File - Casey Coon Family Nurse Practitioner
advertisement

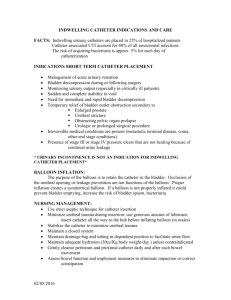
Running head: Post- Operative Orthopedic Patients and Voiding Post-Operative Orthopedic Patients and Voiding Casey L Cleveland SUNY IT NUR 560 Nursing Research Methods Professor Woodhouse 1 Post-Operative Orthopedic Patients and Voiding 2 Post-Operative Orthopedic Patients and Voiding Background of the Problem The background of this research problem is from clinical experience on a 35 bed medical surgical floor. There have been multiple instances where post-operative orthopedic patients have had difficulties voiding and have had to be straight catheterized to empty their bladder. In some instances, the patient has had to be straight catheterized more than once after the initial catheterization, and this is troubling, because as with any invasive procedure, there is always a risk of introducing infection. Hansen, Soreide, Warland & Nilsen (2011) found that post-operative urinary retention is dangerous if unrelieved because it can permanently damage urinary function. There is an increase of a risk of urinary retention as a patient gets older and there seems to be a higher incidence in men. They also state that from their extensive review, it is apparent that more knowledge is required about urinary retention in postoperative patients (p. 545). “Nationally, approximately 20% of all hospital-acquired infections are urinary tract infections, with an estimated 80% of these being linked to urinary catheters” (Dailly, 2011). “It has been estimated that the risk of bacteriuria in catheterised patients increases by 3-10% per day every day the catheter remains in situ and 50% of patients with a catheter in place for ten days will have a bacteriuria. Patients who develop a hospital-acquired infection can expect to remain in hospital two and a half times longer, and incur higher hospital and community costs, than non-infected patients” (Dailly, 2011). “Indwelling urinary catheters are associated with significant mortality and morbidity, and should be avoided or used for the minimum time possible. The greatest risk factor for contracting a urinary tract infection is having a urinary catheter; once inserted, the longer the duration of catheterisation the greater the risk of infection. Therefore using alternative urine collection strategies Post-Operative Orthopedic Patients and Voiding 3 when appropriate and reducing the duration of catheterisation are critical in the prevention of urinary tract infections” (Dailly, 2011). Problem Statement The problem is that orthopedic patients often have a difficult time voiding after surgery, and nurses are forced to subject the patient to a risk for infection by straight catheterizing them. Complicating this issue in this situation is the fact that the patient has already been subjected to a risk of infection through their orthopedic surgery, and then we are again subjecting the patient to a risk for infection with the introduction of a catheter into the bladder. Johansson & Christensson (2010), state the incidence of urinary retention is as high as 56% after hip fracture surgery in older adults (p. 2110). The risk for difficult time voiding is being found in both the older population as well as the younger population. However, the older population is usually more susceptible to infection than the young population. Purpose The purpose for this study is to determine if a post- operative orthopedic patient cannot void on their own, in a specific time frame, is it safe to perform multiple straight catheterizations or would there be a high rate of infection with this practice? If a straight catheterization is performed multiple times, is it safer practice to insert an indwelling catheter for a specific amount of time? In a past study, the authors researched if there was a higher incidence of urinary tract infection when an older patient who had a hip fracture was intermittently catheterized or had an indwelling catheter after surgery, and the results they found was that there was a higher incidence of infection if the catheter was indwelling Post-Operative Orthopedic Patients and Voiding 4 (61% for indwelling, compared to 32% for intermittent) (Johansson, Athlin, Frykholm, Bolinder & Larsson, 2001). The purpose of this study is to determine if the infection rate is lower if we straight catheterize or use an indwelling catheter. Significance The significance of this problem is that post-operative orthopedic patients would benefit from a lower infection rate if it was known which catheterization had the lowest incidence of infection. The patient has already been subjected to major surgery, which has a risk of infection on its own, and then when the patient cannot void on their own, they are subjected to a risk of infection again. “The use of urethral catheters has become increasingly common. Each year over 30 million urinary catheters are inserted in hospitalized patients. On average 3–10% of these patients will develop asymptomatic bacteriuria per day. Twenty-five percent of patients with bacteriuria develop a symptomatic urinary tract infection, and approximately 3% develop bacteremia” (Winter, Helms, Harrington, Luquire, McVay & Rhodes, p. 8, 2009). “Indwelling urinary catheters can cause trauma, affect long-term bladder function, and increase the risk of infection. They can be painful and uncomfortable and can restrict physical activity” (Nazarko, p. 948, 2010). “Intermittent catheterization is preferable to indwelling urethral or suprapubic catheters in patients with bladder emptying dysfunction” (Buchmann & Stinnett, p. 5, 2011). This study is important because there is a high rate of infection associated with catheter use, and the practice with the lowest rate of infection should be used for these post-operative orthopedic patients who are having a difficult time voiding on their own. Post-Operative Orthopedic Patients and Voiding 5 Research Questions The research questions for this study are: If a straight catheterization is to be performed multiple times, is there less of an infection rate to insert an indwelling catheter for a specific amount of time? What are the infection rates for straight catheterizing multiple times vs. the infection rate of inserting an indwelling catheter for a short time? Hypothesis The hypothesis for this experimental study is that the infection rate is lower when performing straight catheterizations compared to indwelling urinary catheterization. Even if the straight catheterization is performed multiple times, it still has a lower infection rate associated with it compared to the infection rate of indwelling catheterization. Definitions The independent variable for this study is using a straight catheter or an indwelling catheter. “In research, an independent variable is the cause or influencing variable” (Woods & Ross-Kerr, 2010, p. 101). The dependent variable for this study is infection rates for the 2 different catheterizations. A dependent variable is “affected by the independent variables, is the effect, and comes later or last” (Woods & Ross-Kerr, 2010, p. 102). Theoretical Framework The framework that is most closely related to the research is Orem’s Self-Care Theory. This theory is associated with life processes and the ability for a person to care for himself. Since the people Post-Operative Orthopedic Patients and Voiding 6 in these studies are having difficulty voiding, they are unable to take care for one of their basic needs; eliminating waste. Orem’s Self-Care Theory would be of good use to this proposed study, as the patient is unable to care for himself at this point in his life (Current Nursing, 2012). According to Orem, she stated the following in her theory: “The condition that validates the existence of a requirement for nursing in an adult is the health-associated absence of the ability to maintain continuously that amount and quality of self-care that is therapeutic in sustaining life and health, in recovering from disease or injury, or in coping with their effects. With children, the condition is the inability of the parent (or guardian) associated with the child's health state to maintain continuously for the child the amount and quality of care that is therapeutic." (Orem, 2001, p. 82) According to Sitzman & Eichelberger (2011), "Orem's Self-Care Model describes a structure wherein the nurse assists the client, where needed, to maintain an adequate level of self-care. The degree of nursing care and intervention depends on the degree to which the client is able (or unable) to meet self-care needs (p. 96)." In this case, where the patient cannot void on their own, they cannot care for one of their basic needs by themselves, and the nurse must step in and help them achieve their needs. One research article that uses Orem’s self-care theory as a focus is Allison’s self-care requirements for activity and rest with an Orem nursing focus. Allison states “According to Orem’s self-care deficit nursing theory, helping people to maintain a balance between activity and rest (a universal self-care requisite) is a legitimate concern of nursing. The meaning of activity and rest, the requirements and potential measures for meeting this self-care requisite, and factors that might influence the process are explored. Criteria for determining a need for nursing, guides for a nursing clinical assessment, and guides for nursing action are suggested as potential ways to assist persons to meet the action demands associated with this self-care requisite” (p. 68, 2007). Allison used this theory to explain the importance of rest and activity for a person’s self-care. A case study by Berbiglia used Orem’s self- care deficit nursing theory (SCDNT) as a basis for a curriculum. “Due to the Post-Operative Orthopedic Patients and Voiding 7 widespread use of Orem's nursing theory in nursing programmes, SCDNT-based curriculum development is perhaps approaching its nadir…. the application of nursing theory to education and the continuous assessment of the resulting impact will give direction to nursing as a discipline in higher education as well as enhance the image of nursing” (Berbiglia, p. 1162, 1991). This study shows that Orem’s self-care deficit theory could be used as a framework for many research studies, including a research study about post-operative orthopedic patients who have a self-care deficit since they cannot void on their own. Literature Review Allison, S. (2008). Self-Care Requirements for Activity and Rest: An Orem Nursing Focus. Nursing Science Quarterly, 68-76. Doi:10.1177/0894318406296297 This article uses Dorothea Orem’s self-care deficit theory to explain the importance of activity and rest in keeping a person well. This article ties into the research study because it is similar to how Orem’s selfcare deficit theory can be tied to a patient being unable to void on their own. It is just as important for a patient to void as it is for a patient to have adequate time for activity and rest. Bernard, M.S., Hunter, K.F., & Moore, K.N. (2012). A review of strategies to decrease the duration of indwelling urethral catheters and potentially reduce the incidence of catheter-associated urinary tract infections. Urologic Nursing, 32(1), 29-37 This article explains that the use of indwelling catheters in hospitalized patients has increased risk of complications, including urinary tract infection caused by the use of the catheter. It also explains that by decreasing the duration of the use of the indwelling catheter, the rate of infection can be reduced. This Post-Operative Orthopedic Patients and Voiding 8 supports the research study in that an indwelling catheter may have a higher rate of infection compared to the use of intermittent catheters. Buchmann, B., & Stinnett, G. (2011). Reducing rates of catheter-associated urinary tract infection. The Alabama Nurse, 5. Retrieved from Medline with Full Text. This article explains that many hospitalized patients acquire an infection while they are being treated, and they are recommending best practice methods to reduce the rate of catheter-associated urinary tract infection. They state “For improvement of quality patient care, continual improvement and development of new best practice measures and/or reinforcement of current measures regarding urinary catheter care should be a priority for all clinicians”. This supports the research study in that there is a risk for infection when using a catheter and best practice measures should be followed, that may mean not choosing to use an indwelling catheter and using a straight catheterization instead. Dailly, S. (2011). Auditing urinary catheter care. Nursing Standard, 26(20), 35-40. Retrieved from Cinahl Plus. This author states “It has been estimated that the risk of bacteriuria in catheterised patients increases by 3-10% per day every day the catheter remains in situ and 50% of patients with a catheter in place for ten days will have a bacteriuria. Patients who develop a hospital-acquired infection can expect to remain in hospital two and a half times longer, and incur higher hospital and community costs, than noninfected patients”. With the information from this article, it would appear for the research study that an indwelling catheter would not be a good choice. Post-Operative Orthopedic Patients and Voiding 9 Dailly, S. (2011, March). Prevention of indwelling catheter-associated urinary tract infections. Nursing Older People, 23(2). Retrieved from Medline with Full Text. This article explains the best practice that should be used with indwelling urinary catheters in order to reduce the incidence of infection. This author states that approximately 20% of all healthcare associated infections are urinary tract infections, with an estimated 80% of those linked to urinary catheters. This article shows the relationship between UTIs and catheters, and is associated with the research study because there is a high rate of infection associated with catheters, and shows that great care should be taken if a catheter is to be used. Hameed, A., Chinegwundoh, F., & Thwaini, A. (2010). Prevention of catheter-related urinary tract infections. British Journal of Hospital Medicine, 71(3), 148-152. Retrieved from Cinahl Plus. This article states that there is a 5% risk for UTI each day a patient has a catheter indwelling. They also state that prophylactic antibiotic use should not be used, as it has not been shown to be effective. This article is important to the research study as it shows that an indwelling catheter is associated with a higher rate of infection. Hansen, B. S., Soreide, E., Warland, A. M., & Nilsen, O. B. (2011). Risk factors of post-operative urinary retention in hospitalised patients. Acta Anaesthesiologica Scandinavica, 55, 545-548. doi:10.1111/j.1399-6576.2011.02416.x This article explains about a quality improvement project that was completed because the post anesthesia care unit was finding patients were having urinary retention after surgery. They found that 13% of hospitalized post-operative patients had urinary retention. This article is important for this Post-Operative Orthopedic Patients and Voiding 10 research study as it shows that there is a risk for post-operative urinary retention in patients, who may need to use a catheter to relieve themselves. Johansson, I., Athlin, E., Frykholm, L., Bolinder, H., & Larsson, G. (2002). Intermittent versus indwelling catheters for older patients with hip fractures. Journal of Clinical Nursing, 11, 651-656. Retrieved from Cinahl Plus. This article states that avoiding routine use of indwelling catheters will lower the risk of infection for patients. This is important to the research study as it was a study performed of indwelling versus intermittent catheterizations, and their study showed that indwelling catheters should not be used over intermittent. Johansson, R., & Christenssen, L. (2010). Urinary retention in older patients in connection with hip fracture surgery. Journal of Clinical Nursing, 19, 2110-2116.doi:10.1111/j.1365-2702.2010.03261.x This article showed that older patients who have had orthopedic surgery have difficulties with urinary retention after surgery. This is important for the research study as it shows that it is a pertinent problem that needs to be studied. The authors also state “The patients who were treated with intermittent catheterisation had had voiding satisfaction earlier and had not had repeated urinary retention compared to patients with indwelling urethral catheter.” This is consistent with the other findings for the research study. Johnson, R., Kuskowski, M., & Wilt, T. (2006). Systematic Review: Antimicrobial Urinary Catheters to Prevent Catheter-Associated Urinary Tract Infection in Hospitalized Patients. Annals of Internal Medicine, 144(2), 116-126. Retrieved from Medline with Full Text. Post-Operative Orthopedic Patients and Voiding 11 This article reviewed using antimicrobial catheters in order to prevent infection, and they found that these antimicrobial catheters can prevent or delay UTI, but it varies greatly with other variables included. This is helpful for the research study as it shows that even with antimicrobial catheters, indwelling catheters still have a high rate of infection associated with them and should be used minimally. Luger, T. J., Garoscio, I., Rehder, P., Oberladstatter, J., & Voelckel, W. (2008). Management of temporary urinary retention after arthroscopic knee surgery in low-dose spinal anesthesia: development of a simple algorithm. Archives of Orthopaedic & Trauma Surgery, 607-612. Doi: 10.1007/s00402-007-0481-x The purpose of this quantitative study was “to identify parameters indicative of urinary retention after low-dose spinal anesthesia and to develop a simple algorithm for patient care” (Luger etc., 2008). They then measured the incidence of spontaneous urination versus urinary catheterization. Their results were that 70% of the patients were able to void on their own; and in the 30% who had to be catheterized due to their bladder retaining over 500ml or they urinated insufficiently. This article is important to the research study because it shows the incidence of urinary retention after orthopedic surgery. Nazarko, L. (2008). Reducing the risk of catheter-related urinary tract infection. British Journal of Nursing, 17(16), 1002-1010. Retrieved from Medline with Full Text. This article explains that even routine medical interventions such as a urinary catheter put patients at a risk for infection. This author states that about 12-26% of patients may have a urinary catheter while in the hospital and 80% of urinary tract infections are caused by catheters. These numbers indicate that it is not ideal to use a urinary catheter, however, sometimes, such as when a post-operative patient Post-Operative Orthopedic Patients and Voiding 12 cannot void on their own, it is necessary. This supports the research study in that using a catheter can cause an infection for our patients. Orem, D., & Taylor, S. (2011). Reflections on Nursing Practice Science: The Nature, the Structure, and the Foundation of Nursing Sciences. Nursing Science Quarterly, 24(1), 35-41. doi:DOI: 10.1177/0894318410389061 This author states “The continuing development of practical nursing sciences moving from the foundations for the science established by nurses’ use of the self-care deficit nursing theory is dependent upon nurses’ ability to think nursing.” This is important to the research study as due to the rates of infection with catheter use, and patients having a self-care deficit from not being able to void on their own, this article would be a good resource for the nurse caring for the patient. Parker, L. (1999). Urinary catheter management: minimizing the risk of infection. British Journal of Nursing, 8(9). Retrieved from Medline with Full Text. This article was written by an infection control nurse who wrote this article about the care of catheters and how to minimize the risk of infection if the patient does need a catheter. This article explains the anatomy of the urinary system and the different kinds of urinary catheters. It explains that there is a high risk of infection associated with catheters, and many nurses are not educated on the proper care and selection of correct equipment. This author states that when a catheter is used it should have a scientific basis and show in the education and training of the nurses who will be caring for the catheter. This article can be used in this research study because it supports the idea that there is an increased risk of infection when using a catheter and serious thought needs to be put into using one. Post-Operative Orthopedic Patients and Voiding 13 Sherburne, E., & Sawin, K. (2008, January). Investigating Time to Void After Lower-Extremity Orthopedic Surgery in a Pediatric Population. Journal for Specialists in Pediatric Nursing, 13(1), 36-47. Retrieved from Cinahl Plus. The purpose of this quantitative study was to determine the time frame of post- operative bladder volume in order to assess children who were at risk for urinary retention in a pediatric orthopedic population. They used a convenience sample of 38 children (ages 4-17) who had lower extremity orthopedic surgery. The results of the study are that 71% of the children spontaneously voided, while the rest of the children (29%) required straight catheterization. They also found that the general rule of waiting 8 hours post-surgery to assess the signs of urinary retention was too long for pediatric patients, and it should be lowered to 4-6 hours post-operatively. This study is important related to the research question as it can help to examine the differences between pediatric and adult post- operative orthopedic patients and their likelihood that they will need to be straight catheterized. Wilson, M. (2011). Addressing the problems of long- term urethral catheterization: part 1. British Journal of Nursing, 20(22), 1418-1424. Retrieved from Medline with Full Text. This author states “Indwelling catheters should only be used in the absence of alternative methods of management, their use reviewed regularly and removed as soon as possible”. This shows how dangerous indwelling catheters can be to patients, and is important to the research study to show that intermittent catheterizations are the preferred method of catheterization. Methodology The design of this specific research study is a descriptive research design, and the setting is medical surgical floors of 3 area hospitals that care for post-operative orthopedic patients. The ethical Post-Operative Orthopedic Patients and Voiding 14 considerations are ensuring that nurses are not needlessly using catheters on patients who can void on their own. The only time a catheter can be used is post-operatively if a patient cannot void. A consent form would need to be signed by the patient before surgery, consenting that if they cannot void on their own either an intermittent or indwelling catheter will be used to relieve them. It will be chosen randomly which patient gets an intermittent catheter or an indwelling catheter, and infection rates will be assessed. The population is any adult that is post-operative and has had an orthopedic surgery done. This may include adult male and female patients of various ages. Every patient who has an orthopedic surgery done will be followed, and if they have trouble voiding, it will be a random decision if they require an intermittent or indwelling catheter. The data will be collected by a research assistant who will speak to the nurses who are caring for the patients and let them know which patient will receive an intermittent catheter or an indwelling catheter if they cannot void. The research assistant will then follow the patient to determine the rate of infection for intermittent VS. indwelling catheters. The research assistant will keep a chart of his findings and this will be kept to be analyzed after all of the data has been collected. The reliability of this study is good, as the research assistant will attempt to eliminate or minimize error by speaking with the nurses and ensuring that they are using proper sterile technique. This should also keep the findings valid, as each nurse will ensure that aseptic technique so this will not misconstrue the infection rate. The results that are obtained from these studies should be stable, credible and accurate. Although the results will only be from 3 local hospitals, researchers can use this to project the results that might be obtained from most hospitals in the US. The results that are obtained will be analyzed by determining the infection rates of the straight catheterizations as well as the indwelling catheters. These infection rates will be compared, and from this analysis it can be determined which practice has a lower infection rate and should be used after surgery for orthopedic patients who are having a difficult time voiding. Post-Operative Orthopedic Patients and Voiding 15 References Allison, S. (2008). Self-Care Requirements for Activity and Rest: An Orem Nursing Focus. Nursing Science Quarterly, 68-76. doi:10.1177/0894318406296297 Berbiglia, V. (1991). A case study: perspectives on a self-care deficit nursing theory-based curriculum. Journal of Advanced Nursing, 16, 1158-1163. Retrieved from Medline with Full Text. Bernard, M.S., Hunter, K.F., & Moore, K.N. (2012). A review of strategies to decrease the duration of indwelling urethral catheters and potentially reduce the incidence of catheter-associated urinary tract infections. Urologic Nursing, 32(1), 29-37 Buchmann, B., & Stinnett, G. (2011). Reducing rates of catheter-associated urinary tract infection. The Alabama Nurse, 5. Retrieved from Medline with Full Text. Current Nursing. (2012). Dorothea Orem's Self-Care Theory. Nursing Theories. Retrieved from http://currentnursing.com/nursing_theory/self_care_deficit_theory.html Dailly, S. (2011). Auditing urinary catheter care. Nursing Standard, 26(20), 35-40. Retrieved from Cinahl Plus. Dailly, S. (2011, March). Prevention of indwelling catheter-associated urinary tract infections. Nursing Older People, 23(2). Retrieved from Medline with Full Text. Hameed, A., Chinegwundoh, F., & Thwaini, A. (2010). Prevention of catheter-related urinary tract infections. British Journal of Hospital Medicine, 71(3), 148-152. Retrieved from Cinahl Plus. Post-Operative Orthopedic Patients and Voiding 16 Hansen, B. S., Soreide, E., Warland, A. M., & Nilsen, O. B. (2011). Risk factors of post-operative urinary retention in hospitalised patients. Acta Anaesthesiologica Scandinavica, 55, 545-548. doi:10.1111/j.1399-6576.2011.02416.x Johansson, I., Athlin, E., Frykholm, L., Bolinder, H., & Larsson, G. (2002). Intermittent versus indwelling catheters for older patients with hip fractures. Journal of Clinical Nursing, 11, 651-656. Retrieved from Cinahl Plus. Johansson, R., & Christenssen, L. (2010). Urinary retention in older patients in connection with hip fracture surgery. Journal of Clinical Nursing, 19, 2110-2116. doi:10.1111/j.13652702.2010.03261.x Johnson, R., Kuskowski, M., & Wilt, T. (2006). Systematic Review: Antimicrobial Urinary Catheters to Prevent Catheter-Associated Urinary Tract Infection in Hospitalized Patients. Annals of Internal Medicine, 144(2), 116-126. Retrieved from Medline with Full Text. Luger, T. J., Garoscio, I., Rehder, P., Oberladstatter, J., & Voelckel, W. (2008). Management of temporary urinary retention after arthroscopic knee surgery in low-dose spinal anesthesia: development of a simple algorithm. Archives of Orthopaedic & Trauma Surgery, 607-612. Doi: 10.1007/s00402007-0481-x Nazarko, L. (2008). Reducing the risk of catheter-related urinary tract infection. British Journal of Nursing, 17(16), 1002-1010. Retrieved from Medline with Full Text. Orem, D. E. (2001). Nursing: Concepts and Practice (6th ed.). St. Louis, MO: Mosby. Post-Operative Orthopedic Patients and Voiding 17 Orem, D., & Taylor, S. (2011). Reflections on Nursing Practice Science: The Nature, the Structure, and the Foundation of Nursing Sciences. Nursing Science Quarterly, 24(1), 35-41. doi: 10.1177/0894318410389061 Parker, L. (1999). Urinary catheter management: minimizing the risk of infection. British Journal of Nursing, 8(9). Retrieved from Medline with Full Text. Sitzman, K. L. & Eichelberger, L. W. (2011). Understanding the Works of Nurse Theorists: A Creative Beginning (2nd ed.). Sudbury, MA: Jones and Barlett Learning, LLC. Sherburne, E., & Sawin, K. (2008, January). Investigating Time to Void After Lower-Extremity Orthopedic Surgery in a Pediatric Population. Journal for Specialists in Pediatric Nursing, 13(1), 36-47. Retrieved from Cinahl Plus. Wilson, M. (2011). Addressing the problems of long- term urethral catheterization: part 1. British Journal of Nursing, 20(22), 1418-1424. Retrieved from Medline with Full Text. Wood, M. J. & Ross-Kerr, J. C. (2011). Basic steps in planning nursing research: From question to proposal. (7th ed.). Sudbury, MA: Jones & Bartlett.