus glomerulonephritis. Kidney Int 2001;59:2156-63. 79. Parichatikanond P, Francis ND, Malasit P, et al. Lupus nephritis: clinicopathological study of 162 cases in Thailand. J Clin Pathol 1986;39:160-6. 80. Pons-Estel GJ, Alarcon GS, McGwin G, Jr., et al. Protective effect of hydroxychloroquine on renal damage in patients with lupus nephritis: LXV, data from a multiethnic US cohort. Arthritis Rheum 2009;61:830-9. 81. Ravinal RC, Costa RS, Coimbra TM, et al. Classes, activity and chronicity indices, and alpha-smooth muscle actin expression as prognostic parameters in lupus nephritis outcome. Lupus 2002;11:82-7. 27 82. Neumann K, Wallace DJ, Azen C, et al. Lupus in the 1980s: III. Influence of clinical variables, biopsy, and treatment on the outcome in 150 patients with lupus nephritis seen at a single center. Semin Arthritis Rheum 1995;25:47-55. 83. Shayakul C, Ong-aj-yooth L, Chirawong P, et al. Lupus nephritis in Thailand: clinicopathologic findings and outcome in 569 patients. Am J Kidney Dis 1995;26:300-7. 84. Shilov EM, Krasnova TN, Ivanov AA, Tareyeva IE. Prognostic factors in lupus nephritis treated with cyclophosphamide pulses. Nephron 1994;66:488-9. 85. Wang F, Looi LM. Systemic lupus erythematosus with membranous lupus nephropathy in Malaysian patients. Q J Med 1984;53:209-26. 86. Kimberly RP, Lockshin MD, Sherman RL, Beary JF, Mouradian J, Cheigh JS. "End-stage" lupus nephritis: clinical course to and outcome on dialysis. Experience with 39 patients. Medicine (Baltimore) 1981;60:277-87. 87. Ioannidis JP, Boki KA, Katsorida ME, et al. Remission, relapse, and re-remission of proliferative lupus nephritis treated with cyclophosphamide. Kidney Int 2000;57:258-64. 88. F L, Y T, X P, et al. A prospective multicentre study of mycophenolate mofetil combined with prednisolone as induction therapy in 213 patients with active lupus nephritis. Lupus 2008;17:622-9. 89. Urowitz MB, Feletar M, Bruce IN, Ibanez D, Gladman DD. Prolonged remission in systemic lupus erythematosus. J Rheumatol 2005;32:1467-72. 90. Mitjavila F, Pac V, Moga I, et al. Clinicopathological correlations and prognostic factors in lupus nephritis. Clin Exp Rheumatol 1997;15:625-31. 91. Bakir AA, Levy PS, Dunea G. The prognosis of lupus nephritis in African-Americans: a retrospective analysis. Am J Kidney Dis 1994;24:159-71. 92. Schwartz MM, Bernstein J, Hill GS, Holley K, Phillips EA. Predictive value of renal pathology in diffuse proliferative lupus glomerulonephritis. Lupus Nephritis Collaborative Study Group. Kidney Int 1989;36:891-6. 93. Chen Q, Liu Z, Hu W, Chen H, Zeng C, Li L. Class V lupus nephritis: a clinicopathologic study in 152 patients. J Nephrol 2003;16:126-32. 94. Behara VY, Whittier WL, Korbet SM, Schwartz MM, Martens M, Lewis EJ. Pathogenetic features of severe segmental lupus nephritis. Nephrol Dial Transplant 2010;25:153-9. 95. Schwartz MM, Kawala KS, Corwin HL, Lewis EJ. The prognosis of segmental glomerulonephritis in systemic lupus erythematosus. Kidney Int 1987;32:274-9. 96. Kolasinski SL, Chung JB, Albert DA. What do we know about lupus membranous nephropathy? An analytic review. Arthritis Rheum 2002;47:450-5. 97. Couzi L, Merville P, Deminiere C, et al. Predominance of CD8+ T lymphocytes among periglomerular infiltrating cells and link to the prognosis of class III and class IV lupus nephritis. Arthritis Rheum 2007;56:2362-70. 98. Hiramatsu N, Kuroiwa T, Ikeuchi H, et al. Revised classification of lupus nephritis is valuable in predicting renal outcome with an indication of the proportion of glomeruli affected by chronic lesions. Rheumatology (Oxford) 2008;47:702-7. 99. Kim YG, Kim HW, Cho YM, et al. The difference between lupus nephritis class IV-G and IV-S in Koreans: focus on the response to cyclophosphamide induction treatment. Rheumatology (Oxford) 2008;47:311-4. 100.Kojo S, Sada KE, Kobayashi M, et al. Clinical usefulness of a prognostic score in histological analysis of renal biopsy in patients with lupus nephritis. J Rheumatol 2009;36:2218-23. 101.Yu F, Wu LH, Tan Y, et al. Tubulointerstitial lesions of patients with lupus nephritis classified by the 2003 International Society of Nephrology and Renal Pathology Society system. Kidney Int 2010;77:820-9. 102.Alexopoulos E, Seron D, Hartley RB, Cameron JS. Lupus nephritis: correlation of interstitial cells with glomerular function. Kidney Int 1990;37:100-9. 103.Nossent H, Berden J, Swaak T. Renal immunofluorescence and the prediction of renal outcome in patients with proliferative lupus nephritis. Lupus 2000;9:504-10. 104.Tuma SN, Llach F, Sostrin S, Dubois EL, Massry SG. Glomerular IgE deposits in patients with lupus nephritis. Am J Nephrol 1981;1:31-6. 105.Magil AB, Ballon HS, Chan V, Lirenman DS, Rae A, Sutton RA. Diffuse proliferative lupus glomerulonephritis. Determination of prognostic significance of clinical, laboratory and pathologic factors. Medicine (Baltimore) 1984;63:210-20. 106.Park MH, D'Agati V, Appel GB, Pirani CL. Tubulointerstitial disease in lupus nephritis: relationship to immune deposits, interstitial inflammation, glomerular changes, renal function, and prognosis. Nephron 1986;44:309-19. 107.Esdaile JM, Joseph L, MacKenzie T, Kashgarian M, Hayslett JP. The pathogenesis and prognosis of lupus nephritis: information from repeat renal biopsy. Semin Arthritis Rheum 1993;23:135-48. 108.Grishman E, Porush JG, Lee SL, Churg J. Renal biopsies in lupus nephritis. Correlation of electron microscopic findings with clinical course. Nephron 1973;10:25-36. 109.Tateno S, Kobayashi Y, Shigematsu H, Hiki Y. Study of lupus nephritis: its classification and the significance of subendothelial deposits. Q J Med 1983;52:311-31. 28 110.Whiting-O'Keefe Q, Riccardi PJ, Henke JE, Shearn MA, Hopper J, Jr., Epstein WV. Recognition of information in renal biopsies of patients with lupus nephritis. Ann Intern Med 1982;96:723-7. 111.Whiting-O'Keefe Q, Henke JE, Shearn MA, Hopper J, Jr., Biava CG, Epstein WV. The information content from renal biopsy in systemic lupus erythematosus. Ann Intern Med 1982;96:718-23. 112.Schwartz MM, Roberts JL, Lewis EJ. Subepithelial electron-dense deposits in proliferative glomerulonephritis of systemic lupus erythematosus. Ultrastruct Pathol 1982;3:10518. 113.Austin HA, 3rd, Muenz LR, Joyce KM, Antonovych TT, Balow JE. Diffuse proliferative lupus nephritis: identification of specific pathologic features affecting renal outcome. Kidney Int 1984;25:689-95. 114.McCune WJ, Saluja M, Bhat S, Lange LA, Holzman L, Johnson K. Correlation of membranous glomerular ultrastructural changes with disease severity and outcome in lupus patients initiating cyclophosphamide therapy. Lupus 2005;14:426-33. 115.Moroni G, Pasquali S, Quaglini S, et al. Clinical and prognostic value of serial renal biopsies in lupus nephritis. Am J Kidney Dis 1999;34:530-9. 116.O'Dell JR, Hays RC, Guggenheim SJ, Steigerwald JC. Tubulointerstitial renal disease in systemic lupus erythematosus. Arch Intern Med 1985;145:1996-9. 117.Sun HO, Hu WX, Xie HL, et al. Long-term outcome of Chinese patients with membranous lupus nephropathy. Lupus 2008;17:56-61. 118.Yoo CW, Kim MK, Lee HS. Predictors of renal outcome in diffuse proliferative lupus nephropathy: data from repeat renal biopsy. Nephrol Dial Transplant 2000;15:1604-8. 119.Arce-Salinas CA, Villa AR, Martinez-Rueda JO, et al. Factors associated with chronic renal failure in 121 patients with diffuse proliferative lupus nephritis: a case-control study. Lupus 1995;4:197-203. 120.Austin HA, 3rd, Boumpas DT, Vaughan EM, Balow JE. Predicting renal outcomes in severe lupus nephritis: contributions of clinical and histologic data. Kidney Int 1994;45:544-50. 121.Austin HA, 3rd, Boumpas DT, Vaughan EM, Balow JE. High-risk features of lupus nephritis: importance of race and clinical and histological factors in 166 patients. Nephrol Dial Transplant 1995;10:1620-8. 122.Magil AB, Puterman ML, Ballon HS, et al. Prognostic factors in diffuse proliferative lupus glomerulonephritis. Kidney Int 1988;34:511-7. 123.Mok CC, Ho CT, Chan KW, Lau CS, Wong RW. Outcome and prognostic indicators of diffuse proliferative lupus glomerulonephritis treated with sequential oral cyclophosphamide and azathioprine. Arthritis Rheum 2002;46:1003-13. 124.Mosca M, Bencivelli W, Neri R, et al. Renal flares in 91 SLE patients with diffuse proliferative glomerulonephritis. Kidney Int 2002;61:1502-9. 125.Schwartz MM, Lan SP, Bernstein J, Hill GS, Holley K, Lewis EJ. Role of pathology indices in the management of severe lupus glomerulonephritis. Lupus Nephritis Collaborative Study Group. Kidney Int 1992;42:743-8. 126.Illei GG, Takada K, Parkin D, et al. Renal flares are common in patients with severe proliferative lupus nephritis treated with pulse immunosuppressive therapy: long-term followup of a cohort of 145 patients participating in randomized controlled studies. Arthritis Rheum 2002;46:995-1002. 127.Daniel L, Sichez H, Giorgi R, et al. Tubular lesions and tubular cell adhesion molecules for the prognosis of lupus nephritis. Kidney Int 2001;60:2215-21. 128.Schwartz MM, Korbet SM, Katz RS, Lewis EJ. Evidence of concurrent immunopathological mechanisms determining the pathology of severe lupus nephritis. Lupus 2009;18:149-58. 129.Bao H, Liu ZH, Xie HL, Hu WX, Zhang HT, Li LS. Successful treatment of class V+IV lupus nephritis with multitarget therapy. J Am Soc Nephrol 2008;19:2001-10. 130.Cortes-Hernandez J, Ordi-Ros J, Labrador M, et al. Predictors of poor renal outcome in patients with lupus nephritis treated with combined pulses of cyclophosphamide and methylprednisolone. Lupus 2003;12:287-96. 131.Faurschou M, Penkowa M, Andersen CB, Starklint H, Jacobsen S. The renal metallothionein expression profile is altered in human lupus nephritis. Arthritis Res Ther 2008;10:R76. 132.Martins L, Rocha G, Rodrigues A, et al. Lupus nephritis: a retrospective review of 78 cases from a single center. Clin Nephrol 2002;57:114-9. 133.Mok CC, Ying KY, Tang S, et al. Predictors and outcome of renal flares after successful cyclophosphamide treatment for diffuse proliferative lupus glomerulonephritis. Arthritis Rheum 2004;50:2559-68. 134.Mok CC, Ying KY, Ng WL, et al. Long-term outcome of diffuse proliferative lupus glomerulonephritis treated with cyclophosphamide. Am J Med 2006;119:355 e25-33. 135.Moroni G, Quaglini S, Maccario M, Banfi G, Ponticelli C. "Nephritic flares" are predictors of bad long-term renal outcome in lupus nephritis. Kidney Int 1996;50:2047-53. 29 136.Moroni G, Quaglini S, Gallelli B, Banfi G, Messa P, Ponticelli C. The long-term outcome of 93 patients with proliferative lupus nephritis. Nephrol Dial Transplant 2007;22:2531-9. 137.Mosca M, Pasquariello A, Tavoni A, et al. Predictors of renal outcome in diffuse proliferative glomerulonephritis in systemic lupus erythematosus. Lupus 1997;6:371-8. 138.Wallace DJ, Goldfinger D, Savage G, et al. Predictive value of clinical, laboratory, pathologic, and treatment variables in steroid/immunosuppressive resistant lupus nephritis. J Clin Apher 1988;4:30-4. 139.Carette S, Klippel JH, Decker JL, et al. Controlled studies of oral immunosuppressive drugs in lupus nephritis. A long-term follow-up. Ann Intern Med 1983;99:1-8. 140.Chan TM, Tse KC, Tang CS, Lai KN, Li FK. Long-term outcome of patients with diffuse proliferative lupus nephritis treated with prednisolone and oral cyclophosphamide followed by azathioprine. Lupus 2005;14:265-72. 141.Chen YE, Korbet SM, Katz RS, Schwartz MM, Lewis EJ. Value of a complete or partial remission in severe lupus nephritis. Clin J Am Soc Nephrol 2008;3:46-53. 142.Ciruelo E, de la Cruz J, Lopez I, Gomez-Reino JJ. Cumulative rate of relapse of lupus nephritis after successful treatment with cyclophosphamide. Arthritis Rheum 1996;39:2028-34. 143.Lim CS, Chin HJ, Jung YC, et al. Prognostic factors of diffuse proliferative lupus nephritis. Clin Nephrol 1999;52:139-47. 144.Kanno A, Hotta O, Yusa N, Taguma Y. Predictive factors of clinical outcome in patients with diffuse proliferative lupus nephritis treated early by intravenous methylprednisolone pulse therapy. Ren Fail 2007;29:41-7. 145.Conlon PJ, Fischer CA, Levesque MC, et al. Clinical, biochemical and pathological predictors of poor response to intravenous cyclophosphamide in patients with proliferative lupus nephritis. Clin Nephrol 1996;46:170-5. 146.Tsumagari T, Fukumoto S, Kinjo M, Tanaka K. Incidence and significance of intrarenal vasculopathies in patients with systemic lupus erythematosus. Hum Pathol 1985;16:439. 147.Banfi G, Bertani T, Boeri V, et al. Renal vascular lesions as a marker of poor prognosis in patients with lupus nephritis. Gruppo Italiano per lo Studio della Nefrite Lupica (GISNEL). Am J Kidney Dis 1991;18:240-8. 148.Atta AM, Pereira MM, Santiago M, Sousa-Atta ML. Anti-dsDNA antibodies in Brazilian patients of mainly African descent with systemic lupus erythematosus: lack of association with lupus nephritis. Clin Rheumatol 2009;28:693-7. 149.Akhter E, Burlingame RW, Seaman AL, Magder L, Petri M. Anti-C1q antibodies have higher correlation with flares of lupus nephritis than other serum markers. Lupus 2011;20:1267-74. 150.Asero R, Banfi G, Radelli L, et al. Relationship between antibodies to dsDNA and to soluble cellular antigens and histologically defined glomerulonephritis in patients with SLE. Autoimmunity 1990;7:13-21. 151.D'Cruz DP, Houssiau FA, Ramirez G, et al. Antibodies to endothelial cells in systemic lupus erythematosus: a potential marker for nephritis and vasculitis. Clin Exp Immunol 1991;85:254-61. 152.Oelzner P, Deliyska B, Funfstuck R, Hein G, Herrmann D, Stein G. Anti-C1q antibodies and antiendothelial cell antibodies in systemic lupus erythematosus - relationship with disease activity and renal involvement. Clin Rheumatol 2003;22:271-8. 153.Houssiau FA, D'Cruz D, Vianna J, Hughes GR. Lupus nephritis: the significance of serological tests at the time of biopsy. Clin Exp Rheumatol 1991;9:345-9. 154.Nossent JC, Henzen-Logmans SC, Vroom TM, Huysen V, Berden JH, Swaak AJ. Relation between serological data at the time of biopsy and renal histology in lupus nephritis. Rheumatol Int 1991;11:77-82. 155.Gunnarsson I, Ronnelid J, Huang YH, et al. Association between ongoing anti-C1q antibody production in peripheral blood and proliferative nephritis in patients with active systemic lupus erythematosus. Br J Rheumatol 1997;36:32-7. 156.do Nascimento AP, Viana Vdos S, Testagrossa Lde A, et al. Antibodies to ribosomal P proteins: a potential serologic marker for lupus membranous glomerulonephritis. Arthritis Rheum 2006;54:1568-72. 157.Okamura M, Kanayama Y, Amastu K, et al. Significance of enzyme linked immunosorbent assay (ELISA) for antibodies to double stranded and single stranded DNA in patients with lupus nephritis: correlation with severity of renal histology. Ann Rheum Dis 1993;52:14-20. 158.Bigler C, Lopez-Trascasa M, Potlukova E, et al. Antinucleosome antibodies as a marker of active proliferative lupus nephritis. Am J Kidney Dis 2008;51:624-9. 30 159.Cortes-Hernandez J, Ordi-Ros J, Labrador M, et al. Antihistone and anti-double-stranded deoxyribonucleic acid antibodies are associated with renal disease in systemic lupus erythematosus. Am J Med 2004;116:165-73. 160.Perry GJ, Elston T, Khouri NA, Chan TM, Cameron JS, Frampton G. Antiendothelial cell antibodies in lupus: correlations with renal injury and circulating markers of endothelial damage. Q J Med 1993;86:727-34. 161.Tron F, Bach JF. Relationships between antibodies to native DNA and glomerulonephritis in systemic lupus erythematosus. Clin Exp Immunol 1977;28:426-32. 162.Coremans IE, Spronk PE, Bootsma H, et al. Changes in antibodies to C1q predict renal relapses in systemic lupus erythematosus. Am J Kidney Dis 1995;26:595-601. 163.Fang QY, Yu F, Tan Y, et al. Anti-C1q antibodies and IgG subclass distribution in sera from Chinese patients with lupus nephritis. Nephrol Dial Transplant 2009;24:172-8. 164.Siegert CE, Daha MR, Tseng CM, Coremans IE, van Es LA, Breedveld FC. Predictive value of IgG autoantibodies against C1q for nephritis in systemic lupus erythematosus. Ann Rheum Dis 1993;52:851-6. 165.Tan Y, Zhou W, Yu F, Fang Q, Yang HZ, Zhao MH. Detection of anti-C1q antibodies and anti-C1q globular head domain antibodies in sera from Chinese patients with lupus nephritis. Mol Immunol 2009;46:2178-82. 166.Trendelenburg M, Lopez-Trascasa M, Potlukova E, et al. High prevalence of anti-C1q antibodies in biopsy-proven active lupus nephritis. Nephrol Dial Transplant 2006. 167.Carvalho JF, Viana VS, Borba EF, et al. High-titer antichromatin antibody is associated with proliferative class IV of lupus nephritis. Clin Rheumatol 2008;27:1417-21. 168.de Macedo PA, Borba EF, Viana Vdos S, et al. Antibodies to ribosomal P proteins in lupus nephritis: a surrogate marker for a better renal survival? Autoimmun Rev 2011;10:126-30. 169.Field M, Williams DG, Charles P, Maini RN. Specificity of anti-Sm antibodies by ELISA for systemic lupus erythematosus: increased sensitivity of detection using purified peptide antigens. Ann Rheum Dis 1988;47:820-5. 170.Venables PJ, Yi T, Woodrow DF, Moss J, Maini RN. Relationship of precipitating antibodies to soluble cellular antigens and histologically defined renal lesions in systemic lupus erythematosus. Ann Rheum Dis 1983;42:17-22. 171.Winn DM, Wolfe JF, Lindberg DA, Fristoe FH, Kingsland L, Sharp GC. Identification of a clinical subset of systemic lupus erythematosus by antibodies to the SM antigen. Arthritis Rheum 1979;22:1334-7. 172.Al-Maini MH, El-Ageb EM, Al-Wahaibi SS, Al-Farsi Y, Richens ER. Demographic, autoimmune, and clinical profiles of patients with systemic lupus erythematosus in Oman. Rheumatol Int 2003;23:186-91. 173.Chin HJ, Ahn C, Lim CS, et al. Clinical implications of antineutrophil cytoplasmic antibody test in lupus nephritis. Am J Nephrol 2000;20:57-63. 174.Zhao MH, Liu N, Zhang YK, Wang HY. Antineutrophil cytoplasmic autoantibodies (ANCA) and their target antigens in Chinese patients with lupus nephritis. Nephrol Dial Transplant 1998;13:2821-4. 175.Chan TM, Cheng IK. A prospective study on anti-endothelial cell antibodies in patients with systemic lupus erythematosus. Clin Immunol Immunopathol 1996;78:41-6. 176.Wang MX, Walker RG, Kincaid-Smith P. Clinicopathologic associations of anti-endothelial cell antibodies in immunoglobulin A nephropathy and lupus nephritis. Am J Kidney Dis 1993;22:378-86. 177.Sjowall C, Zickert A, Skogh T, Wettero J, Gunnarsson I. Serum levels of autoantibodies against C-reactive protein correlate with renal disease activity and response to therapy in lupus nephritis. Arthritis Res Ther 2009;11:R188. 178.Tan Y, Yu F, Yang H, Chen M, Fang Q, Zhao MH. Autoantibodies against monomeric C-reactive protein in sera from patients with lupus nephritis are associated with disease activity and renal tubulointerstitial lesions. Hum Immunol 2008;69:840-4. 179.Ikeda Y, Fujimoto T, Ameno M, Shiiki H, Dohi K. Relationship between lupus nephritis activity and the serum level of soluble VCAM-1. Lupus 1998;7:347-54. 180.Al-Maini MH, Mountz JD, Al-Mohri HA, et al. Serum levels of soluble Fas correlate with indices of organ damage in systemic lupus erythematosus. Lupus 2000;9:132-9. 181.Bond RE, Donadio JV, Jr., Holley KE, Bowie EJ. Fibrinolytic split products. A clinicopathological correlative study in adults with lupus glomerulonephritis and various renal diseases. Arch Intern Med 1973;132:182-7. 182.Chen D, Hsieh C, Chen K, Chen Y, Lin F, Lan J. Association of interleukin-18 promoter polymorphisms with WHO pathological classes and serum IL-18 levels in Chinese patients with lupus nephritis. Lupus 2009;18:29-37. 183.Oates JC, Shaftman SR, Self SE, Gilkeson GS. Association of serum nitrate and nitrite levels with longitudinal assessments of disease activity and damage in systemic lupus erythematosus and lupus nephritis. Arthritis Rheum 2008;58:263-72. 31 184.Masutani K, Akahoshi M, Tsuruya K, et al. Predominance of Th1 immune response in diffuse proliferative lupus nephritis. Arthritis Rheum 2001;44:2097-106. 185.Tucci M, Lombardi L, Richards HB, Dammacco F, Silvestris F. Overexpression of interleukin-12 and T helper 1 predominance in lupus nephritis. Clin Exp Immunol 2008;154:247-54. 186.Laut J, Senitzer D, Petrucci R, Sablay LB, Barland P, Glicklich D. Soluble interleukin-2 receptor levels in lupus nephritis. Clin Nephrol 1992;38:179-84. 187.Iwano M, Dohi K, Hirata E, et al. Urinary levels of IL-6 in patients with active lupus nephritis. Clin Nephrol 1993;40:16-21. 188.Chan RW, Lai FM, Li EK, et al. Expression of chemokine and fibrosing factor messenger RNA in the urinary sediment of patients with lupus nephritis. Arthritis Rheum 2004;50:2882-90. 189.Chan RW, Lai FM, Li EK, et al. Intrarenal cytokine gene expression in lupus nephritis. Ann Rheum Dis 2007;66:886-92. 190.Rovin BH, Song H, Birmingham DJ, Hebert LA, Yu CY, Nagaraja HN. Urine chemokines as biomarkers of human systemic lupus erythematosus activity. J Am Soc Nephrol 2005;16:467-73. 191.Wada T, Yokoyama H, Su SB, et al. Monitoring urinary levels of monocyte chemotactic and activating factor reflects disease activity of lupus nephritis. Kidney Int 1996;49:761-7. 192.Chan RW, Lai FM, Li EK, et al. Imbalance of Th1/Th2 transcription factors in patients with lupus nephritis. Rheumatology (Oxford) 2006;45:951-7. 193.Chan RW, Lai FM, Li EK, et al. Messenger RNA expression of RANTES in the urinary sediment of patients with lupus nephritis. Nephrology (Carlton) 2006;11:219-25. 194.Oates JC, Varghese S, Bland AM, et al. Prediction of urinary protein markers in lupus nephritis. Kidney Int 2005;68:2588-92. 195.Uhm WS, Na K, Song GW, et al. Cytokine balance in kidney tissue from lupus nephritis patients. Rheumatology (Oxford) 2003;42:935-8. 196.Tam LS, Li EK, Lai FM, Chan YK, Szeto CC. Mesangial lupus nephritis in Chinese is associated with a high rate of transformation to higher grade nephritis. Lupus 2003;12:665-71. 197.Shelp WD, Bloodworth JM, Jr., Rieselbach RE. Effect of azathioprine on renal histology and function in lupus nephritis. Arch Intern Med 1971;128:566-73. 198.Faedda R, Palomba D, Satta A, Pirisi M, Tanda F, Bartoli E. Immunosuppressive treatment of the glomerulonephritis of systemic lupus. Clin Nephrol 1995;44:367-75. 199.Laskari K, Tzioufas AG, Antoniou A, Moutsopoulos HM. Longterm followup after tapering mycophenolate mofetil during maintenance treatment for proliferative lupus nephritis. J Rheumatol 2011;38:1304-8. 200.Mok CC, Cheung TT, Lo WH. Minimal mesangial lupus nephritis: a systematic review. Scand J Rheumatol 2010;39:181-9. 201.Felson DT, Anderson J. Evidence for the superiority of immunosuppressive drugs and prednisone over prednisone alone in lupus nephritis. Results of a pooled analysis. N Engl J Med 1984;311:1528-33. 202.Flanc RS, Roberts MA, Strippoli GF, Chadban SJ, Kerr PG, Atkins RC. Treatment for lupus nephritis. Cochrane Database Syst Rev 2004:CD002922. 203.Flanc RS, Roberts MA, Strippoli GF, Chadban SJ, Kerr PG, Atkins RC. Treatment of diffuse proliferative lupus nephritis: a meta-analysis of randomized controlled trials. Am J Kidney Dis 2004;43:197-208. 204.Bansal VK, Beto JA. Treatment of lupus nephritis: a meta-analysis of clinical trials. Am J Kidney Dis 1997;29:193-9. 205.Cade R, Spooner G, Schlein E, et al. Comparison of azathioprine, prednisone, and heparin alone or combined in treating lupus nephritis. Nephron 1973;10:37-56. 206.Decker JL, Klippel JH, Plotz PH, Steinberg AD. Cyclophosphamide or azathioprine in lupus glomerulonephritis. A controlled trial: results at 28 months. Ann Intern Med 1975;83:606-15. 207.Donadio JV, Jr., Holley KE, Ferguson RH, Ilstrup DM. Treatment of diffuse proliferative lupus nephritis with prednisone and combined prednisone and cyclophosphamide. N Engl J Med 1978;299:1151-5. 208.Illei GG, Austin HA, Crane M, et al. Combination therapy with pulse cyclophosphamide plus pulse methylprednisolone improves long-term renal outcome without adding toxicity in patients with lupus nephritis. Ann Intern Med 2001;135:248-57. 209.Steinberg AD, Steinberg SC. Long-term preservation of renal function in patients with lupus nephritis receiving treatment that includes cyclophosphamide versus those treated with prednisone only. Arthritis Rheum 1991;34:945-50. 210.Austin HA, 3rd, Klippel JH, Balow JE, et al. Therapy of lupus nephritis. Controlled trial of prednisone and cytotoxic drugs. N Engl J Med 1986;314:614-9. 211.Balow JE, Austin HA, 3rd, Muenz LR, et al. Effect of treatment on the evolution of renal abnormalities in lupus nephritis. N Engl J Med 1984;311:491-5. 32 212.Gourley MF, Austin HA, 3rd, Scott D, et al. Methylprednisolone and cyclophosphamide, alone or in combination, in patients with lupus nephritis. A randomized, controlled trial. Ann Intern Med 1996;125:549-57. 213.Hahn BH, Kantor OS, Osterland CK. Azathioprine plus prednisone compared with prednisone alone in the treatment of systemic lupus erythematosus. Report of a prospective controlled trial in 24 patients. Ann Intern Med 1975;83:597-605. 214.Sesso R, Monteiro M, Sato E, Kirsztajn G, Silva L, Ajzen H. A controlled trial of pulse cyclophosphamide versus pulse methylprednisolone in severe lupus nephritis. Lupus 1994;3:107-12. 215.Steinberg AD, Kaltreider HB, Staples PJ, Goetzl EJ, Talal N, Decker JL. Cyclophosphamide in lupus nephritis: a controlled trial. Ann Intern Med 1971;75:165-71. 216.Williams W, Bhagwandass A, Sargeant LA, Shah D. Severity of systemic lupus erythematosus with diffuse proliferative glomerulonephritis and the ineffectiveness of standard pulse intravenous cyclophosphamide therapy in Jamaican patients. Lupus 2003;12:640-5. 217.Ginzler E, Sharon E, Diamond H, Kaplan D. Long-term maintenance therapy with azathioprine in systemic lupus erythematosus. Arthritis Rheum 1975;18:27-34. 218.Austin HA, 3rd, Illei GG, Braun MJ, Balow JE. Randomized, controlled trial of prednisone, cyclophosphamide, and cyclosporine in lupus membranous nephropathy. J Am Soc Nephrol 2009;20:901-11. 219.Moroni G, Maccario M, Banfi G, Quaglini S, Ponticelli C. Treatment of membranous lupus nephritis. Am J Kidney Dis 1998;31:681-6. 220.Bitencourt Dias C, Pinheiro CC, Malafronte P, et al. Prednisone monotherapy induced remission in a group of patients with membranous lupus nephritis. Clin Nephrol 2011;76:57-63. 221.Mok CC, Ying KY, Yim CW, Ng WL, Wong WS. Very long-term outcome of pure lupus membranous nephropathy treated with glucocorticoid and azathioprine. Lupus 2009;18:1091-5. 222.Chan TM, Li FK, Hao WK, et al. Treatment of membranous lupus nephritis with nephrotic syndrome by sequential immunosuppression. Lupus 1999;8:545-51. 223.Mok CC, Ying KY, Lau CS, et al. Treatment of pure membranous lupus nephropathy with prednisone and azathioprine: an open-label trial. Am J Kidney Dis 2004;43:269-76. 224.Kasitanon N, Petri M, Haas M, Magder LS, Fine DM. Mycophenolate mofetil as the primary treatment of membranous lupus nephritis with and without concurrent proliferative disease: a retrospective study of 29 cases. Lupus 2008;17:40-5. 225.Spetie DN, Tang Y, Rovin BH, et al. Mycophenolate therapy of SLE membranous nephropathy. Kidney Int 2004;66:2411-5. 226.Hallegua D, Wallace DJ, Metzger AL, Rinaldi RZ, Klinenberg JR. Cyclosporine for lupus membranous nephritis: experience with ten patients and review of the literature. Lupus 2000;9:241-51. 227.Radhakrishnan J, Kunis CL, D'Agati V, Appel GB. Cyclosporine treatment of lupus membranous nephropathy. Clin Nephrol 1994;42:147-54. 228.Tam LS, Li EK, Szeto CC, et al. Treatment of membranous lupus nephritis with prednisone, azathioprine and cyclosporin A. Lupus 2001;10:827-9. 229.Dinant HJ, Decker JL, Klippel JH, Balow JE, Plotz PH, Steinberg AD. Alternative modes of cyclophosphamide and azathioprine therapy in lupus nephritis. Ann Intern Med 1982;96:728-36. 230.Harisdangkul V, Rockhold L, Myers A. Lupus nephritis: efficacy of monthly pulse therapy with intravenous methylprednisolone. South Med J 1989;82:321-7. 231.Makino H, Yamasaki Y, Shikata K, et al. Transition of morphologic features in lupus nephritis: does steroid therapy accelerate glomerulosclerosis? Intern Med 1995;34:982-7. 232.Cathcart ES, Idelson BA, Scheinberg MA, Couser WG. Beneficial effects of methylprednisolone "pulse" therapy in diffuse proliferative lupus nephritis. Lancet 1976;1:163-6. 233.Badsha H, Edwards CJ. Intravenous pulses of methylprednisolone for systemic lupus erythematosus. Semin Arthritis Rheum 2003;32:370-7. 234.Bertoni M, Brugnolo F, Bertoni E, Salvadori M, Romagnani S, Emmi L. Long term efficacy of high-dose intravenous methylprednisolone pulses in active lupus nephritis. A 21month prospective study. Scand J Rheumatol 1994;23:82-6. 235.Kimberly RP, Lockshin MD, Sherman RL, McDougal JS, Inman RD, Christian CL. High-dose intravenous methylprednisolone pulse therapy in systemic lupus erythematosus. Am J Med 1981;70:817-24. 236.Ponticelli C, Moroni G, Banfi G. Treatment of diffuse proliferative lupus nephritis. Contrib Nephrol 1992;99:55-9. 237.Tang Z, Wang Z, Zhang HT, et al. Clinical features and renal outcome in lupus patients with diffuse crescentic glomerulonephritis. Rheumatol Int 2009;30:45-9. 238.Yeung CK, Ng WL, Wong WS, Wong KL, Chan MK. Acute deterioration in renal function in systemic lupus erythematosus. Q J Med 1985;56:393-402. 239.Belmont HM, Storch M, Buyon J, Abramson S. New York University/Hospital for Joint Diseases experience with intravenous cyclophosphamide treatment: efficacy in steroid unresponsive lupus nephritis. Lupus 1995;4:104-8. 33 240.Calguneri M, Ozbalkan Z, Ozturk MA, Apras S, Ertenli AI, Kiraz S. Intensified, intermittent, low-dose intravenous cyclophosphamide together with oral alternate-day steroid therapy in lupus nephritis (long-term outcome). Clin Rheumatol 2006. 241.Laskari K, Mavragani CP, Tzioufas AG, Moutsopoulos HM. Mycophenolate mofetil as maintenance therapy for proliferative lupus nephritis: a long-term observational prospective study. Arthritis Res Ther 2010;12:R208. 242.McKinley A, Park E, Spetie D, et al. Oral cyclophosphamide for lupus glomerulonephritis: an underused therapeutic option. Clin J Am Soc Nephrol 2009;4:1754-60. 243.Mosca M, Neri R, Giannessi S, et al. Therapy with pulse methylprednisolone and short course pulse cyclophosphamide for diffuse proliferative glomerulonephritis. Lupus 2001;10:253-7. 244.Valeri A, Radhakrishnan J, Estes D, et al. Intravenous pulse cyclophosphamide treatment of severe lupus nephritis: a prospective five-year study. Clin Nephrol 1994;42:71-8. 245.Boumpas DT, Austin HA, 3rd, Vaughn EM, et al. Controlled trial of pulse methylprednisolone versus two regimens of pulse cyclophosphamide in severe lupus nephritis. Lancet 1992;340:741-5. 246.Sumethkul V, Chalermsanyakorn P, Changsirikulchai S, Radinahamed P. Lupus nephritis: a challenging cause of rapidly progressive crescentic glomerulonephritis. Lupus 2000;9:424-8. 247.Mok CC, Ho CT, Siu YP, et al. Treatment of diffuse proliferative lupus glomerulonephritis: a comparison of two cyclophosphamide-containing regimens. Am J Kidney Dis 2001;38:256-64. 248.Nasr SH, D'Agati VD, Park HR, et al. Necrotizing and crescentic lupus nephritis with antineutrophil cytoplasmic antibody seropositivity. Clin J Am Soc Nephrol 2008;3:682-90. 249.Chan TM, Li FK, Wong RW, Wong KL, Chan KW, Cheng IK. Sequential therapy for diffuse proliferative and membranous lupus nephritis: cyclophosphamide and prednisolone followed by azathioprine and prednisolone. Nephron 1995;71:321-7. 250.Houssiau FA, D'Cruz DP, Haga HJ, Hughes GR. Short course of weekly low-dose intravenous pulse cyclophosphamide in the treatment of lupus nephritis: a preliminary study. Lupus 1991;1:31-5. 251.Rabrenovic V, Poskurica M, Kovacevic Z, et al. Treatment of lupus nephritis by mycophenolate mofetil. Kidney Blood Press Res 2010;33:297-303. 252.Martinelli R, Pereira LJ, Santos ES, Rocha H. Clinical effects of intermittent, intravenous cyclophosphamide in severe systemic lupus erythematosus. Nephron 1996;74:313-7. 253.McCune WJ, Golbus J, Zeldes W, Bohlke P, Dunne R, Fox DA. Clinical and immunologic effects of monthly administration of intravenous cyclophosphamide in severe systemic lupus erythematosus. N Engl J Med 1988;318:1423-31. 254.Yee CS, Gordon C, Dostal C, et al. EULAR randomised controlled trial of pulse cyclophosphamide and methylprednisolone versus continuous cyclophosphamide and prednisolone followed by azathioprine and prednisolone in lupus nephritis. Ann Rheum Dis 2004;63:525-9. 255.Siso A, Ramos-Casals M, Bove A, et al. Outcomes in biopsy-proven lupus nephritis: evaluation of 190 white patients from a single center. Medicine (Baltimore) 2010;89:300-7. 256.Lee YH, Woo JH, Choi SJ, Ji JD, Song GG. Induction and maintenance therapy for lupus nephritis: a systematic review and meta-analysis. Lupus 2010;19:703-10. 257.Houssiau FA, Vasconcelos C, D'Cruz D, et al. The 10-year follow-up data of the Euro-Lupus Nephritis Trial comparing low-dose and high-dose intravenous cyclophosphamide. Ann Rheum Dis 2010;69:61-4. 258.Houssiau FA, Vasconcelos C, D'Cruz D, et al. Early response to immunosuppressive therapy predicts good renal outcome in lupus nephritis: lessons from long-term followup of patients in the Euro-Lupus Nephritis Trial. Arthritis Rheum 2004;50:3934-40. 259.Houssiau FA, Vasconcelos C, D'Cruz D, et al. Immunosuppressive therapy in lupus nephritis: the Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum 2002;46:2121-31. 260.Petri M, Brodsky RA, Jones RJ, Gladstone D, Fillius M, Magder LS. High-dose cyclophosphamide versus monthly intravenous cyclophosphamide for systemic lupus erythematosus: a prospective randomized trial. Arthritis Rheum 2010;62:1487-93. 261.Sabry A, Abo-Zenah H, Medhat T, Sheashaa H, Mahmoud K, El-Huseini A. A comparative study of two intensified pulse cyclophosphamide remission-inducing regimens for diffuse proliferative lupus nephritis: an Egyptian experience. Int Urol Nephrol 2009;41:153-61. 262.D'Cruz D, Cuadrado MJ, Mujic F, et al. Immunosuppressive therapy in lupus nephritis. Clin Exp Rheumatol 1997;15:275-82. 263.Martin-Suarez I, D'Cruz D, Mansoor M, Fernandes AP, Khamashta MA, Hughes GR. Immunosuppressive treatment in severe connective tissue diseases: effects of low dose intravenous cyclophosphamide. Ann Rheum Dis 1997;56:481-7. 34 264.Seong SS, Choi CB, Yun HR, Kim YJ, Sung YK, Bae SC. Effect of lower dose intravenous cyclophosphamide on remission induction in Korean patients with lupus nephritis. Rheumatol Int 2008;28:453-8. 265.Boumpas DT, Austin HA, 3rd, Vaughan EM, Yarboro CH, Klippel JH, Balow JE. Risk for sustained amenorrhea in patients with systemic lupus erythematosus receiving intermittent pulse cyclophosphamide therapy. Ann Intern Med 1993;119:366-9. 266.Ioannidis JP, Katsifis GE, Tzioufas AG, Moutsopoulos HM. Predictors of sustained amenorrhea from pulsed intravenous cyclophosphamide in premenopausal women with systemic lupus erythematosus. J Rheumatol 2002;29:2129-35. 267.Laskari K, Zintzaras E, Tzioufas AG. Ovarian function is preserved in women with severe systemic lupus erythematosus after a 6-month course of cyclophosphamide followed by mycophenolate mofetil. Clin Exp Rheumatol 2010;28:83-6. 268.Ginzler E, Diamond H, Guttadauria M, Kaplan D. Prednisone and azathioprine compared to prednisone plus low-dose azathioprine and cyclophosphamide in the treatment of diffuse lupus nephritis. Arthritis Rheum 1976;19:693-9. 269.Steinberg AD, Decker JL. A double-blind controlled trial comparing cyclophosphamide, azathioprine and placebo in the treatment of lupus glomerulonephritis. Arthritis Rheum 1974;17:923-37. 270.Donadio JV, Jr., Holley KE, Wagoner RD, Ferguson RH, McDuffie FC. Treatment of lupus nephritis with prednisone and combined prednisone and azathioprine. Ann Intern Med 1972;77:829-35. 271.Donadio JV, Jr., Holley KE, Wagoner RD, Ferguson RH, McDuffie FC. Further observations on the treatment of lupus nephritis with prednisone and combined prednisone and azathioprine. Arthritis Rheum 1974;17:573-81. 272.Grootscholten C, Ligtenberg G, Hagen EC, et al. Azathioprine/methylprednisolone versus cyclophosphamide in proliferative lupus nephritis. A randomized controlled trial. Kidney Int 2006;70:732-42. 273.Arends S, Grootscholten C, Derksen RH, et al. Long-term follow-up of a randomised controlled trial of azathioprine/methylprednisolone versus cyclophosphamide in patients with proliferative lupus nephritis. Ann Rheum Dis 2011. 274.Sabbour MS, Osman LM. Comparison of chlorambucil, azathioprine or cyclophosphamide combined with corticosteroids in the treatment of lupus nephritis. Br J Dermatol 1979;100:113-25. 275.de Glas-Vos JW, Krediet RT, Weening JJ, Arisz L. Treatment of proliferative lupus nephritis with methylprednisolone pulse therapy and oral azathioprine. Neth J Med 1995;46:4-14. 276.Urowitz MB, Ibanez D, Ali Y, Gladman DD. Outcomes in patients with active lupus nephritis requiring immunosuppressives who never received cyclophosphamide. J Rheumatol 2007;34:1491-6. 277.Bono L, Cameron JS, Hicks JA. The very long-term prognosis and complications of lupus nephritis and its treatment. Qjm 1999;92:211-8. 278.Nossent HC, Koldingsnes W. Long-term efficacy of azathioprine treatment for proliferative lupus nephritis. Rheumatology (Oxford) 2000;39:969-74. 279.Drinkard JP, Stanley TM, Dornfeld L, et al. Azathioprine and prednisone in the treatment of adults with lupus nephritis. Clinical, histological, and immunological changes with therapy. Medicine (Baltimore) 1970;49:411-32. 280.Hayslett JP, Kashgarian M, Cook CD, Spargo BH. The effect of azathioprine on lupus glomerulonephritis. Medicine (Baltimore) 1972;51:393-412. 281.Maher JF, Schreiner GE. Treatment of lupus nephritis with azathioprine. Arch Intern Med 1970;125:293-8. 282.Barnett EV, Dornfeld L, Lee DB, Liebling MR. Longterm survival of lupus nephritis patients treated with azathioprine and prednisone. J Rheumatol 1978;5:275-87. 283.Kamanamool N, McEvoy M, Attia J, Ingsathit A, Ngamjanyaporn P, Thakkinstian A. Efficacy and adverse events of mycophenolate mofetil versus cyclophosphamide for induction therapy of lupus nephritis: systematic review and meta-analysis. Medicine (Baltimore) 2010;89:227-35. 284.Mak A, Cheak AA, Tan JY, Su HC, Ho RC, Lau CS. Mycophenolate mofetil is as efficacious as, but safer than, cyclophosphamide in the treatment of proliferative lupus nephritis: a meta-analysis and meta-regression. Rheumatology (Oxford) 2009;48:944-52. 285.Moore RA, Derry S. Systematic review and meta-analysis of randomised trials and cohort studies of mycophenolate mofetil in lupus nephritis. Arthritis Res Ther 2006;8:R182. 286.Touma Z, Gladman DD, Urowitz MB, Beyene J, Uleryk EM, Shah PS. Mycophenolate mofetil for induction treatment of lupus nephritis: a systematic review and metaanalysis. J Rheumatol 2011;38:69-78. 35 287.Walsh M, James M, Jayne D, Tonelli M, Manns BJ, Hemmelgarn BR. Mycophenolate mofetil for induction therapy of lupus nephritis: a systematic review and meta-analysis. Clin J Am Soc Nephrol 2007;2:968-75. 288.Zhu B, Chen N, Lin Y, et al. Mycophenolate mofetil in induction and maintenance therapy of severe lupus nephritis: a meta-analysis of randomized controlled trials. Nephrol Dial Transplant 2007;22:1933-42. 289.Mohan S, Radhakrishnan J. Geographical variation in the response of lupus nephritis to mycophenolate mofetil induction therapy. Clin Nephrol 2011;75:233-41. 290.Chan TM, Li FK, Tang CS, et al. Efficacy of mycophenolate mofetil in patients with diffuse proliferative lupus nephritis. Hong Kong-Guangzhou Nephrology Study Group. N Engl J Med 2000;343:1156-62. 291.Chan TM, Tse KC, Tang CS, Mok MY, Li FK. Long-term study of mycophenolate mofetil as continuous induction and maintenance treatment for diffuse proliferative lupus nephritis. J Am Soc Nephrol 2005;16:1076-84. 292.El-Shafey EM, Abdou SH, Shareef MM. Is mycophenolate mofetil superior to pulse intravenous cyclophosphamide for induction therapy of proliferative lupus nephritis in Egyptian patients? Clin Exp Nephrol 2010;14:214-21. 293.Ginzler EM, Dooley MA, Aranow C, et al. Mycophenolate mofetil or intravenous cyclophosphamide for lupus nephritis. N Engl J Med 2005;353:2219-28. 294.Ong LM, Hooi LS, Lim TO, et al. Randomized controlled trial of pulse intravenous cyclophosphamide versus mycophenolate mofetil in the induction therapy of proliferative lupus nephritis. Nephrology (Carlton) 2005;10:504-10. 295.Appel GB, Contreras G, Dooley MA, et al. Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol 2009;20:1103-12. 296.Isenberg D, Appel GB, Contreras G, et al. Influence of race/ethnicity on response to lupus nephritis treatment: the ALMS study. Rheumatology (Oxford) 2010;49:128-40. 297.Rivera TL, Belmont HM, Malani S, et al. Current therapies for lupus nephritis in an ethnically heterogeneous cohort. J Rheumatol 2009;36:298-305. 298.Kasitanon N, Fine DM, Haas M, Magder LS, Petri M. Hydroxychloroquine use predicts complete renal remission within 12 months among patients treated with mycophenolate mofetil therapy for membranous lupus nephritis. Lupus 2006;15:366-70. 299.Cross J, Dwomoa A, Andrews P, et al. Mycophenolate mofetil for remission induction in severe lupus nephritis. Nephron Clin Pract 2005;100:c92-100. 300.Ding L, Zhao M, Zou W, Liu Y, Wang H. Mycophenolate mofetil combined with prednisone for diffuse proliferative lupus nephritis: a histopathological study. Lupus 2004;13:113-8. 301.Paydas S, Kurt C, Taskapan H, Balal M, Sertdemir Y, Pembegul I. The effect of mycophenolate mofetil on primary and secondary treatment of primary glomerulonephritis and lupus nephritis. Int Urol Nephrol 2009;41:145-52. 302.Pisoni CN, Karim Y, Cuadrado MJ. Mycophenolate mofetil and systemic lupus erythematosus: an overview. Lupus 2005;14 Suppl 1:s9-11. 303.Zeher M, Doria A, Lan J, et al. Efficacy and safety of enteric-coated mycophenolate sodium in combination with two glucocorticoid regimens for the treatment of active lupus nephritis. Lupus 2011;20:1484-93. 304.Traitanon O, Avihingsanon Y, Kittikovit V, et al. Efficacy of enteric-coated mycophenolate sodium in patients with resistant-type lupus nephritis: a prospective study. Lupus 2008;17:744-51. 305.Mak SK, Lo KY, Lo MW, et al. Efficacy of enteric-coated mycophenolate sodium in patients with active lupus nephritis. Nephrology (Carlton) 2008;13:331-6. 306.Kitiyakara C, Ophascharoensuk V, Changsirikulchai S, et al. Treatment of lupus nephritis and primary glomerulonephritis with enteric-coated mycophenolate sodium. Clin Nephrol 2008;69:90-101. 307.Wang J, Hu W, Xie H, et al. Induction therapies for class IV lupus nephritis with non-inflammatory necrotizing vasculopathy: mycophenolate mofetil or intravenous cyclophosphamide. Lupus 2007;16:707-12. 308.Tang Z, Yang G, Yu C, et al. Effects of mycophenolate mofetil for patients with crescentic lupus nephritis. Nephrology (Carlton) 2008;13:702-7. 309.Zavada J, Pesickova S, Rysava R, et al. Cyclosporine A or intravenous cyclophosphamide for lupus nephritis: the Cyclofa-Lune study. Lupus 2010;19:1281-9. 310.Dostal C, Tesar V, Rychlik I, et al. Effect of 1 year cyclosporine A treatment on the activity and renal involvement of systemic lupus erythematosus: a pilot study. Lupus 1998;7:29-36. 311.Manger K, Kalden JR, Manger B. Cyclosporin A in the treatment of systemic lupus erythematosus: results of an open clinical study. Br J Rheumatol 1996;35:669-75. 312.Tam LS, Li EK, Leung CB, et al. Long-term treatment of lupus nephritis with cyclosporin A. Qjm 1998;91:573-80. 36 313.Chen W, Tang X, Liu Q, et al. Short-term outcomes of induction therapy with tacrolimus versus cyclophosphamide for active lupus nephritis: A multicenter randomized clinical trial. Am J Kidney Dis 2011;57:235-44. 314.Miyasaka N, Kawai S, Hashimoto H. Efficacy and safety of tacrolimus for lupus nephritis: a placebo-controlled double-blind multicenter study. Mod Rheumatol 2009;19:60615. 315.Asamiya Y, Uchida K, Otsubo S, Takei T, Nitta K. Clinical assessment of tacrolimus therapy in lupus nephritis: one-year follow-up study in a single center. Nephron Clin Pract 2009;113:c330-6. 316.Mok CC, Tong KH, To CH, Siu YP, Au TC. Tacrolimus for induction therapy of diffuse proliferative lupus nephritis: an open-labeled pilot study. Kidney Int 2005;68:813-7. 317.Takahashi S, Hiromura K, Sakurai N, et al. Efficacy and safety of tacrolimus for induction therapy in patients with active lupus nephritis. Mod Rheumatol 2011;21:282-9. 318.Tse KC, Lam MF, Tang SC, Tang CS, Chan TM. A pilot study on tacrolimus treatment in membranous or quiescent lupus nephritis with proteinuria resistant to angiotensin inhibition or blockade. Lupus 2007;16:46-51. 319.Uchino A, Tsukamoto H, Nakashima H, et al. Tacrolimus is effective for lupus nephritis patients with persistent proteinuria. Clin Exp Rheumatol 2010;28:6-12. 320.Lee YH, Lee HS, Choi SJ, Dai Ji J, Song GG. Efficacy and safety of tacrolimus therapy for lupus nephritis: a systematic review of clinical trials. Lupus 2011;20:636-40. 321.Clark WF, Cattran DC, Balfe JW, Williams W, Lindsay RM, Linton AL. Chronic plasma exchange in systemic lupus erythematosus nephritis. Proc Eur Dial Transplant Assoc 1983;20:629-35. 322.Clark WF, Lindsay RM, Cattran DC, Chodirker WB, Barnes CC, Linton AL. Monthly plasmapheresis for systemic lupus erythematosus with diffuse proliferative glomerulonephritis: a pilot study. Can Med Assoc J 1981;125:171-4. 323.Lewis EJ, Hunsicker LG, Lan SP, Rohde RD, Lachin JM. A controlled trial of plasmapheresis therapy in severe lupus nephritis. The Lupus Nephritis Collaborative Study Group. N Engl J Med 1992;326:1373-9. 324.Nakamura T, Ushiyama C, Hara M, et al. Comparative effects of plasmapheresis and intravenous cyclophosphamide on urinary podocyte excretion in patients with proliferative Lupus nephritis. Clin Nephrol 2002;57:108-13. 325.Danieli MG, Palmieri C, Salvi A, Refe MC, Strusi AS, Danieli G. Synchronised therapy and high-dose cyclophosphamide in proliferative lupus nephritis. J Clin Apher 2002;17:72-7. 326.Sugimoto K, Yamaji K, Yang KS, Kanai Y, Tsuda H, Hashimoto H. Immunoadsorption plasmapheresis using a phenylalanine column as an effective treatment for lupus nephritis. Ther Apher Dial 2006;10:187-92. 327.Yamaji K, Kim YJ, Tsuda H, Takasaki Y. Long-term clinical outcomes of synchronized therapy with plasmapheresis and intravenous cyclophosphamide pulse therapy in the treatment of steroid-resistant lupus nephritis. Ther Apher Dial 2008;12:298-305. 328.Harada T, Ozono Y, Miyazaki M, et al. Plasmapheresis in the treatment of rapidly progressive glomerulonephritis. Ther Apher 1997;1:366-9. 329.Leaker BR, Becker GJ, Dowling JP, Kincaid-Smith PS. Rapid improvement in severe lupus glomerular lesions following intensive plasma exchange associated with immunosuppression. Clin Nephrol 1986;25:236-44. 330.Tam LS, Li EK, Wong CK, Lam CW, Szeto CC. Double-blind, randomized, placebo-controlled pilot study of leflunomide in systemic lupus erythematosus. Lupus 2004;13:6014. 331.Wang HY, Cui TG, Hou FF, et al. Induction treatment of proliferative lupus nephritis with leflunomide combined with prednisone: a prospective multi-centre observational study. Lupus 2008;17:638-44. 332.Zhang FS, Nie YK, Jin XM, Yu HM, Li YN, Sun Y. The efficacy and safety of leflunomide therapy in lupus nephritis by repeat kidney biopsy. Rheumatol Int 2009;29:1331-5. 333.Snaith ML, Holt JM, Oliver DO, Stephenson A. Successful treatment of patients with systemic lupus erythematosus, including nephritis, using chlorambucil. Ann Rheum Dis 1973;32:279-80. 334.Li EK, Tam LS, Zhu TY, et al. Is combination rituximab with cyclophosphamide better than rituximab alone in the treatment of lupus nephritis? Rheumatology (Oxford) 2009;48:892-8. 335.Rovin BH, Furie R, Latinis K, et al. Efficacy and safety of rituximab in patients with active proliferative lupus nephritis: The lupus nephritis assessment with rituximab (LUNAR) study. Arthritis Rheum 2012. 37 336.Ramos-Casals M, Soto MJ, Cuadrado MJ, Khamashta MA. Rituximab in systemic lupus erythematosus: A systematic review of off-label use in 188 cases. Lupus 2009;18:76776. 337.Ramos-Casals M, Diaz-Lagares C, Soto-Cardenas MJ, et al. Rituximab therapy in lupus nephritis: current clinical evidence. Clin Rev Allergy Immunol 2011;40:159-69. 338.Diaz-Lagares C, Croca S, Sangle S, et al. Efficacy of rituximab in 164 patients with biopsy-proven lupus nephritis: Pooled data from European cohorts. Autoimmun Rev 2012;11:357-64. 339.Petri M. Author's reply. Lancet 2011;377:2080-1. 340.Moroni G, Gallelli B, Quaglini S, et al. Withdrawal of therapy in patients with proliferative lupus nephritis: long-term follow-up. Nephrol Dial Transplant 2006;21:1541-8. 341.Pablos JL, Gutierrez-Millet V, Gomez-Reino JJ. Remission of lupus nephritis with cyclophosphamide and late relapses following therapy withdrawal. Scand J Rheumatol 1994;23:142-4. 342.Boletis JN, Ioannidis JP, Boki KA, Moutsopoulos HM. Intravenous immunoglobulin compared with cyclophosphamide for proliferative lupus nephritis. Lancet 1999;354:56970. 343.Contreras G, Pardo V, Leclercq B, et al. Sequential therapies for proliferative lupus nephritis. N Engl J Med 2004;350:971-80. 344.Dooley MA, Jayne D, Ginzler EM, et al. Mycophenolate versus azathioprine as maintenance therapy for lupus nephritis. N Engl J Med 2011;365:1886-95. 345.Houssiau FA, D'Cruz D, Sangle S, et al. Azathioprine versus mycophenolate mofetil for long-term immunosuppression in lupus nephritis: results from the MAINTAIN Nephritis Trial. Ann Rheum Dis 2010;69:2083-9. 346.Sahin GM, Sahin S, Kiziltas S, Masatlioglu S, Oguz F, Ergin H. Mycophenolate mofetil versus azathioprine in the maintenance therapy of lupus nephritis. Ren Fail 2008;30:865-9. 347.Pisoni CN, Sanchez FJ, Karim Y, et al. Mycophenolate mofetil in systemic lupus erythematosus: efficacy and tolerability in 86 patients. J Rheumatol 2005;32:1047-52. 348.Moroni G, Doria A, Mosca M, et al. A randomized pilot trial comparing cyclosporine and azathioprine for maintenance therapy in diffuse lupus nephritis over four years. Clin J Am Soc Nephrol 2006;1:925-32. 349.Boletis JN, Marinaki S, Skalioti C, Lionaki SS, Iniotaki A, Sfikakis PP. Rituximab and mycophenolate mofetil for relapsing proliferative lupus nephritis: a long-term prospective study. Nephrol Dial Transplant 2009;24:2157-60. 350.Loo CY, Mohamed Said MS, Mohd R, et al. Immunoadsorption and plasmapheresis are equally efficacious as adjunctive therapies for severe lupus nephritis. Transfus Apher Sci 2010;43:335-40. 351.Dooley MA, Cosio FG, Nachman PH, et al. Mycophenolate mofetil therapy in lupus nephritis: clinical observations. J Am Soc Nephrol 1999;10:833-9. 352.Karim MY, Alba P, Cuadrado MJ, et al. Mycophenolate mofetil for systemic lupus erythematosus refractory to other immunosuppressive agents. Rheumatology (Oxford) 2002;41:876-82. 353.Kingdon EJ, McLean AG, Psimenou E, et al. The safety and efficacy of MMF in lupus nephritis: a pilot study. Lupus 2001;10:606-11. 354.Sahin GM, Sahin S, Kantarci G, Ergin H. Mycophenolate mofetil treatment for therapy-resistant glomerulopathies. Nephrology (Carlton) 2007;12:285-8. 355.Weng MY, Weng CT, Liu MF. The efficacy of low-dose mycophenolate mofetil for treatment of lupus nephritis in Taiwanese patients with systemic lupus erythematosus. Clin Rheumatol 2010;29:771-5. 356.Ogawa H, Kameda H, Nagasawa H, et al. Prospective study of low-dose cyclosporine A in patients with refractory lupus nephritis. Mod Rheumatol 2007;17:92-7. 357.Ogawa H, Kameda H, Amano K, Takeuchi T. Efficacy and safety of cyclosporine A in patients with refractory systemic lupus erythematosus in a daily clinical practice. Lupus 2010;19:162-9. 358.Rihova Z, Vankova Z, Maixnerova D, et al. Treatment of lupus nephritis with cyclosporine - an outcome analysis. Kidney Blood Press Res 2007;30:124-8. 359.Cortes-Hernandez J, Torres-Salido MT, Medrano AS, Tarres MV, Ordi-Ros J. Long-term outcomes--mycophenolate mofetil treatment for lupus nephritis with addition of tacrolimus for resistant cases. Nephrol Dial Transplant 2010;25:3939-48. 360.Lanata CM, Mahmood T, Fine DM, Petri M. Combination therapy of mycophenolate mofetil and tacrolimus in lupus nephritis. Lupus 2010;19:935-40. 361.Lee T, Oh KH, Joo KW, et al. Tacrolimus is an alternative therapeutic option for the treatment of refractory lupus nephritis. Lupus 2010;19:974-80. 362.Levy Y, Sherer Y, George J, et al. Intravenous immunoglobulin treatment of lupus nephritis. Semin Arthritis Rheum 2000;29:321-7. 38 363.Monova D, Belovezhdov N, Altunkova I, Monov S. Intravenous immunoglobulin G in the treatment of patients with chronic glomerulonephritis: clinical experience lasting 15 years. Nephron 2002;90:262-6. 364.Wallace DJ. Plasmapheresis for lupus nephritis. N Engl J Med 1992;327:1029: author reply -30. 365.Stummvoll GH, Aringer M, Smolen JS, et al. IgG immunoadsorption reduces systemic lupus erythematosus activity and proteinuria: a long term observational study. Ann Rheum Dis 2005;64:1015-21. 366.Stummvoll GH, Schmaldienst S, Smolen JS, Derfler K, Biesenbach P. Lupus nephritis: prolonged immunoadsorption (IAS) reduces proteinuria and stabilizes global disease activity. Nephrol Dial Transplant 2011. 367.Catapano F, Chaudhry AN, Jones RB, Smith KG, Jayne DW. Long-term efficacy and safety of rituximab in refractory and relapsing systemic lupus erythematosus. Nephrol Dial Transplant 2010;25:3586-92. 368.Pepper R, Griffith M, Kirwan C, et al. Rituximab is an effective treatment for lupus nephritis and allows a reduction in maintenance steroids. Nephrol Dial Transplant 2009;24:3717-23. 369.Sfikakis PP, Boletis JN, Lionaki S, et al. Remission of proliferative lupus nephritis following B cell depletion therapy is preceded by down-regulation of the T cell costimulatory molecule CD40 ligand: an open-label trial. Arthritis Rheum 2005;52:501-13. 370.Terrier B, Amoura Z, Ravaud P, et al. Safety and efficacy of rituximab in systemic lupus erythematosus: results from 136 patients from the French AutoImmunity and Rituximab registry. Arthritis Rheum 2010;62:2458-66. 371.Garcia-Carrasco M, Mendoza-Pinto C, Sandoval-Cruz M, et al. Anti-CD20 therapy in patients with refractory systemic lupus erythematosus: a longitudinal analysis of 52 Hispanic patients. Lupus 2010;19:213-9. 372.Gunnarsson I, Sundelin B, Jonsdottir T, Jacobson SH, Henriksson EW, van Vollenhoven RF. Histopathologic and clinical outcome of rituximab treatment in patients with cyclophosphamide-resistant proliferative lupus nephritis. Arthritis Rheum 2007;56:1263-72. 373.Jonsdottir T, Gunnarsson I, Risselada A, Henriksson EW, Klareskog L, van Vollenhoven RF. Treatment of refractory SLE with rituximab plus cyclophosphamide: clinical effects, serological changes, and predictors of response. Ann Rheum Dis 2008;67:330-4. 374.Jonsdottir T, Gunnarsson I, Mourao AF, Lu TY, van Vollenhoven RF, Isenberg D. Clinical improvements in proliferative vs membranous lupus nephritis following B-cell depletion: pooled data from two cohorts. Rheumatology (Oxford) 2010;49:1502-4. 375.Lateef A, Lahiri M, Teng GG, Vasoo S. Use of rituximab in the treatment of refractory systemic lupus erythematosus: Singapore experience. Lupus 2010;19:765-70. 376.Lindholm C, Borjesson-Asp K, Zendjanchi K, Sundqvist AC, Tarkowski A, Bokarewa M. Longterm clinical and immunological effects of anti-CD20 treatment in patients with refractory systemic lupus erythematosus. J Rheumatol 2008;35:826-33. 377.Melander C, Sallee M, Trolliet P, et al. Rituximab in severe lupus nephritis: early B-cell depletion affects long-term renal outcome. Clin J Am Soc Nephrol 2009;4:579-87. 378.Roccatello D, Sciascia S, Rossi D, et al. Intensive short-term treatment with rituximab, cyclophosphamide and methylprednisolone pulses induces remission in severe cases of SLE with nephritis and avoids further immunosuppressive maintenance therapy. Nephrol Dial Transplant 2011;26:3987-92. 379.Smith KG, Jones RB, Burns SM, Jayne DR. Long-term comparison of rituximab treatment for refractory systemic lupus erythematosus and vasculitis: Remission, relapse, and re-treatment. Arthritis Rheum 2006;54:2970-82. 380.Vigna-Perez M, Hernandez-Castro B, Paredes-Saharopulos O, et al. Clinical and immunological effects of Rituximab in patients with lupus nephritis refractory to conventional therapy: a pilot study. Arthritis Res Ther 2006;8:R83. 381.Burt RK, Traynor A, Statkute L, et al. Nonmyeloablative hematopoietic stem cell transplantation for systemic lupus erythematosus. Jama 2006;295:527-35. 382.Farge D, Labopin M, Tyndall A, et al. Autologous hematopoietic stem cell transplantation for autoimmune diseases: an observational study on 12 years' experience from the European Group for Blood and Marrow Transplantation Working Party on Autoimmune Diseases. Haematologica 2010;95:284-92. 383.Sun L, Wang D, Liang J, et al. Umbilical cord mesenchymal stem cell transplantation in severe and refractory systemic lupus erythematosus. Arthritis Rheum 2010;62:2467-75. 384.Traynor AE, Schroeder J, Rosa RM, et al. Treatment of severe systemic lupus erythematosus with high-dose chemotherapy and haemopoietic stem-cell transplantation: a phase I study. Lancet 2000;356:701-7. 385.Jayne D, Tyndall A. Autologous stem cell transplantation for systemic lupus erythematosus. Lupus 2004;13:359-65. 39 386.Liang J, Zhang H, Hua B, et al. Allogenic mesenchymal stem cells transplantation in refractory systemic lupus erythematosus: a pilot clinical study. Ann Rheum Dis 2010;69:1423-9. 387.Song XN, Lv HY, Sun LX, et al. Autologous stem cell transplantation for systemic lupus erythematosus: report of efficacy and safety at 7 years of follow-up in 17 patients. Transplant Proc 2011;43:1924-7. 388.Petri M, Jones RJ, Brodsky RA. High-dose cyclophosphamide without stem cell transplantation in systemic lupus erythematosus. Arthritis Rheum 2003;48:166-73. 389.Tam LS, Li EK, Wong CK, Lam CW, Li WC, Szeto CC. Safety and efficacy of leflunomide in the treatment of lupus nephritis refractory or intolerant to traditional immunosuppressive therapy: an open label trial. Ann Rheum Dis 2006;65:417-8. 390.Genovese MC, Uhrin Z, Bloch DA, et al. Long-term followup of patients treated with total lymphoid irradiation for lupus nephritis. Arthritis Rheum 2002;46:1014-8. 391.Strober S, Field E, Hoppe RT, et al. Treatment of intractable lupus nephritis with total lymphoid irradiation. Ann Intern Med 1985;102:450-8. 392.Strober S, Farinas MC, Field EH, et al. Lupus nephritis after total lymphoid irradiation: persistent improvement and reduction of steroid therapy. Ann Intern Med 1987;107:68990. 393.Strober S, Farinas MC, Field EH, et al. Treatment of lupus nephritis with total lymphoid irradiation. Observations during a 12-79-month followup. Arthritis Rheum 1988;31:8508. 394.Galindo-Rodriguez G, Bustamante R, Esquivel-Nava G, et al. Pentoxifylline in the treatment of refractory nephrotic syndrome secondary to lupus nephritis. J Rheumatol 2003;30:2382-4. 395.Matsumura R, Umemiya K, Sugiyama T, et al. Anti-tumor necrosis factor therapy in patients with difficult-to-treat lupus nephritis: a prospective series of nine patients. Clin Exp Rheumatol 2009;27:416-21. 396.Radhakrishnan J, Moutzouris DA, Ginzler EM, Solomons N, Siempos, II, Appel GB. Mycophenolate mofetil and intravenous cyclophosphamide are similar as induction therapy for class V lupus nephritis. Kidney Int 2010;77:152-60. 397.Kapitsinou PP, Boletis JN, Skopouli FN, Boki KA, Moutsopoulos HM. Lupus nephritis: treatment with mycophenolate mofetil. Rheumatology (Oxford) 2004;43:377-80. 398.Karim MY, Pisoni CN, Ferro L, et al. Reduction of proteinuria with mycophenolate mofetil in predominantly membranous lupus nephropathy. Rheumatology (Oxford) 2005;44:1317-21. 399.Szeto CC, Kwan BC, Lai FM, et al. Tacrolimus for the treatment of systemic lupus erythematosus with pure class V nephritis. Rheumatology (Oxford) 2008;47:1678-81. 400.Borba EF, Guedes LK, Christmann RB, Figueiredo CP, Goncalves CR, Bonfa E. Mycophenolate mofetil is effective in reducing lupus glomerulonephritis proteinuria. Rheumatol Int 2006. 401.Reich HN, Gladman DD, Urowitz MB, et al. Persistent proteinuria and dyslipidemia increase the risk of progressive chronic kidney disease in lupus erythematosus. Kidney Int 2011;79:914-20. 402.Levey AS, Lan SP, Corwin HL, et al. Progression and remission of renal disease in the Lupus Nephritis Collaborative Study. Results of treatment with prednisone and short-term oral cyclophosphamide. Ann Intern Med 1992;116:114-23. 403.Hill GS, Delahousse M, Nochy D, et al. Outcome of relapse in lupus nephritis: roles of reversal of renal fibrosis and response of inflammation to therapy. Kidney Int 2002;61:2176-86. 404.Mak A, Mok CC, Chu WP, To CH, Wong SN, Au TC. Renal damage in systemic lupus erythematosus: a comparative analysis of different age groups. Lupus 2007;16:28-34. 405.So MW, Koo BS, Kim YG, Lee CK, Yoo B. Predictive value of remission status after 6 months induction therapy in patients with proliferative lupus nephritis: a retrospective analysis. Clin Rheumatol 2011;30:1399-405. 406.Barber CE, Geldenhuys L, Hanly JG. Sustained remission of lupus nephritis. Lupus 2006;15:94-101. 407.Tian S, Li J, Wang L, et al. Urinary levels of RANTES and M-CSF are predictors of lupus nephritis flare. Inflamm Res 2007;56:304-10. 408.Ardoin S, Birmingham DJ, Hebert PL, Yu CY, Rovin BH, Hebert LA. An approach to validating criteria for proteinuric flare in systemic lupus erythematosus glomerulonephritis. Arthritis Rheum 2011;63:2031-7. 409.El Hachmi M, Jadoul M, Lefebvre C, Depresseux G, Houssiau FA. Relapses of lupus nephritis: incidence, risk factors, serology and impact on outcome. Lupus 2003;12:692-6. 410.Daza L, Kornhauser C, Zamora L, Flores J. Captopril effect on prostaglandin E2, thromboxane B2 and proteinuria in lupus nephritis patients. Prostaglandins Other Lipid Mediat 2005;78:194-201. 40 411.Kanda H, Kubo K, Tateishi S, et al. Antiproteinuric effect of ARB in lupus nephritis patients with persistent proteinuria despite immunosuppressive therapy. Lupus 2005;14:288-92. 412.Tse KC, Li FK, Tang S, Tang CS, Lai KN, Chan TM. Angiotensin inhibition or blockade for the treatment of patients with quiescent lupus nephritis and persistent proteinuria. Lupus 2005;14:947-52. 413.Duran-Barragan S, McGwin G, Jr., Vila LM, Reveille JD, Alarcon GS. Angiotensin-converting enzyme inhibitors delay the occurrence of renal involvement and are associated with a decreased risk of disease activity in patients with systemic lupus erythematosus--results from LUMINA (LIX): a multiethnic US cohort. Rheumatology (Oxford) 2008;47:1093-6. 414.Chong YB, Yap DY, Tang CS, Chan TM. Dyslipidaemia in patients with lupus nephritis. Nephrology (Carlton) 2011;16:511-7. 415.Fessler BJ, Alarcon GS, McGwin G, Jr., et al. Systemic lupus erythematosus in three ethnic groups: XVI. Association of hydroxychloroquine use with reduced risk of damage accrual. Arthritis Rheum 2005;52:1473-80. 416.Siso A, Ramos-Casals M, Bove A, et al. Previous antimalarial therapy in patients diagnosed with lupus nephritis: influence on outcomes and survival. Lupus 2008;17:281-8. 417.Tsakonas E, Joseph L, Esdaile JM, et al. A long-term study of hydroxychloroquine withdrawal on exacerbations in systemic lupus erythematosus. The Canadian Hydroxychloroquine Study Group. Lupus 1998;7:80-5. 418.Clark WF, Parbtani A, Huff MW, Reid B, Holub BJ, Falardeau P. Omega-3 fatty acid dietary supplementation in systemic lupus erythematosus. Kidney Int 1989;36:653-60. 419.Clark WF, Parbtani A, Naylor CD, et al. Fish oil in lupus nephritis: clinical findings and methodological implications. Kidney Int 1993;44:75-86. 420.Clark WF, Parbtani A. Omega-3 fatty acid supplementation in clinical and experimental lupus nephritis. Am J Kidney Dis 1994;23:644-7. 421.Clark WF, Kortas C, Heidenheim AP, Garland J, Spanner E, Parbtani A. Flaxseed in lupus nephritis: a two-year nonplacebo-controlled crossover study. J Am Coll Nutr 2001;20:143-8. 422.Mosley K, Tam FW, Edwards RJ, Crozier J, Pusey CD, Lightstone L. Urinary proteomic profiles distinguish between active and inactive lupus nephritis. Rheumatology (Oxford) 2006;45:1497-504. 423.Kasitanon N, Fine DM, Haas M, Magder LS, Petri M. Estimating renal function in lupus nephritis: comparison of the Modification of Diet in Renal Disease and Cockcroft Gault equations. Lupus 2007;16:887-95. 424.Leung YY, Lo KM, Tam LS, Szeto CC, Li EK, Kun EW. Estimation of glomerular filtration rate in patients with systemic lupus erythematosus. Lupus 2006;15:276-81. 425.Martinez-Martinez MU, Borjas-Garcia JA, Magana-Aquino M, Cuevas-Orta E, Llamazares-Azuara L, Abud-Mendoza C. Renal function assessment in patients with systemic lupus erythematosus. Rheumatol Int 2011. 426.Petri M, Bockenstedt L, Colman J, et al. Serial assessment of glomerular filtration rate in lupus nephropathy. Kidney Int 1988;34:832-9. 427.Roubenoff R, Drew H, Moyer M, Petri M, Whiting-O'Keefe Q, Hellmann DB. Oral cimetidine improves the accuracy and precision of creatinine clearance in lupus nephritis. Ann Intern Med 1990;113:501-6. 428.ter Borg EJ, Horst G, Hummel E, Limburg PC, Kallenberg CG. Rises in anti-double stranded DNA antibody levels prior to exacerbations of systemic lupus erythematosus are not merely due to polyclonal B cell activation. Clin Immunol Immunopathol 1991;59:117-28. 429.Colburn KK, Green LM, Wong AK. Circulating antibodies to guanosine in systemic lupus erythematosus: correlation with nephritis and polyserositis by acute and longitudinal analyses. Lupus 2001;10:410-7. 430.Ghirardello A, Villalta D, Morozzi G, et al. Diagnostic accuracy of currently available anti-double-stranded DNA antibody assays. An Italian multicentre study. Clin Exp Rheumatol 2011;29:50-6. 431.Grootscholten C, Dieker JW, McGrath FD, et al. A prospective study of anti-chromatin and anti-C1q autoantibodies in patients with proliferative lupus nephritis treated with cyclophosphamide pulses or azathioprine/methylprednisolone. Ann Rheum Dis 2007;66:693-6. 432.Gutierrez-Adrianzen OA, Koutouzov S, Mota RM, das Chagas Medeiros MM, Bach JF, de Holanda Campos H. Diagnostic value of anti-nucleosome antibodies in the assessment of disease activity of systemic lupus erythematosus: a prospective study comparing anti-nucleosome with anti-dsDNA antibodies. J Rheumatol 2006;33:1538-44. 433.Hanly JG, Thompson K, McCurdy G, Fougere L, Theriault C, Wilton K. Measurement of autoantibodies using multiplex methodology in patients with systemic lupus erythematosus. J Immunol Methods 2010;352:147-52. 41 434.Ho A, Magder LS, Barr SG, Petri M. Decreases in anti-double-stranded DNA levels are associated with concurrent flares in patients with systemic lupus erythematosus. Arthritis Rheum 2001;44:2342-9. 435.Julkunen H, Ekblom-Kullberg S, Miettinen A. Nonrenal and renal activity of systemic lupus erythematosus: a comparison of two anti-C1q and five anti-dsDNA assays and complement C3 and C4. Rheumatol Int 2011. 436.Kiss E, Lakos G, Szegedi G, Poor G, Szodoray P. Anti-nuscleosome antibody, a reliable indicator for lupus nephritis. Autoimmunity 2009;42:393-8. 437.Kramers C, Termaat RM, ter Borg EJ, van Bruggen MC, Kallenberg CG, Berden JH. Higher anti-heparan sulphate reactivity during systemic lupus erythematosus (SLE) disease exacerbations with renal manifestations; a long term prospective analysis. Clin Exp Immunol 1993;93:34-8. 438.Kwan BC, Tam LS, Lai KB, et al. The gene expression of type 17 T-helper cell-related cytokines in the urinary sediment of patients with systemic lupus erythematosus. Rheumatology (Oxford) 2009;48:1491-7. 439.Mok CC, Ho LY, Leung HW, Wong LG. Performance of anti-C1q, antinucleosome, and anti-dsDNA antibodies for detecting concurrent disease activity of systemic lupus erythematosus. Transl Res 2010;156:320-5. 440.Moroni G, Radice A, Giammarresi G, et al. Are laboratory tests useful for monitoring the activity of lupus nephritis? A 6-year prospective study in a cohort of 228 patients with lupus nephritis. Ann Rheum Dis 2009;68:234-7. 441.Mosca M, Chimenti D, Pratesi F, et al. Prevalence and clinico-serological correlations of anti-alpha-enolase, anti-C1q, and anti-dsDNA antibodies in patients with systemic lupus erythematosus. J Rheumatol 2006;33:695-7. 442.Neogi T, Gladman DD, Ibanez D, Urowitz M. Anti-dsDNA Antibody Testing by Farr and ELISA Techniques Is Not Equivalent. J Rheumatol 2006. 443.Pitashny M, Schwartz N, Qing X, et al. Urinary lipocalin-2 is associated with renal disease activity in human lupus nephritis. Arthritis Rheum 2007;56:1894-903. 444.Tsai CY, Wu TH, Yu CL, Lu JY, Tsai YY. Increased excretions of beta2-microglobulin, IL-6, and IL-8 and decreased excretion of Tamm-Horsfall glycoprotein in urine of patients with active lupus nephritis. Nephron 2000;85:207-14. 445.Ballou SP, Kushner I. Anti-native DNA detection by the Crithidia luciliae method: an improved guide to the diagnosis and clinical management of systemic lupus erythematosus. Arthritis Rheum 1979;22:321-7. 446.Ballou SP, Kushner I. Immunochemical characteristics of antibodies to DNA in patients with active systemic lupus erythematosus. Clin Exp Immunol 1979;37:58-67. 447.Helve T, Teppo AM, Kurki P, Wegelius O. Circulating DNA-antibodies in systemic lupus erythematosus. Rheumatol Int 1982;2:103-6. 448.Quintana G, Coral-Alvarado P, Aroca G, et al. Single anti-P ribosomal antibodies are not associated with lupus nephritis in patients suffering from active systemic lupus erythematosus. Autoimmun Rev 2010;9:750-5. 449.Bijl M, Dijstelbloem HM, Oost WW, et al. IgG subclass distribution of autoantibodies differs between renal and extra-renal relapses in patients with systemic lupus erythematosus. Rheumatology (Oxford) 2002;41:62-7. 450.Cameron JS, Lessof MH, Ogg CS, Williams BD, Williams DG. Disease activity in the nephritis of systemic lupus erythematosus in relation to serum complement concentrations. DNA-binding capacity and precipitating anti-DNA antibody. Clin Exp Immunol 1976;25:418-27. 451.Cervera R, Vinas O, Ramos-Casals M, et al. Anti-chromatin antibodies in systemic lupus erythematosus: a useful marker for lupus nephropathy. Ann Rheum Dis 2003;62:431-4. 452.Esdaile JM, Abrahamowicz M, Joseph L, MacKenzie T, Li Y, Danoff D. Laboratory tests as predictors of disease exacerbations in systemic lupus erythematosus. Why some tests fail. Arthritis Rheum 1996;39:370-8. 453.Jaekell HP, Trabandt A, Grobe N, Werle E. Anti-dsDNA antibody subtypes and anti-C1q antibodies: toward a more reliable diagnosis and monitoring of systemic lupus erythematosus and lupus nephritis. Lupus 2006;15:335-45. 454.Manson JJ, Ma A, Rogers P, et al. Relationship between anti-dsDNA, anti-nucleosome and anti-alpha-actinin antibodies and markers of renal disease in patients with lupus nephritis: a prospective longitudinal study. Arthritis Res Ther 2009;11:R154. 455.Matrat A, Veysseyre-Balter C, Trolliet P, et al. Simultaneous detection of anti-C1q and anti-double stranded DNA autoantibodies in lupus nephritis: predictive value for renal flares. Lupus 2011;20:28-34. 456.Renaudineau Y, Croquefer S, Jousse S, et al. Association of alpha-actinin-binding anti-double-stranded DNA antibodies with lupus nephritis. Arthritis Rheum 2006;54:2523-32. 457.Sinico RA, Radice A, Ikehata M, et al. Anti-C1q autoantibodies in lupus nephritis: prevalence and clinical significance. Ann N Y Acad Sci 2005;1050:193-200. 42 458.Swaak AJ, Aarden LA, Statius van Eps LW, Feltkamp TE. Anti-dsDNA and complement profiles as prognostic guides in systemic lupus erythematosus. Arthritis Rheum 1979;22:226-35. 459.Zonana-Nacach A, Salas M, Sanchez ML, Camargo-Coronel A, Bravo-Gatica C, Mintz G. Measurement of clinical activity of systemic lupus erythematosus and laboratory abnormalities: a 12-month prospective study. J Rheumatol 1995;22:45-9. 460.Becker-Merok A, Kalaaji M, Haugbro K, et al. Alpha-actinin-binding antibodies in relation to systemic lupus erythematosus and lupus nephritis. Arthritis Res Ther 2006;8:R162. 461.Schiffer L, Kumpers P, Davalos-Misslitz AM, et al. B-cell-attracting chemokine CXCL13 as a marker of disease activity and renal involvement in systemic lupus erythematosus (SLE). Nephrol Dial Transplant 2009;24:3708-12. 462.Appel AE, Sablay LB, Golden RA, Barland P, Grayzel AI, Bank N. The effect of normalization of serum complement and anti-DNA antibody on the course of lupus nephritis: a two year prospective study. Am J Med 1978;64:274-83. 463.Birmingham DJ, Irshaid F, Nagaraja HN, et al. The complex nature of serum C3 and C4 as biomarkers of lupus renal flare. Lupus 2010;19:1272-80. 464.Dall'era M, Stone D, Levesque V, Cisternas M, Wofsy D. Identification of Biomarkers That Predict Response to Treatment of Lupus Nephritis With Mycophenolate Mofetil or Pulse Cyclophosphamide. Arthritis Care Res 2011;63:351-7. 465.El-Shehaby A, Darweesh H, El-Khatib M, et al. Correlations of urinary biomarkers, TNF-like weak inducer of apoptosis (TWEAK), osteoprotegerin (OPG), monocyte chemoattractant protein-1 (MCP-1), and IL-8 with lupus nephritis. J Clin Immunol 2011;31:848-56. 466.Ho A, Barr SG, Magder LS, Petri M. A decrease in complement is associated with increased renal and hematologic activity in patients with systemic lupus erythematosus. Arthritis Rheum 2001;44:2350-7. 467.Swaak AJ, Groenwold J, Bronsveld W. Predictive value of complement profiles and anti-dsDNA in systemic lupus erythematosus. Ann Rheum Dis 1986;45:359-66. 468.Tanaka H, Akama H, Tominaga N, Oshima H, Ichikawa Y, Ikeda Y. Progressive renal failure in patients with lupus nephritis. J Intern Med 1993;234:257-62. 469.Ricker DM, Hebert LA, Rohde R, Sedmak DD, Lewis EJ, Clough JD. Serum C3 levels are diagnostically more sensitive and specific for systemic lupus erythematosus activity than are serum C4 levels. The Lupus Nephritis Collaborative Study Group. Am J Kidney Dis 1991;18:678-85. 470.Amezcua-Guerra LM, Springall R, Arrieta-Alvarado AA, et al. C-reactive protein and complement components but not other acute-phase reactants discriminate between clinical subsets and organ damage in systemic lupus erythematosus. Clin Lab 2011;57:607-13. 471.Pillemer SR, Austin HA, 3rd, Tsokos GC, Balow JE. Lupus nephritis: association between serology and renal biopsy measures. J Rheumatol 1988;15:284-8. 472.Tikly M, Burgin S, Mohanlal P, Bellingan A, George J. Autoantibodies in black South Africans with systemic lupus erythematosus: spectrum and clinical associations. Clin Rheumatol 1996;15:261-5. 473.Moura CGGd, Mangueira CLP, Cruz LAS, Cruz CMS. Negative Anti-C1q Antibody Titers May Influence Therapeutic Decisions and Reduce the Number of Renal Biopsies in Systemic Lupus Erythematosus. Nephron Clin Pract 2011;118:c355-c60. 474.Horak P, Hermanova Z, Zadrazil J, et al. C1q complement component and -antibodies reflect SLE activity and kidney involvement. Clin Rheumatol 2006;25:532-6. 475.Horvath L, Czirjak L, Fekete B, et al. High levels of antibodies against Clq are associated with disease activity and nephritis but not with other organ manifestations in SLE patients. Clin Exp Rheumatol 2001;19:667-72. 476.Katsumata Y, Miyake K, Kawaguchi Y, et al. Anti-C1q antibodies are associated with systemic lupus erythematosus global activity but not specifically with nephritis: a controlled study of 126 consecutive patients. Arthritis Rheum 2011;63:2436-44. 477.Marto N, Bertolaccini ML, Calabuig E, Hughes GR, Khamashta MA. Anti-C1q antibodies in nephritis: correlation between titres and renal disease activity and positive predictive value in systemic lupus erythematosus. Ann Rheum Dis 2005;64:444-8. 478.Moroni G, Trendelenburg M, Del Papa N, et al. Anti-C1q antibodies may help in diagnosing a renal flare in lupus nephritis. Am J Kidney Dis 2001;37:490-8. 479.Moura CG, Lima I, Barbosa L, et al. Anti-C1q antibodies: association with nephritis and disease activity in systemic lupus erythematosus. J Clin Lab Anal 2009;23:19-23. 480.Trendelenburg M, Marfurt J, Gerber I, Tyndall A, Schifferli JA. Lack of occurrence of severe lupus nephritis among anti-C1q autoantibody-negative patients. Arthritis Rheum 1999;42:187-8. 481.Zhang CQ, Ren L, Gao F, Mu FY, You YQ, Liu YH. Anti-C1q antibodies are associated with systemic lupus erythematosus disease activity and lupus nephritis in northeast of China. Clin Rheumatol 2011;30:967-73. 43 482.Siegert C, Daha M, Westedt ML, van der Voort E, Breedveld F. IgG autoantibodies against C1q are correlated with nephritis, hypocomplementemia, and dsDNA antibodies in systemic lupus erythematosus. J Rheumatol 1991;18:230-4. 483.Simon JA, Cabiedes J, Ortiz E, Alcocer-Varela J, Sanchez-Guerrero J. Anti-nucleosome antibodies in patients with systemic lupus erythematosus of recent onset. Potential utility as a diagnostic tool and disease activity marker. Rheumatology (Oxford) 2004;43:220-4. 484.Souza A, da Silva LM, Oliveira FR, Roselino AM, Louzada-Junior P. Anti-nucleosome and anti-chromatin antibodies are present in active systemic lupus erythematosus but not in the cutaneous form of the disease. Lupus 2009;18:223-9. 485.Chindalore V, Neas B, Reichlin M. The association between anti-ribosomal P antibodies and active nephritis in systemic lupus erythematosus. Clin Immunol Immunopathol 1998;87:292-6. 486.Figueredo MA, Rodriguez A, Ruiz-Yague M, et al. Autoantibodies against C-reactive protein: clinical associations in systemic lupus erythematosus and primary antiphospholipid syndrome. J Rheumatol 2006;33:1980-6. 487.Ravirajan CT, Rowse L, MacGowan JR, Isenberg DA. An analysis of clinical disease activity and nephritis-associated serum autoantibody profiles in patients with systemic lupus erythematosus: a cross-sectional study. Rheumatology (Oxford) 2001;40:1405-12. 488.Tseng JC, Lu LY, Hu RJ, et al. Elevated serum anti-endothelial cell autoantibodies titer is associated with lupus nephritis in patients with systemic lupus erythematosus. J Microbiol Immunol Infect 2007;40:50-5. 489.Hebert LA, Dillon JJ, Middendorf DF, Lewis EJ, Peter JB. Relationship between appearance of urinary red blood cell/white blood cell casts and the onset of renal relapse in systemic lupus erythematosus. Am J Kidney Dis 1995;26:432-8. 490.Roberti I, Dikman S, Spiera H, Reisman L, Eichenfield AH, Lieberman KV. Comparative value of urinalysis, urine cytology and urine sIL2R in the assessment of renal disease in patients with systemic lupus erythematosus (SLE). Clin Nephrol 1996;46:176-82. 491.Birmingham DJ, Rovin BH, Shidham G, et al. Spot urine protein/creatinine ratios are unreliable estimates of 24 h proteinuria in most systemic lupus erythematosus nephritis flares. Kidney Int 2007;72:865-70. 492.Christopher-Stine L, Petri M, Astor BC, Fine D. Urine protein-to-creatinine ratio is a reliable measure of proteinuria in lupus nephritis. J Rheumatol 2004;31:1557-9. 493.Cottiero RA, Madaio MP, Levey AS. Glomerular filtration rate and urinary albumin excretion rate in systemic lupus erythematosus. Nephron 1995;69:140-6. 494.Fine DM, Ziegenbein M, Petri M, et al. A prospective study of protein excretion using short-interval timed urine collections in patients with lupus nephritis. Kidney Int 2009;76:1284-8. 495.Hebert LA, Birmingham DJ, Shidham G, Rovin B, Nagaraja HN, Yu CY. Random spot urine protein/creatinine ratio is unreliable for estimating 24-hour proteinuria in individual systemic lupus erythematosus nephritis patients. Nephron Clin Pract 2009;113:c177-82. 496.Leung YY, Szeto CC, Tam LS, et al. Urine protein-to-creatinine ratio in an untimed urine collection is a reliable measure of proteinuria in lupus nephritis. Rheumatology (Oxford) 2007;46:649-52. 497.Salesi M, Karimifar M, Farajzadegan Z, et al. The protein-creatinine ratio in spot morning urine samples and 24-h urinary protein excretion in patients with systemic lupus erythematosus. Rheumatol Int 2009;29:503-7. 498.Sessoms S, Mehta K, Kovarsky J. Quantitation of proteinuria in systemic lupus erythematosus by use of a random, spot urine collection. Arthritis Rheum 1983;26:918-20. 499.Siedner MJ, Gelber AC, Rovin BH, et al. Diagnostic accuracy study of urine dipstick in relation to 24-hour measurement as a screening tool for proteinuria in lupus nephritis. J Rheumatol 2008;35:84-90. 500.Wang G, Lai FM, Tam LS, et al. Messenger RNA expression of podocyte-associated molecules in urinary sediment of patients with lupus nephritis. J Rheumatol 2007;34:235864. 501.Chan RW, Chow KM, Tam LS, et al. Can the urine dipstick test reduce the need for microscopy for assessment of systemic lupus erythematosus disease activity? J Rheumatol 2005;32:828-31. 502.Chotayaporn T, Kasitanon N, Sukitawut W, Louthrenoo W. Comparison of proteinuria determination by urine dipstick, spot urine protein creatinine index, and urine protein 24 hours in lupus patients. J Clin Rheumatol 2011;17:124-9. 503.Sabry A, Sheashaa H, El-Husseini A, El-Dahshan K, Abdel-Rahim M, Elbasyouni SR. Intercellular adhesion molecules in systemic lupus erythematosus patients with lupus nephritis. Clin Rheumatol 2007;26:1819-23. 44 504.Spronk PE, Bootsma H, Huitema MG, Limburg PC, Kallenberg CG. Levels of soluble VCAM-1, soluble ICAM-1, and soluble E-selectin during disease exacerbations in patients with systemic lupus erythematosus (SLE); a long term prospective study. Clin Exp Immunol 1994;97:439-44. 505.Clough JD, Barna BP, Danao-Camara TC, Chang RK. Serological detection of disease activity in SLE. Clin Biochem 1992;25:201-8. 506.Mok MY, Wu HJ, Lo Y, Lau CS. The relation of interleukin 17 (IL-17) and IL-23 to Th1/Th2 cytokines and disease activity in systemic lupus erythematosus. J Rheumatol 2010;37:2046-52. 507.Lee HT, Shiao YM, Wu TH, et al. Serum BLC/CXCL13 concentrations and renal expression of CXCL13/CXCR5 in patients with systemic lupus erythematosus and lupus nephritis. J Rheumatol 2010;37:45-52. 508.Kim HA, Jeon JY, Yoon JM, Suh CH. Beta 2-microglobulin can be a disease activity marker in systemic lupus erythematosus. Am J Med Sci 2010;339:337-40. 509.Leanos-Miranda A, Cardenas-Mondragon G. Serum free prolactin concentrations in patients with systemic lupus erythematosus are associated with lupus activity. Rheumatology (Oxford) 2006;45:97-101. 510.Li Y, Lee PY, Sobel ES, et al. Increased expression of FcgammaRI/CD64 on circulating monocytes parallels ongoing inflammation and nephritis in lupus. Arthritis Res Ther 2009;11:R6. 511.Zhao LD, Li Y, Smith MF, Jr., et al. Expressions of BAFF/BAFF receptors and their correlation with disease activity in Chinese SLE patients. Lupus 2010;19:1534-49. 512.Gilkeson G, Cannon C, Oates J, Reilly C, Goldman D, Petri M. Correlation of serum measures of nitric oxide production with lupus disease activity. J Rheumatol 1999;26:31824. 513.Kotajima L, Aotsuka S, Fujimani M, et al. Increased levels of matrix metalloproteinase-3 in sera from patients with active lupus nephritis. Clin Exp Rheumatol 1998;16:409-15. 514.Bobkova I, Lysenko L, Polyantseva L, Tareyeva I. Urinary von Willebrand factor as a marker of lupus nephritis progression. Nephron 2001;87:369-70. 515.Chan RW, Tam LS, Li EK, et al. Inflammatory cytokine gene expression in the urinary sediment of patients with lupus nephritis. Arthritis Rheum 2003;48:1326-31. 516.Kiani AN, Johnson K, Chen C, et al. Urine osteoprotegerin and monocyte chemoattractant protein-1 in lupus nephritis. J Rheumatol 2009;36:2224-30. 517.Schwartz N, Su L, Burkly LC, et al. Urinary TWEAK and the activity of lupus nephritis. J Autoimmun 2006;27:242-50. 518.Schwartz N, Rubinstein T, Burkly LC, et al. Urinary TWEAK as a biomarker of lupus nephritis: a multicenter cohort study. Arthritis Res Ther 2009;11:R143. 519.Rubinstein T, Pitashny M, Levine B, et al. Urinary neutrophil gelatinase-associated lipocalin as a novel biomarker for disease activity in lupus nephritis. Rheumatology (Oxford) 2010;49:960-71. 520.Zhang X, Jin M, Wu H, et al. Biomarkers of lupus nephritis determined by serial urine proteomics. Kidney Int 2008;74:799-807. 521.ter Borg EJ, de Jong PE, Meijer SS, Kallenberg CG. Tubular dysfunction in proliferative lupus nephritis. Am J Nephrol 1991;11:16-22. 522.Wang G, Lai FM, Tam LS, et al. Urinary FOXP3 mRNA in patients with lupus nephritis--relation with disease activity and treatment response. Rheumatology (Oxford) 2009;48:755-60. 523.Daleboudt GM, Bajema IM, Goemaere NN, van Laar JM, Bruijn JA, Berger SP. The clinical relevance of a repeat biopsy in lupus nephritis flares. Nephrol Dial Transplant 2009;24:3712-7. 524.Ginzler EM, Nicastri AD, Chen CK, Friedman EA, Diamond HS, Kaplan D. Progression of mesangial and focal to diffuse lupus nephritis. N Engl J Med 1974;291:693-6. 525.Hecht B, Siegel N, Adler M, Kashgarian M, Hayslett JP. Prognostic indices in lupus nephritis. Medicine (Baltimore) 1976;55:163-81. 526.Hill GS, Delahousse M, Nochy D, et al. Predictive power of the second renal biopsy in lupus nephritis: significance of macrophages. Kidney Int 2001;59:304-16. 527.Jarrett MP, Sablay LB, Walter L, Barland P, Grayzel AI. The effect of continuous normalization of serum hemolytic complement on the course of lupus nephritis: a five year prospective study. Am J Med 1981;70:1067-72. 528.Lee HS, Mujais SK, Kasinath BS, Spargo BH, Katz AI. Course of renal pathology in patients with systemic lupus erythematosus. Am J Med 1984;77:612-20. 529.Lu J, Tam LS, Lai FM, et al. Repeat renal biopsy in lupus nephritis: a change in histological pattern is common. Am J Nephrol 2011;34:220-5. 530.Bajaj S, Albert L, Gladman DD, Urowitz MB, Hallett DC, Ritchie S. Serial renal biopsy in systemic lupus erythematosus. J Rheumatol 2000;27:2822-6. 531.Chrysochou C, Randhawa H, Reeve R, et al. Determinants of renal functional outcome in lupus nephritis: a single centre retrospective study. Qjm 2008;101:313-6. 532.Castro Wd, Morales J, Wagner M, Graudenz M, Edelweiss M, Gonçalves L. Hypertension and Afro-descendant ethnicity: a bad interaction for lupus nephritis treated with cyclophosphamide? Lupus 2008;16:724-30. 45 533.Dooley MA, Hogan S, Jennette C, Falk R. Cyclophosphamide therapy for lupus nephritis: poor renal survival in black Americans. Glomerular Disease Collaborative Network. Kidney Int 1997;51:1188-95. 534.Korbet SM, Schwartz MM, Evans J, Lewis EJ. Severe lupus nephritis: racial differences in presentation and outcome. J Am Soc Nephrol 2007;18:244-54. 535.Nossent JC, Bronsveld W, Swaak AJ. Systemic lupus erythematosus. III. Observations on clinical renal involvement and follow up of renal function: Dutch experience with 110 patients studied prospectively. Ann Rheum Dis 1989;48:810-6. 536.Resende AL, Titan SM, Barros RT, Woronik V. Worse renal outcome of lupus nephritis in male patients: a case-control study. Lupus 2011;20:561-7. 537.Rzany B, Coresh J, Whelton PK, Petri M. Risk factors for hypercreatinemia in patients with systemic lupus erythematosus. Lupus 1999;8:532-40. 538.Tisseverasinghe A, Lim S, Greenwood C, Urowitz M, Gladman D, Fortin PR. Association between serum total cholesterol level and renal outcome in systemic lupus erythematosus. Arthritis Rheum 2006;54:2211-9. 539.Wallace DJ, Podell TE, Weiner JM, et al. Lupus nephritis. Experience with 230 patients in a private practice from 1950 to 1980. Am J Med 1982;72:209-20. 540.Zweiman B, Kornblum J, Cornog J, Hildreth EA. The prognosis of lupus nephritis. Role of clinical-pathologic correlations. Ann Intern Med 1968;69:441-62. 541.Ginzler EM, Diamond HS, Weiner M, et al. A multicenter study of outcome in systemic lupus erythematosus. I. Entry variables as predictors of prognosis. Arthritis Rheum 1982;25:601-11. 542.Mercadal L, Montcel ST, Nochy D, et al. Factors affecting outcome and prognosis in membranous lupus nephropathy. Nephrol Dial Transplant 2002;17:1771-8. 543.Rabbani MA, Habib HB, Islam M, et al. Early renal damage assessed by the SLICC/ACR damage index is predictor of severe outcome in lupus patients in Pakistan. Lupus 2010;19:1573-8. 544.Bastian HM, Alarcon GS, Roseman JM, et al. Systemic lupus erythematosus in a multiethnic US cohort (LUMINA) XL II: factors predictive of new or worsening proteinuria. Rheumatology (Oxford) 2007;46:683-9. 545.Burling F, Ng J, Thein H, Ly J, Marshall MR, Gow P. Ethnic, clinical and immunological factors in systemic lupus erythematosus and the development of lupus nephritis: results from a multi-ethnic New Zealand cohort. Lupus 2007;16:830-7. 546.Cervera R, Khamashta MA, Font J, et al. Morbidity and mortality in systemic lupus erythematosus during a 5-year period. A multicenter prospective study of 1,000 patients. European Working Party on Systemic Lupus Erythematosus. Medicine (Baltimore) 1999;78:167-75. 547.Linnik MD, Hu JZ, Heilbrunn KR, Strand V, Hurley FL, Joh T. Relationship between anti-double-stranded DNA antibodies and exacerbation of renal disease in patients with systemic lupus erythematosus. Arthritis Rheum 2005;52:1129-37. 548.Petri M, Singh S, Tesfasyone H, Malik A. Prevalence of flare and influence of demographic and serologic factors on flare risk in systemic lupus erythematosus: a prospective study. J Rheumatol 2009;36:2476-80. 549.To CH, Petri M. Is antibody clustering predictive of clinical subsets and damage in systemic lupus erythematosus? Arthritis Rheum 2005;52:4003-10. 550.van den Berg L, Nossent H, Rekvig O. Prior anti-dsDNA antibody status does not predict later disease manifestations in systemic lupus erythematosus. Clin Rheumatol 2006;25:347-52. 551.Vila LM, Molina MJ, Mayor AM, Peredo RA, Santaella ML, Vila S. Clinical and prognostic value of autoantibodies in puerto Ricans with systemic lupus erythematosus. Lupus 2006;15:892-8. 552.Adler M, Chambers S, Edwards C, Neild G, Isenberg D. An assessment of renal failure in an SLE cohort with special reference to ethnicity, over a 25-year period. Rheumatology (Oxford) 2006. 553.Sullivan KE, Wisnieski JJ, Winkelstein JA, et al. Serum complement determinations in patients with quiescent systemic lupus erythematosus. J Rheumatol 1996;23:2063-7. 554.Nieves-Plaza M, Ortiz AP, Colon M, et al. Outcome and predictors of kidney disease progression in Puerto Ricans with systemic lupus erythematosus initially presenting with mild renal involvement. J Clin Rheumatol 2011;17:179-84. 555.Stinton LM, Barr SG, Tibbles LA, et al. Autoantibodies in lupus nephritis patients requiring renal transplantation. Lupus 2007;16:394-400. 556.Wasicek CA, Reichlin M. Clinical and serological differences between systemic lupus erythematosus patients with antibodies to Ro versus patients with antibodies to Ro and La. J Clin Invest 1982;69:835-43. 557.Meyer OC, Nicaise-Roland P, Cadoudal N, et al. Anti-C1q antibodies antedate patent active glomerulonephritis in patients with systemic lupus erythematosus. Arthritis Res Ther 2009;11:R87. 46 558.Blanco FJ, Gomez-Reino JJ, de la Mata J, et al. Survival analysis of 306 European Spanish patients with systemic lupus erythematosus. Lupus 1998;7:159-63. 559.Nossent JC. Clinical renal involvement in Afro-Caribbean lupus patients. Lupus 1993;2:173-6. 560.Fraenkel L, MacKenzie T, Joseph L, Kashgarian M, Hayslett JP, Esdaile JM. Response to treatment as a predictor of longterm outcome in patients with lupus nephritis. J Rheumatol 1994;21:2052-7. 561.Budman DR, Steinberg AD. Hypertension and renal disease in systemic lupus erythematosus. Arch Intern Med 1976;136:1003-7. 562.Naiker IP, Chrystal V, Randeree IG, Seedat YK. The significance of arterial hypertension at the onset of clinical lupus nephritis. Postgrad Med J 1997;73:230-3. 563.Petri M, Perez-Gutthann S, Longenecker JC, Hochberg M. Morbidity of systemic lupus erythematosus: role of race and socioeconomic status. Am J Med 1991;91:345-53. 564.Petrin J, Rozman B, Dolenc P, et al. The dissociation of arterial hypertension and lupus glomerulonephritis in systemic lupus erythematosus. Blood Press 1993;2:108-12. 565.Ward MM, Studenski S. Clinical prognostic factors in lupus nephritis. The importance of hypertension and smoking. Arch Intern Med 1992;152:2082-8. 566.Ginzler EM, Felson DT, Anthony JM, Anderson JJ. Hypertension increases the risk of renal deterioration in systemic lupus erythematosus. J Rheumatol 1993;20:1694-700. 567.Costenbader KH, Desai A, Alarcon GS, et al. Trends in the incidence, demographics, and outcomes of end-stage renal disease due to lupus nephritis in the US from 1995 to 2006. Arthritis Rheum 2011;63:1681-8. 568.Nissenson AR, Port FK. Outcome of end-stage renal disease in patients with rare causes of renal failure. III. Systemic/vascular disorders. Q J Med 1990;74:63-74. 569.Sitter T, Spannagl M, Schiffl H. Anticardiolipin antibodies and lupus anticoagulant in patients treated with different methods of renal replacement therapy in comparison to patients with systemic lupus erythematosus. Ann Hematol 1992;65:79-82. 570.Cheigh JS, Stenzel KH, Rubin AL, Chami J, Sullivan JF. Systemic lupus erythematosus in patients with chronic renal failure. Am J Med 1983;75:602-6. 571.Lee PT, Fang HC, Chen CL, Chiou YH, Chou KJ, Chung HM. Poor prognosis of end-stage renal disease in systemic lupus erythematosus: a cohort of Chinese patients. Lupus 2003;12:827-32. 572.Iseki K, Nishime K, Uehara H, Osawa A, Fukiyama K. Effect of renal diseases and comorbid conditions on survival in chronic dialysis patients. Nephron 1994;68:80-6. 573.Jarrett MP, Santhanam S, Del Greco F. The clinical course of end-stage renal disease in systemic lupus erythematosus. Arch Intern Med 1983;143:1353-6. 574.Huang JW, Hung KY, Yen CJ, Wu KD, Tsai TJ. Systemic lupus erythematosus and peritoneal dialysis: outcomes and infectious complications. Perit Dial Int 2001;21:143-7. 575.Kimberly RP, Lockshin MD, Sherman RL, Mouradian J, Saal S. Reversible "end-stage" lupus nephritis. Analysis of patients able to discontinue dialysis. Am J Med 1983;74:361-8. 576.Liang CC, Huang CC, Wang IK, et al. Impact of renal survival on the course and outcome of systemic lupus erythematosus patients treated with chronic peritoneal dialysis. Ther Apher Dial 2010;14:35-42. 577.Nossent HC, Swaak TJ, Berden JH. Systemic lupus erythematosus: analysis of disease activity in 55 patients with end-stage renal failure treated with hemodialysis or continuous ambulatory peritoneal dialysis. Dutch Working Party on SLE. Am J Med 1990;89:169-74. 578.Perkins RM, Reynolds JC, Ahuja TS, et al. Thrombotic microangiopathy in United States long-term dialysis patients. Nephrol Dial Transplant 2006;21:191-6. 579.Sires RL, Adler SG, Louie JS, Cohen AH. Poor prognosis in end-stage lupus nephritis due to nonautologous vascular access site associated septicemia and lupus flares. Am J Nephrol 1989;9:279-84. 580.Siu YP, Leung KT, Tong MK, Kwan TH, Mok CC. Clinical outcomes of systemic lupus erythematosus patients undergoing continuous ambulatory peritoneal dialysis. Nephrol Dial Transplant 2005;20:2797-802. 581.Weng CH, Hsu CW, Yu CC, Yen TH, Yang CW, Hung CC. Peritoneal dialysis and hemodialysis in systemic lupus erythematosus patients: comparison of clinical outcomes. Kidney Blood Press Res 2009;32:451-6. 582.Sule S, Fivush B, Neu A, Furth S. Increased risk of death in pediatric and adult patients with ESRD secondary to lupus. Pediatr Nephrol 2011;26:93-8. 583.Correia P, Cameron JS, Lian JD, et al. Why do patients with lupus nephritis die? Br Med J (Clin Res Ed) 1985;290:126-31. 584.Shafi ST, Gupta M. Risk of vascular access thrombosis in patients with systemic lupus erythematosus on hemodialysis. J Vasc Access 2007;8:103-8. 585.Andrews PA, Warr KJ, Hicks JA, Cameron JS. Impaired outcome of continuous ambulatory peritoneal dialysis in immunosuppressed patients. Nephrol Dial Transplant 1996;11:1104-8. 586.Ward MM. Cardiovascular and cerebrovascular morbidity and mortality among women with end-stage renal disease attributable to lupus nephritis. Am J Kidney Dis 2000;36:516-25. 47 587.Coplon NS, Diskin CJ, Petersen J, Swenson RS. The long-term clinical course of systemic lupus erythematosus in end-stage renal disease. N Engl J Med 1983;308:186-90. 588.Heine G, Sester U, Sester M, Scherberich JE, Girndt M, Kohler H. A shift in the Th(1)/Th(2) ratio accompanies the clinical remission of systemic lupus erythematosus in patients with end-stage renal disease. Nephrol Dial Transplant 2002;17:1790-4. 589.Moroni G, Tantardini F, Gallelli B, et al. The long-term prognosis of renal transplantation in patients with lupus nephritis. Am J Kidney Dis 2005;45:903-11. 590.Nossent HC, Swaak TJ, Berden JH. Systemic lupus erythematosus after renal transplantation: patient and graft survival and disease activity. The Dutch Working Party on Systemic Lupus Erythematosus. Ann Intern Med 1991;114:183-8. 591.Krane NK, Burjak K, Archie M, O'Donovan R. Persistent lupus activity in end-stage renal disease. Am J Kidney Dis 1999;33:872-9. 592.Okano K, Yumura W, Nitta K, et al. Analysis of lupus activity in end-stage renal disease treated by hemodialysis. Intern Med 2001;40:598-602. 593.Ribeiro FM, Leite MA, Velarde GC, Fabris CL, Santos RC, Lugon JR. Activity of systemic lupus erythematosus in end-stage renal disease patients: study in a Brazilian cohort. Am J Nephrol 2005;25:596-603. 594.Rodby RA, Korbet SM, Lewis EJ. Persistence of clinical and serologic activity in patients with systemic lupus erythematosus undergoing peritoneal dialysis. Am J Med 1987;83:613-8. 595.Szeto CC, Li PK, Wong TY, Leung CB, Lui SF. Factors associated with active systemic lupus erythematosus after endstage renal disease. J Rheumatol 1998;25:1520-5. 596.Cheigh JS, Kim H, Stenzel KH, et al. Systemic lupus erythematosus in patients with end-stage renal disease: long-term follow-up on the prognosis of patients and the evolution of lupus activity. Am J Kidney Dis 1990;16:189-95. 597.Signori Baracat AL, Ribeiro-Alves MA, Alves-Filho G, Mazzali M. Systemic lupus erythematosus after renal transplantation: is complement a good marker for graft survival? Transplant Proc 2008;40:746-8. 598.Tang H, Chelamcharla M, Baird BC, Shihab FS, Koford JK, Goldfarb-Rumyantzev AS. Factors affecting kidney-transplant outcome in recipients with lupus nephritis. Clin Transplant 2008;22:263-72. 599.Tang H, Poynton MR, Hurdle JF, Baird BC, Koford JK, Goldfarb-Rumyantzev AS. Predicting three-year kidney graft survival in recipients with systemic lupus erythematosus. Asaio J 2011;57:300-9. 600.Ward MM. Outcomes of renal transplantation among patients with end-stage renal disease caused by lupus nephritis. Kidney Int 2000;57:2136-43. 601.Bumgardner GL, Mauer SM, Payne W, et al. Single-center 1-15-year results of renal transplantation in patients with systemic lupus erythematosus. Transplantation 1988;46:703-9. 602.Bunnapradist S, Chung P, Peng A, et al. Outcomes of renal transplantation for recipients with lupus nephritis: analysis of the Organ Procurement and Transplantation Network database. Transplantation 2006;82:612-8. 603.Lochhead KM, Pirsch JD, D'Alessandro AM, et al. Risk factors for renal allograft loss in patients with systemic lupus erythematosus. Kidney Int 1996;49:512-7. 604.Roth D, Milgrom M, Esquenazi V, Strauss J, Zilleruelo G, Miller J. Renal transplantation in systemic lupus erythematosus: one center's experience. Am J Nephrol 1987;7:36774. 605.Burgos PI, Perkins EL, Pons-Estel GJ, et al. Risk factors and impact of recurrent lupus nephritis in patients with systemic lupus erythematosus undergoing renal transplantation: data from a single US institution. Arthritis Rheum 2009;60:2757-66. 606.Contreras G, Mattiazzi A, Guerra G, et al. Recurrence of lupus nephritis after kidney transplantation. J Am Soc Nephrol 2010;21:1200-7. 607.Stone JH, Millward CL, Olson JL, Amend WJ, Criswell LA. Frequency of recurrent lupus nephritis among ninety-seven renal transplant patients during the cyclosporine era. Arthritis Rheum 1998;41:678-86. 608.Goral S, Ynares C, Shappell SB, et al. Recurrent lupus nephritis in renal transplant recipients revisited: it is not rare. Transplantation 2003;75:651-6. 609.Lionaki S, Kapitsinou PP, Iniotaki A, Kostakis A, Moutsopoulos HM, Boletis JN. Kidney transplantation in lupus patients: a case-control study from a single centre. Lupus 2008;17:670-5. 610.Stone JH, Amend WJ, Criswell LA. Outcome of renal transplantation in ninety-seven cyclosporine-era patients with systemic lupus erythematosus and matched controls. Arthritis Rheum 1998;41:1438-45. 611.Villaverde Verdejo P, Fernandez Rivera C, Alonso Hernandez A, et al. Evaluation of renal grafts in patients with lupus nephritis as cause of end-stage renal disease. Transplant Proc 2005;37:1426-7. 48 612.Goss JA, Cole BR, Jendrisak MD, et al. Renal transplantation for systemic lupus erythematosus and recurrent lupus nephritis. A single-center experience and a review of the literature. Transplantation 1991;52:805-10. 613.Magee JC, Leichtman AB, Merion RM. Renal transplantation for systemic lupus erythematosis: excellent long-term results with both living and cadaveric donors. Transplant Proc 1998;30:1798-9. 614.Mejia G, Zimmerman SW, Glass NR, Miller DT, Sollinger HW, Belzer FO. Renal transplantation in patients with systemic lupus erythematosus. Arch Intern Med 1983;143:2089-92. 615.Stone JH, Amend WJ, Criswell LA. Outcome of renal transplantation in systemic lupus erythematosus. Semin Arthritis Rheum 1997;27:17-26. 616.Stone JH, Amend WJ, Criswell LA. Antiphospholipid antibody syndrome in renal transplantation: occurrence of clinical events in 96 consecutive patients with systemic lupus erythematosus. Am J Kidney Dis 1999;34:1040-7. 617.Vaidya S, Daller J, Gugliuzza K. Role of anti-beta 2 glycoprotein 1 antibodies in ESRD patients with antiphospholipid antibody syndrome. Clin Transplant 2002;16:362-7. 618.Vaidya S, Sellers R, Kimball P, et al. Frequency, potential risk and therapeutic intervention in end-stage renal disease patients with antiphospholipid antibody syndrome: a multicenter study. Transplantation 2000;69:1348-52. 619.Vaidya S, Wang CC, Gugliuzza C, Fish JC. Relative risk of post-transplant renal thrombosis in patients with antiphospholipid antibodies. Clin Transplant 1998;12:439-44. 620.Radhakrishnan J, Williams GS, Appel GB, Cohen DJ. Renal transplantation in anticardiolipin antibody-positive lupus erythematosus patients. Am J Kidney Dis 1994;23:286-9. 621.Azevedo LS, Romao JE, Jr., Malheiros D, Saldanha LB, Ianhez LE, Sabbaga E. Renal transplantation in systemic lupus erythematosus. A case control study of 45 patients. Nephrol Dial Transplant 1998;13:2894-8. 622.Dong G, Panaro F, Bogetti D, et al. Standard chronic immunosuppression after kidney transplantation for systemic lupus erythematosus eliminates recurrence of disease. Clin Transplant 2005;19:56-60. 623.el-Shahawy MA, Aswad S, Mendez RG, Bangsil R, Mendez R, Massry SG. Renal transplantation in systemic lupus erythematosus: a single-center experience with sixty-four cases. Am J Nephrol 1995;15:123-8. 624.Ghafari A, Etemadi J, Ardalan MR. Renal transplantation in patients with lupus nephritis: a single-center experience. Transplant Proc 2008;40:143-4. 625.Meehan SM, Chang A, Khurana A, Baliga R, Kadambi PV, Javaid B. Pauci-immune and immune glomerular lesions in kidney transplants for systemic lupus erythematosus. Clin J Am Soc Nephrol 2008;3:1469-78. 626.Grimbert P, Frappier J, Bedrossian J, et al. Long-term outcome of kidney transplantation in patients with systemic lupus erythematosus: a multicenter study. Groupe Cooperatif de Transplantation d'ile de France. Transplantation 1998;66:1000-3. 627.Grimbert P, Lang P, Frappier J, et al. Renal transplantation in patients with systemic lupus erythematosus: a multicenter study. Transplant Proc 1997;29:2363-4. 628.Norby GE, Strom EH, Midtvedt K, et al. Recurrent lupus nephritis after kidney transplantation: a surveillance biopsy study. Ann Rheum Dis 2010;69:1484-7. 629.Nyberg G, Blohme I, Persson H, Olausson M, Svalander C. Recurrence of SLE in transplanted kidneys: a follow-up transplant biopsy study. Nephrol Dial Transplant 1992;7:1116-23. 630.Tsang WK, Tong KL, Tang HL, Chu KH, Chan HW. Thirteen-year results of renal transplantation in patients with systemic lupus erythematosus. Transplant Proc 2000;32:18245. 631.Norby GE, Holme I, Fellstrom B, et al. Effect of fluvastatin on cardiac outcomes in kidney transplant patients with systemic lupus erythematosus: A randomized placebocontrolled study. Arthritis Rheum 2009;60:1060-4. 632.Abu-Shakra M, Gladman DD, Urowitz MB, Farewell V. Anticardiolipin antibodies in systemic lupus erythematosus: clinical and laboratory correlations. Am J Med 1995;99:624-8. 633.Bhandari S, Harnden P, Brownjohn AM, Turney JH. Association of anticardiolipin antibodies with intraglomerular thrombi and renal dysfunction in lupus nephritis. Qjm 1998;91:401-9. 634.Frampton G, Hicks J, Cameron JS. Significance of anti-phospholipid antibodies in patients with lupus nephritis. Kidney Int 1991;39:1225-31. 635.Mehrani T, Petri M. IgM anti-beta2 glycoprotein I is protective against lupus nephritis and renal damage in systemic lupus erythematosus. J Rheumatol 2011;38:450-3. 636.Mehrani T, Petri M. Association of IgA Anti-beta2 glycoprotein I with clinical and laboratory manifestations of systemic lupus erythematosus. J Rheumatol 2011;38:64-8. 49 637.Moroni G, Ventura D, Riva P, et al. Antiphospholipid antibodies are associated with an increased risk for chronic renal insufficiency in patients with lupus nephritis. Am J Kidney Dis 2004;43:28-36. 638.Naiker IP, Rughubar KN, Duursma J, Pudifin DJ, Seedat YK. Anticardiolipin antibodies in South African patients with lupus nephritis: a clinical and renal pathological study. Am J Nephrol 2000;20:351-7. 639.Tsuruta Y, Uchida K, Itabashi M, Yumura W, Nitta K. Antiphospholipid antibodies and renal outcomes in patients with lupus nephritis. Intern Med 2009;48:1875-80. 640.Natejumnong C, Ruangkanchanasetr P, Aimpun P, Supaporn T. Significance of antiphospholipid antibodies in lupus nephritis. J Med Assoc Thai 2006;89 Suppl 2:S121-8. 641.Cheunsuchon B, Rungkaew P, Chawanasuntorapoj R, Pattaragarn A, Parichatikanond P. Prevalence and clinicopathologic findings of antiphospholipid syndrome nephropathy in Thai systemic lupus erythematosus patients who underwent renal biopsies. Nephrology (Carlton) 2007;12:474-80. 642.Daugas E, Nochy D, Huong DL, et al. Antiphospholipid syndrome nephropathy in systemic lupus erythematosus. J Am Soc Nephrol 2002;13:42-52. 643.Tektonidou MG, Sotsiou F, Nakopoulou L, Vlachoyiannopoulos PG, Moutsopoulos HM. Antiphospholipid syndrome nephropathy in patients with systemic lupus erythematosus and antiphospholipid antibodies: prevalence, clinical associations, and long-term outcome. Arthritis Rheum 2004;50:2569-79. 644.Silvarino R, Sant F, Espinosa G, et al. Nephropathy associated with antiphospholipid antibodies in patients with systemic lupus erythematosus. Lupus 2011;20:721-9. 645.Zheng H, Chen Y, Ao W, et al. Antiphospholipid antibody profiles in lupus nephritis with glomerular microthrombosis: a prospective study of 124 cases. Arthritis Res Ther 2009;11:R93. 646.Galindo M, Gonzalo E, Martinez-Vidal MP, et al. Immunohistochemical detection of intravascular platelet microthrombi in patients with lupus nephritis and anti-phospholipid antibodies. Rheumatology (Oxford) 2009;48:1003-7. 647.Bridoux F, Vrtovsnik F, Noel C, et al. Renal thrombotic microangiopathy in systemic lupus erythematosus: clinical correlations and long-term renal survival. Nephrol Dial Transplant 1998;13:298-304. 648.Perdiguero M, Boronat M, Marco P, Rivera F. The role of antiphospholipid antibodies in lupus nephropathy. Nephron 1995;71:35-9. 649.Shen YM, Lee R, Frenkel E, Sarode R. IgA antiphospholipid antibodies are an independent risk factor for thromboses. Lupus 2008;17:996-1003. 650.Moss KE, Isenberg DA. Comparison of renal disease severity and outcome in patients with primary antiphospholipid syndrome, antiphospholipid syndrome secondary to systemic lupus erythematosus (SLE) and SLE alone. Rheumatology (Oxford) 2001;40:863-7. 651.Farrugia E, Torres VE, Gastineau D, Michet CJ, Holley KE. Lupus anticoagulant in systemic lupus erythematosus: a clinical and renal pathological study. Am J Kidney Dis 1992;20:463-71. 652.Miranda JM, Garcia-Torres R, Jara LJ, Medina F, Cervera H, Fraga A. Renal biopsy in systemic lupus erythematosus: significance of glomerular thrombosis. Analysis of 108 cases. Lupus 1994;3:25-9. 653.Kant KS, Pollak VE, Weiss MA, Glueck HI, Miller AN, Hess EV. Glomerular thrombosis in systemic lupus erythematosus: prevalence and significance. Medicine (Baltimore) 1981;60:71-86. 654.Glueck HI, Kant KS, Weiss MA, Pollak VE, Miller MA, Coots M. Thrombosis in systemic lupus erythematosus. Relation to the presence of circulating anticoagulants. Arch Intern Med 1985;145:1389-95. 655.Canaud G, Bienaime F, Noel LH, et al. Severe vascular lesions and poor functional outcome in kidney transplant recipients with lupus anticoagulant antibodies. Am J Transplant 2010;10:2051-60. 656.Al Arfaj AS, Khalil N. Pregnancy outcome in 396 pregnancies in patients with SLE in Saudi Arabia. Lupus 2010;19:1665-73. 657.Gimovsky ML, Montoro M, Paul RH. Pregnancy outcome in women with systemic lupus erythematosus. Obstet Gynecol 1984;63:686-92. 658.Cortes-Hernandez J, Ordi-Ros J, Paredes F, Casellas M, Castillo F, Vilardell-Tarres M. Clinical predictors of fetal and maternal outcome in systemic lupus erythematosus: a prospective study of 103 pregnancies. Rheumatology (Oxford) 2002;41:643-50. 659.Packham DK, Lam SS, Nicholls K, Fairley KF, Kincaid-Smith PS. Lupus nephritis and pregnancy. Q J Med 1992;83:315-24. 660.Clowse ME, Magder LS, Witter F, Petri M. Early risk factors for pregnancy loss in lupus. Obstet Gynecol 2006;107:293-9. 661.Hayslett JP, Lynn RI. Effect of pregnancy in patients with lupus nephropathy. Kidney Int 1980;18:207-20. 662.Le Thi Huong D, Wechsler B, Piette JC, Bletry O, Godeau P. Pregnancy and its outcome in systemic lupus erythematosus. Qjm 1994;87:721-9. 663.Moroni G, Quaglini S, Banfi G, et al. Pregnancy in lupus nephritis. Am J Kidney Dis 2002;40:713-20. 50 664.Rahman FZ, Rahman J, Al-Suleiman SA, Rahman MS. Pregnancy outcome in lupus nephropathy. Arch Gynecol Obstet 2005;271:222-6. 665.Wagner SJ, Craici I, Reed D, et al. Maternal and foetal outcomes in pregnant patients with active lupus nephritis. Lupus 2009;18:342-7. 666.Carmona F, Font J, Moga I, et al. Class III-IV proliferative lupus nephritis and pregnancy: a study of 42 cases. Am J Reprod Immunol 2005;53:182-8. 667.Aggarwal N, Sawhney H, Vasishta K, Chopra S, Bambery P. Pregnancy in patients with systemic lupus erythematosus. Aust N Z J Obstet Gynaecol 1999;39:28-30. 668.Clowse ME, Magder LS, Witter F, Petri M. The impact of increased lupus activity on obstetric outcomes. Arthritis Rheum 2005;52:514-21. 669.Cavallasca JA, Laborde HA, Ruda-Vega H, Nasswetter GG. Maternal and fetal outcomes of 72 pregnancies in Argentine patients with systemic lupus erythematosus (SLE). Clin Rheumatol 2008;27:41-6. 670.Imbasciati E, Surian M, Bottino S, et al. Lupus nephropathy and pregnancy. A study of 26 pregnancies in patients with systemic lupus erythematosus and nephritis. Nephron 1984;36:46-51. 671.Jungers P, Dougados M, Pelissier C, et al. Lupus nephropathy and pregnancy. Report of 104 cases in 36 patients. Arch Intern Med 1982;142:771-6. 672.Georgiou PE, Politi EN, Katsimbri P, Sakka V, Drosos AA. Outcome of lupus pregnancy: a controlled study. Rheumatology (Oxford) 2000;39:1014-9. 673.Johns KR, Morand EF, Littlejohn GO. Pregnancy outcome in systemic lupus erythematosus (SLE): a review of 54 cases. Aust N Z J Med 1998;28:18-22. 674.Clowse ME, Magder LS, Petri M. The clinical utility of measuring complement and anti-dsDNA antibodies during pregnancy in patients with systemic lupus erythematosus. J Rheumatol 2011;38:1012-6. 675.Rahman P, Gladman DD, Urowitz MB. Clinical predictors of fetal outcome in systemic lupus erythematosus. J Rheumatol 1998;25:1526-30. 676.Kwok LW, Tam LS, Zhu T, Leung YY, Li E. Predictors of maternal and fetal outcomes in pregnancies of patients with systemic lupus erythematosus. Lupus 2011;20:829-36. 677.Julkunen H, Jouhikainen T, Kaaja R, et al. Fetal outcome in lupus pregnancy: a retrospective case-control study of 242 pregnancies in 112 patients. Lupus 1993;2:125-31. 678.Carmona F, Font J, Cervera R, Munoz F, Cararach V, Balasch J. Obstetrical outcome of pregnancy in patients with systemic Lupus erythematosus. A study of 60 cases. Eur J Obstet Gynecol Reprod Biol 1999;83:137-42. 679.Chakravarty EF, Colon I, Langen ES, et al. Factors that predict prematurity and preeclampsia in pregnancies that are complicated by systemic lupus erythematosus. Am J Obstet Gynecol 2005;192:1897-904. 680.Imbasciati E, Tincani A, Gregorini G, et al. Pregnancy in women with pre-existing lupus nephritis: predictors of fetal and maternal outcome. Nephrol Dial Transplant 2009;24:519-25. 681.Julkunen H, Kaaja R, Palosuo T, Gronhagen-Riska C, Teramo K. Pregnancy in lupus nephropathy. Acta Obstet Gynecol Scand 1993;72:258-63. 682.Huong DL, Wechsler B, Vauthier-Brouzes D, Beaufils H, Lefebvre G, Piette JC. Pregnancy in past or present lupus nephritis: a study of 32 pregnancies from a single centre. Ann Rheum Dis 2001;60:599-604. 683.Oviasu E, Hicks J, Cameron JS. The outcome of pregnancy in women with lupus nephritis. Lupus 1991;1:19-25. 684.Smyth A, Oliveira GH, Lahr BD, Bailey KR, Norby SM, Garovic VD. A systematic review and meta-analysis of pregnancy outcomes in patients with systemic lupus erythematosus and lupus nephritis. Clin J Am Soc Nephrol 2010;5:2060-8. 685.Clark CA, Spitzer KA, Nadler JN, Laskin CA. Preterm deliveries in women with systemic lupus erythematosus. J Rheumatol 2003;30:2127-32. 686.Gladman DD, Tandon A, Ibanez D, Urowitz MB. The effect of lupus nephritis on pregnancy outcome and fetal and maternal complications. J Rheumatol 2010;37:754-8. 687.Andrade R, Sanchez ML, Alarcon GS, et al. Adverse pregnancy outcomes in women with systemic lupus erythematosus from a multiethnic US cohort: LUMINA (LVI) [corrected]. Clin Exp Rheumatol 2008;26:268-74. 688.Nicklin JL. Systemic lupus erythematosus and pregnancy at the Royal Women's Hospital, Brisbane 1979-1989. Aust N Z J Obstet Gynaecol 1991;31:128-33. 689.Soubassi L, Haidopoulos D, Sindos M, et al. Pregnancy outcome in women with pre-existing lupus nephritis. J Obstet Gynaecol 2004;24:630-4. 690.Carvalheiras G, Vita P, Marta S, et al. Pregnancy and systemic lupus erythematosus: review of clinical features and outcome of 51 pregnancies at a single institution. Clin Rev Allergy Immunol 2010;38:302-6. 691.Derksen RH, Bruinse HW, de Groot PG, Kater L. Pregnancy in systemic lupus erythematosus: a prospective study. Lupus 1994;3:149-55. 692.Clowse ME, Magder L, Witter F, Petri M. Hydroxychloroquine in lupus pregnancy. Arthritis Rheum 2006;54:3640-7. 693.Kaaja R, Julkunen H, Ammala P. Hypertension as a risk factor in pregnancies complicated by systemic lupus erythematosus. Acta Obstet Gynecol Scand 1990;69:393-6. 51 694.Le Huong D, Wechsler B, Vauthier-Brouzes D, et al. Outcome of planned pregnancies in systemic lupus erythematosus: a prospective study on 62 pregnancies. Br J Rheumatol 1997;36:772-7. 695.Mecacci F, Bianchi B, Pieralli A, et al. Pregnancy outcome in systemic lupus erythematosus complicated by anti-phospholipid antibodies. Rheumatology (Oxford) 2009;48:2469. 696.Petri M, Howard D, Repke J. Frequency of lupus flare in pregnancy. The Hopkins Lupus Pregnancy Center experience. Arthritis Rheum 1991;34:1538-45. 697.Ruiz-Irastorza G, Lima F, Alves J, et al. Increased rate of lupus flare during pregnancy and the puerperium: a prospective study of 78 pregnancies. Br J Rheumatol 1996;35:1338. 698.Tandon A, Ibanez D, Gladman DD, Urowitz MB. The effect of pregnancy on lupus nephritis. Arthritis Rheum 2004;50:3941-6. 699.Wong KL, Chan FY, Lee CP. Outcome of pregnancy in patients with systemic lupus erythematosus. A prospective study. Arch Intern Med 1991;151:269-73. 700.Bear R. Pregnancy and lupus nephritis. A detailed report of six cases with a review of the literature. Obstet Gynecol 1976;47:715-8. 701.Lockshin MD, Reinitz E, Druzin ML, Murrman M, Estes D. Lupus pregnancy. Case-control prospective study demonstrating absence of lupus exacerbation during or after pregnancy. Am J Med 1984;77:893-8. 702.Clowse ME, Jamison M, Myers E, James AH. A national study of the complications of lupus in pregnancy. Am J Obstet Gynecol 2008;199:127 e1-6. 703.Clowse ME, Magder L, Petri M. Cyclophosphamide for lupus during pregnancy. Lupus 2005;14:593-7. 704.Park MC, Park YB, Jung SY, Chung IH, Choi KH, Lee SK. Risk of ovarian failure and pregnancy outcome in patients with lupus nephritis treated with intravenous cyclophosphamide pulse therapy. Lupus 2004;13:569-74. 705.Buyon JP, Cronstein BN, Morris M, Tanner M, Weissmann G. Serum complement values (C3 and C4) to differentiate between systemic lupus activity and pre-eclampsia. Am J Med 1986;81:194-200. 706.Bader-Meunier B, Armengaud JB, Haddad E, et al. Initial presentation of childhood-onset systemic lupus erythematosus: a French multicenter study. J Pediatr 2005;146:648-53. 707.Bakr A. Epidemiology treatment and outcome of childhood systemic lupus erythematosus in Egypt. Pediatr Nephrol 2005;20:1081-6. 708.Bandeira M, Buratti S, Bartoli M, et al. Relationship between damage accrual, disease flares and cumulative drug therapies in juvenile-onset systemic lupus erythematosus. Lupus 2006;15:515-20. 709.Barron KS, Silverman ED, Gonzales J, Reveille JD. Clinical, serologic, and immunogenetic studies in childhood-onset systemic lupus erythematosus. Arthritis Rheum 1993;36:348-54. 710.Benseler SM, Bargman JM, Feldman BM, et al. Acute renal failure in paediatric systemic lupus erythematosus: treatment and outcome. Rheumatology (Oxford) 2009;48:176-82. 711.Brunner HI, Gladman DD, Ibanez D, Urowitz MD, Silverman ED. Difference in disease features between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis Rheum 2008;58:556-62. 712.Brunner HI, Higgins GC, Wiers K, et al. Health-related quality of life and its relationship to patient disease course in childhood-onset systemic lupus erythematosus. J Rheumatol 2009;36:1536-45. 713.Caeiro F, Michielson FM, Bernstein R, Hughes GR, Ansell BM. Systemic lupus erythematosus in childhood. Ann Rheum Dis 1981;40:325-31. 714.Carreno L, Lopez-Longo FJ, Monteagudo I, et al. Immunological and clinical differences between juvenile and adult onset of systemic lupus erythematosus. Lupus 1999;8:28792. 715.Coppo R, Gianoglio B, Porcellini MG, Maringhini S. Frequency of renal diseases and clinical indications for renal biopsy in children (report of the Italian National Registry of Renal Biopsies in Children). Group of Renal Immunopathology of the Italian Society of Pediatric Nephrology and Group of Renal Immunopathology of the Italian Society of Nephrology. Nephrol Dial Transplant 1998;13:293-7. 716.Descloux E, Durieu I, Cochat P, et al. Paediatric systemic lupus erythematosus: prognostic impact of antiphospholipid antibodies. Rheumatology (Oxford) 2008;47:183-7. 717.Dumas R. Lupus nephritis. Collaborative study by the French Society of Paediatric Nephrology. Arch Dis Child 1985;60:126-8. 718.Emre S, Bilge I, Sirin A, et al. Lupus nephritis in children: prognostic significance of clinicopathological findings. Nephron 2001;87:118-26. 719.Fish AJ, Blau EB, Westberg NG, Burke BA, Vernier RL, Michael AF. Systemic lupus erythematosus within the first two decades of life. Am J Med 1977;62:99-117. 720.Font J, Cervera R, Espinosa G, et al. Systemic lupus erythematosus (SLE) in childhood: analysis of clinical and immunological findings in 34 patients and comparison with SLE characteristics in adults. Ann Rheum Dis 1998;57:456-9. 52 721.Garin EH, Donnelly WH, Fennell RS, 3rd, Richard GA. Nephritis in systemic lupus erythematosus in children. J Pediatr 1976;89:366-71. 722.Hari P, Bagga A, Mahajan P, Dinda A. Outcome of lupus nephritis in Indian children. Lupus 2009;18:348-54. 723.Hersh AO, von Scheven E, Yazdany J, et al. Differences in long-term disease activity and treatment of adult patients with childhood- and adult-onset systemic lupus erythematosus. Arthritis Rheum 2009;61:13-20. 724.Hoffman IE, Lauwerys BR, De Keyser F, et al. Juvenile-onset systemic lupus erythematosus: different clinical and serological pattern than adult-onset systemic lupus erythematosus. Ann Rheum Dis 2009;68:412-5. 725.Livingston B, Bonner A, Pope J. Differences in clinical manifestations between childhood-onset lupus and adult-onset lupus: a meta-analysis. Lupus 2011;20:1345-55. 726.Miettunen PM, Ortiz-Alvarez O, Petty RE, et al. Gender and ethnic origin have no effect on longterm outcome of childhood-onset systemic lupus erythematosus. J Rheumatol 2004;31:1650-4. 727.Morris MC, Cameron JS, Chantler C, Turner DR. Systemic lupus erythematosus with nephritis. Arch Dis Child 1981;56:779-83. 728.Muzaffer MA, Al-Mayouf SM. Clinical and laboratory variables of childhood systemic lupus erythematosus in western province of Saudi Arabia. Rheumatol Int 2011;31:23-6. 729.Norris DG, Colon AR, Stickler GB. Systemic lupus erythematosus in children: the complex problems of diagnosis and treatment encountered in 101 such patients at the Mayo Clinic. Clin Pediatr (Phila) 1977;16:774-8. 730.Pande I, Sekharan NG, Kailash S, et al. Analysis of clinical and laboratory profile in Indian childhood systemic lupus erythematosus and its comparison with SLE in adults. Lupus 1993;2:83-7. 731.Rush PJ, Baumal R, Shore A, Balfe JW, Schreiber M. Correlation of renal histology with outcome in children with lupus nephritis. Kidney Int 1986;29:1066-71. 732.Taddio A, Rossetto E, Rose CD, et al. Prognostic impact of atypical presentation in pediatric systemic lupus erythematosus: results from a multicenter study. J Pediatr 2010;156:972-7. 733.Tucker LB, Uribe AG, Fernandez M, et al. Adolescent onset of lupus results in more aggressive disease and worse outcomes: results of a nested matched case-control study within LUMINA, a multiethnic US cohort (LUMINA LVII). Lupus 2008;17:314-22. 734.Walravens PA, Chase HP. The prognosis of childhood systemic lupus erythematosus. Am J Dis Child 1976;130:929-33. 735.Webb R, Kelly JA, Somers EC, et al. Early disease onset is predicted by a higher genetic risk for lupus and is associated with a more severe phenotype in lupus patients. Ann Rheum Dis 2011;70:151-6. 736.Wong SN, Tse KC, Lee TL, et al. Lupus nephritis in Chinese children--a territory-wide cohort study in Hong Kong. Pediatr Nephrol 2006;21:1104-12. 737.Woolf A, Croker B, Osofsky SG, Kredich DW. Nephritis in children and young adults with systemic lupus erythematosus and normal urinary sediment. Pediatrics 1979;64:67885. 738.Brunner HI, Freedman M, Silverman ED. Close relationship between systemic lupus erythematosus and thrombotic thrombocytopenic purpura in childhood. Arthritis Rheum 1999;42:2346-55. 739.Baqi N, Moazami S, Singh A, Ahmad H, Balachandra S, Tejani A. Lupus nephritis in children: a longitudinal study of prognostic factors and therapy. J Am Soc Nephrol 1996;7:924-9. 740.Bogdanovic R, Nikolic V, Pasic S, et al. Lupus nephritis in childhood: a review of 53 patients followed at a single center. Pediatr Nephrol 2004;19:36-44. 741.Brunner HI, Silverman ED, To T, Bombardier C, Feldman BM. Risk factors for damage in childhood-onset systemic lupus erythematosus: cumulative disease activity and medication use predict disease damage. Arthritis Rheum 2002;46:436-44. 742.Cramer CH, 2nd, Mills M, Valentini RP, Smoyer WE, Haftel H, Brophy PD. Clinical presentation and outcome in a cohort of paediatric patients with membranous lupus nephritis. Nephrol Dial Transplant 2007;22:3495-500. 743.Hagelberg S, Lee Y, Bargman J, et al. Longterm followup of childhood lupus nephritis. J Rheumatol 2002;29:2635-42. 744.Marks SD, Sebire NJ, Pilkington C, Tullus K. Clinicopathological correlations of paediatric lupus nephritis. Pediatr Nephrol 2007;22:77-83. 745.McCurdy DK, Lehman TJ, Bernstein B, et al. Lupus nephritis: prognostic factors in children. Pediatrics 1992;89:240-6. 746.Singh S, Devidayal, Minz R, Nada R, Joshi K. Childhood lupus nephritis: 12 years experience from North India. Rheumatol Int 2006;26:604-7. 747.Vachvanichsanong P, Dissaneewate P, McNeil E. Diffuse proliferative glomerulonephritis does not determine the worst outcome in childhood-onset lupus nephritis: a 23-year experience in a single centre. Nephrol Dial Transplant 2009;24:2729-34. 53 748.Zappitelli M, Duffy C, Bernard C, et al. Clinicopathological study of the WHO classification in childhood lupus nephritis. Pediatr Nephrol 2004;19:503-10. 749.Miller MN, Baumal R, Poucell S, Steele BT. Incidence and prognostic importance of glomerular crescents in renal diseases of childhood. Am J Nephrol 1984;4:244-7. 750.Zappitelli M, Duffy CM, Bernard C, Gupta IR. Evaluation of activity, chronicity and tubulointerstitial indices for childhood lupus nephritis. Pediatr Nephrol 2008;23:83-91. 751.Lee BS, Cho HY, Kim EJ, et al. Clinical outcomes of childhood lupus nephritis: a single center's experience. Pediatr Nephrol 2007;22:222-31. 752.Demircin G, Oner A, Erdogan O, et al. Long-term efficacy and safety of quadruple therapy in childhood diffuse proliferative lupus nephritis. Ren Fail 2008;30:603-9. 753.Olowu WA, Adelusola KA, Senbanjo IO. Clinicopathology of childhood-onset renal systemic lupus erythematosus. Nephrology (Carlton) 2007;12:364-70. 754.Askenazi D, Myones B, Kamdar A, et al. Outcomes of children with proliferative lupus nephritis: the role of protocol renal biopsy. Pediatr Nephrol 2007;22:981-6. 755.Aragon E, Chan YH, Ng KH, Lau YW, Tan PH, Yap HK. Good outcomes with mycophenolate-cyclosporine-based induction protocol in children with severe proliferative lupus nephritis. Lupus 2010;19:965-73. 756.Singsen BH, Bernstein BH, King KK, Hanson V. Systemic lupus erythematosus in childhood correlations between changes in disease activity and serum complement levels. J Pediatr 1976;89:358-69. 757.Watson L, Midgley A, Pilkington C, et al. Urinary monocyte chemoattractant protein 1 and alpha 1 acid glycoprotein as biomarkers of renal disease activity in juvenile-onset systemic lupus erythematosus. Lupus 2011. 758.Edelbauer M, Kshirsagar S, Riedl M, et al. Markers of childhood lupus nephritis indicating disease activity. Pediatr Nephrol 2011;26:401-10. 759.Wu FQ, Zhao Q, Cui XD, Zhang W. C1q and anti-C1q antibody levels are correlated with disease severity in Chinese pediatric systemic lupus erythematosus. Rheumatol Int 2011;31:501-5. 760.Gilliam BE, Ombrello AK, Burlingame RW, Pepmueller PH, Moore TL. Measurement of Autoantibodies in Pediatric-Onset Systemic Lupus Erythematosus and Their Relationship with Disease-Associated Manifestations. Semin Arthritis Rheum 2011. 761.Brunner HI, Mueller M, Rutherford C, et al. Urinary neutrophil gelatinase-associated lipocalin as a biomarker of nephritis in childhood-onset systemic lupus erythematosus. Arthritis Rheum 2006;54:2577-84. 762.Suzuki M, Wiers K, Brooks EB, et al. Initial validation of a novel protein biomarker panel for active pediatric lupus nephritis. Pediatr Res 2009;65:530-6. 763.Marks SD, Pilkington C, Woo P, Dillon MJ. The use of the British Isles Lupus Assessment Group (BILAG) index as a valid tool in assessing disease activity in childhood-onset systemic lupus erythematosus. Rheumatology (Oxford) 2004;43:1186-9. 764.Hoftman AD, Tai LQ, Tze S, Seligson D, Gatti RA, McCurdy DK. MAGE-B2 autoantibody: a new biomarker for pediatric systemic lupus erythematosus. J Rheumatol 2008;35:2430-8. 765.Hinze CH, Suzuki M, Klein-Gitelman M, et al. Neutrophil gelatinase-associated lipocalin is a predictor of the course of global and renal childhood-onset systemic lupus erythematosus disease activity. Arthritis Rheum 2009;60:2772-81. 766.Suzuki M, Wiers KM, Klein-Gitelman MS, et al. Neutrophil gelatinase-associated lipocalin as a biomarker of disease activity in pediatric lupus nephritis. Pediatr Nephrol 2008;23:403-12. 767.Chien JW, Chen WL, Tsui YG, Lee MC, Lin AY, Lin CY. Daily urinary interleukin-11 excretion correlated with proteinuria in IgA nephropathy and lupus nephritis. Pediatr Nephrol 2006;21:490-6. 768.Marks SD, Shah V, Pilkington C, Tullus K. Urinary monocyte chemoattractant protein-1 correlates with disease activity in lupus nephritis. Pediatr Nephrol 2010;25:2283-8. 769.Suzuki M, Ross GF, Wiers K, et al. Identification of a urinary proteomic signature for lupus nephritis in children. Pediatr Nephrol 2007;22:2047-57. 770.Ezzat M, El-Gammasy T, Shaheen K, Shokr E. Elevated production of serum B-cell-attracting chemokine-1 (BCA-1/CXCL13) is correlated with childhood-onset lupus disease activity, severity, and renal involvement. Lupus 2011;20:845-54. 771.Apenteng T, Kaplan B, Meyers K. Renal outcomes in children with lupus and a family history of autoimmune disease. Lupus 2006;15:65-70. 772.Ataei N, Haydarpour M, Madani A, et al. Outcome of lupus nephritis in Iranian children: prognostic significance of certain features. Pediatr Nephrol 2008;23:749-55. 773.Coleman WP, 3rd, coleman WP, Derbes VJ, Jolly HW, Jr., Nesbitt LT, Jr. Collagen disease in children. A review of 71 cases. Jama 1977;237:1095-100. 774.Hersh AO, Trupin L, Yazdany J, et al. Childhood-onset disease as a predictor of mortality in an adult cohort of patients with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2010;62:1152-9. 54 775.Hiraki LT, Benseler SM, Tyrrell PN, Hebert D, Harvey E, Silverman ED. Clinical and laboratory characteristics and long-term outcome of pediatric systemic lupus erythematosus: a longitudinal study. J Pediatr 2008;152:550-6. 776.Khoo JJ, Pee S, Thevarajah B, Yap YC, Chin CK. Lupus nephritis in children in Malaysia. J Paediatr Child Health 2005;41:31-5. 777.Tejani A, Nicastri AD, Chen CK, Fikrig S, Gurumurthy K. Lupus nephritis in black and Hispanic children. Am J Dis Child 1983;137:481-3. 778.Vachvanichsanong P, Dissaneewate P, Lim A, McNeil E. Childhood Acute Renal Failure: 22-Year Experience in a University Hospital in Southern Thailand. Pediatrics 2006. 779.Yang LY, Chen WP, Lin CY. Lupus nephritis in children--a review of 167 patients. Pediatrics 1994;94:335-40. 780.Taheri S, Beiraghdar F. Lupus nephritis in Iranian children: a review of 60 patients. Ren Fail 2011;33:499-505. 781.Gutierrez-Suarez R, Ruperto N, Gastaldi R, et al. A proposal for a pediatric version of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index based on the analysis of 1,015 patients with juvenile-onset systemic lupus erythematosus. Arthritis Rheum 2006;54:2989-96. 782.Gibson KL, Gipson DS, Massengill SA, et al. Predictors of relapse and end stage kidney disease in proliferative lupus nephritis: focus on children, adolescents, and young adults. Clin J Am Soc Nephrol 2009;4:1962-7. 783.Lau KK, Jones DP, Hastings MC, Gaber LW, Ault BH. Short-term outcomes of severe lupus nephritis in a cohort of predominantly African-American children. Pediatr Nephrol 2006;21:655-62. 784.Lau KK, Jones DP, Ault BH. Prognosis of lupus membranous nephritis in children. Lupus 2007;16:70. 785.Wang LC, Yang YH, Lu MY, Chiang BL. Retrospective analysis of the renal outcome of pediatric lupus nephritis. Clin Rheumatol 2004;23:318-23. 786.Wong SN, Chan WK, Hui J, et al. Membranous lupus nephritis in Chinese children--a case series and review of the literature. Pediatr Nephrol 2009;24:1989-96. 787.Pereira T, Abitbol CL, Seeherunvong W, et al. Three decades of progress in treating childhood-onset lupus nephritis. Clin J Am Soc Nephrol 2011;6:2192-9. 788.Wang LC, Yang YH, Lu MY, Chiang BL. Retrospective analysis of mortality and morbidity of pediatric systemic lupus erythematosus in the past two decades. J Microbiol Immunol Infect 2003;36:203-8. 789.Massengill SF, Hedrick C, Ayoub EM, Sleasman JW, Kao KJ. Antiphospholipid antibodies in pediatric lupus nephritis. Am J Kidney Dis 1997;29:355-61. 790.Hiraki LT, Lu B, Alexander SR, et al. End-stage renal disease due to lupus nephritis among children in the US, 1995-2006. Arthritis Rheum 2011;63:1988-97. 791.Sule SD, Fadrowski JJ, Fivush BA, Gorman G, Furth SL. Reduced albumin levels and utilization of arteriovenous access in pediatric patients with systemic lupus erythematosus (SLE). Pediatr Nephrol 2007;22:2041-6. 792.Sule SD, Fadrowski JJ, Fivush BA, Neu AM, Furth SL. Persistent low albumin and temporary vascular access in pediatric patients with SLE on hemodialysis. Pediatr Nephrol 2009;24:1981-7. 793.Bartosh SM, Fine RN, Sullivan EK. Outcome after transplantation of young patients with systemic lupus erythematosus: a report of the North American pediatric renal transplant cooperative study. Transplantation 2001;72:973-8. 794.Gipson DS, Ferris ME, Dooley MA, Huang K, Hogan SL. Renal transplantation in children with lupus nephritis. Am J Kidney Dis 2003;41:455-63. 795.Garin EH, Sleasman JW, Richard GA, Iravani AA, Fennell RS. Pulsed methylprednisolone therapy compared to high dose prednisone in systemic lupus erythematosus nephritis. Eur J Pediatr 1986;145:380-3. 796.Hobbs DJ, Barletta GM, Rajpal JS, et al. Severe paediatric systemic lupus erythematosus nephritis--a single-centre experience. Nephrol Dial Transplant 2010;25:457-63. 797.Tanaka Y, Yoshikawa N, Hattori S, et al. Combination therapy with steroids and mizoribine in juvenile SLE: a randomized controlled trial. Pediatr Nephrol 2010;25:877-82. 798.Tanaka H, Tsugawa K, Oki E, Suzuki K, Ito E. Mizoribine intermittent pulse protocol for induction therapy for systemic lupus erythematosus in children: an open-label pilot study with five newly diagnosed patients. Clin Rheumatol 2008;27:85-9. 799.Yoshidome K, Takei S, Imanaka H, Maeno N, Ohkawa T, Kawano Y. Efficacy of mizoribine in the treatment of systemic lupus erythematosus in children. Pediatr Int 2004;46:444-9. 800.Hagge WW, Burke EC, Stickler GB. Treatment of systemic lupus erythematosus complicated by nephritis in children. Pediatrics 1967;40:822-7. 801.Barron KS, Person DA, Brewer EJ, Jr., Beale MG, Robson AM. Pulse methylprednisolone therapy in diffuse proliferative lupus nephritis. J Pediatr 1982;101:137-41. 802.Lau KK, Ault BH, Jones DP, Butani L. Induction therapy for pediatric focal proliferative lupus nephritis: cyclophosphamide versus mycophenolate mofetil. J Pediatr Health Care 2008;22:282-8. 55 803.Barbano G, Gusmano R, Damasio B, et al. Childhood-onset lupus nephritis: a single-center experience of pulse intravenous cyclophosphamide therapy. J Nephrol 2002;15:1239. 804.Fu LW, Yang LY, Chen WP, Lin CY. Clinical efficacy of cyclosporin a neoral in the treatment of paediatric lupus nephritis with heavy proteinuria. Br J Rheumatol 1998;37:217-21. 805.Al Salloum AA. Cyclophosphamide therapy for lupus nephritis: poor renal survival in Arab children. Pediatr Nephrol 2003;18:357-61. 806.Baskin E, Ozen S, Cakar N, Bayrakci US, Demirkaya E, Bakkaloglu A. The use of low-dose cyclophosphamide followed by AZA/MMF treatment in childhood lupus nephritis. Pediatr Nephrol 2010;25:111-7. 807.Chiu SJ, Ou LS, Tsai TL, Hung IJ, Huang JL. Sequential evaluation of clinical and laboratory changes amongst children suffering from lupus nephritis during intermittent intravenous cyclophosphamide therapy. Clin Rheumatol 2006;25:515-9. 808.Dixit MP, Bracamonte E, Dixit N. Intravenous cyclophosphamide--resistant systemic lupus erythematosus in Arizona. Pediatr Nephrol 2004;19:738-43. 809.Lehman TJ, Sherry DD, Wagner-Weiner L, et al. Intermittent intravenous cyclophosphamide therapy for lupus nephritis. J Pediatr 1989;114:1055-60. 810.Lehman TJ, Onel K. Intermittent intravenous cyclophosphamide arrests progression of the renal chronicity index in childhood systemic lupus erythematosus. J Pediatr 2000;136:243-7. 811.Opastirakul S, Chartapisak W. Pulse cyclophosphamide induction treatment in Thai children with diffuse proliferative lupus nephritis. Nephrology (Carlton) 2011. 812.Tanaka H, Tateyama T, Waga S. Methylprednisolone pulse therapy in Japanese children with severe lupus nephritis. Pediatr Nephrol 2001;16:817-9. 813.Vachvanichsanong P, Dissaneewate P, Winn T. Intravenous cyclophosphamide for lupus nephritis in Thai children. Scand J Rheumatol 2004;33:339-42. 814.Falcini F, Capannini S, Martini G, et al. Mycophenolate mofetil for the treatment of juvenile onset SLE: a multicenter study. Lupus 2009;18:139-43. 815.Kazyra I, Pilkington C, Marks SD, Tullus K. Mycophenolate mofetil treatment in children and adolescents with lupus. Arch Dis Child 2010;95:1059-61. 816.Tanaka H, Oki E, Tsuruga K, Yashiro T, Hanada I, Ito E. Management of young patients with lupus nephritis using tacrolimus administered as a single daily dose. Clin Nephrol 2009;72:430-6. 817.Tanaka H, Nakahata T, Tsugawa K, Tsuruga K, Yumura W, Ito E. Mizoribine pulse therapy for patients with flares of lupus nephritis: a 1-year observation. Clin Nephrol 2004;62:165-6. 818.Tanaka H, Oki E, Tsugawa K, Nonaka K, Suzuki K, Ito E. Effective treatment of young patients with pediatric-onset, long-standing lupus nephritis with tacrolimus given as a single daily dose: an open-label pilot study. Lupus 2007;16:896-900. 819.Nathanson S, Salomon R, Ranchin B, et al. Prognosis of lupus membranous nephropathy in children. Pediatr Nephrol 2006;21:1113-6. 820.Buratti S, Szer IS, Spencer CH, Bartosh S, Reiff A. Mycophenolate mofetil treatment of severe renal disease in pediatric onset systemic lupus erythematosus. J Rheumatol 2001;28:2103-8. 821.Baca V, Catalan T, Villasis-Keever M, Ramon G, Morales AM, Rodriguez-Leyva F. Effect of low-dose cyclosporine A in the treatment of refractory proteinuria in childhoodonset lupus nephritis. Lupus 2006;15:490-5. 822.Ravelli A, Ballardini G, Viola S, Villa I, Ruperto N, Martini A. Methotrexate therapy in refractory pediatric onset systemic lupus erythematosus. J Rheumatol 1998;25:572-5. 823.Lehman TJ, Edelheit BS, Onel KB. Combined intravenous methotrexate and cyclophosphamide for refractory childhood lupus nephritis. Ann Rheum Dis 2004;63:321-3. 824.Lin CY, Hsu HC, Chiang H. Improvement of histological and immunological change in steroid and immunosuppressive drug-resistant lupus nephritis by high-dose intravenous gamma globulin. Nephron 1989;53:303-10. 825.Tanaka H, Tsugawa K, Suzuki K, Nakahata T, Ito E. Long-term mizoribine intermittent pulse therapy for young patients with flare of lupus nephritis. Pediatr Nephrol 2006;21:962-6. 826.Tanaka H, Suzuki K, Nakahata T, Sato T, Ito E. Mizoribine oral pulse therapy for a patient with severe lupus nephritis. Pediatr Int 2003;45:488-90. 827.Nwobi O, Abitbol CL, Chandar J, Seeherunvong W, Zilleruelo G. Rituximab therapy for juvenile-onset systemic lupus erythematosus. Pediatr Nephrol 2008;23:413-9. 828.Podolskaya A, Stadermann M, Pilkington C, Marks SD, Tullus K. B cell depletion therapy for 19 patients with refractory systemic lupus erythematosus. Arch Dis Child 2008;93:401-6. 829.Willems M, Haddad E, Niaudet P, et al. Rituximab therapy for childhood-onset systemic lupus erythematosus. J Pediatr 2006;148:623-7. 56 830.Jordan SC, Ho W, Ettenger R, Salusky IB, Fine RN. Plasma exchange improves the glomerulonephritis of systemic lupus erythematosus in selected pediatric patients. Pediatr Nephrol 1987;1:276-80. 831.Wright EC, Tullus K, Dillon MJ. Retrospective study of plasma exchange in children with systemic lupus erythematosus. Pediatr Nephrol 2004;19:1108-14. 57