Supplemental Material I

Supplemental Material I
Supporting Evidence for Environmental Mediated Transmission and
Model Parameterization
To perform exposure assessment of an ICU hospital environment, we used an environmental infection transmission system (EITS) framework that allows incorporation of pathogen, environment, patients and healthcare workers in the same system. Here, we provided supporting evidence for the parameterization of the following environmental processes: 1)
Staphylococcus aureus ( S. aureus ) shed into the environment; 2) S. aureus survivability in the environment and on hands; 3) contacts between hands and surfaces, and between fingertips and noses; and 4) S. aureus transferred between the two contacting surfaces (porous and nonporous).
S1. S. aureus shed to the environment continuously and sometimes profusely
S. aureus is a common human commensal organism. Its ecological niche is in the anterior nares, in the throat, in the gastrointestinal tract, and on the skin at numerous body parts including
perineum, axilla, and wounds [1]. It can also be found ubiquitously in hospital environment on
various surfaces, including floors, carpets, bed linens, bed frames, over-bed tables, blood
Studies in 1956 and 1958 showed that the major route of its spread was due to the release
of pathogen from the skin into air [4, 5]. Little was spread by other routes such as 1) expulsion
via respiratory droplets from the nose, 2) contamination of nasal discharge onto hands, 3) excretion in the feces [1, 2]. By the early 1960s, much attention was focused on the ability of S.
1
aureus to disperse into air, but the underlying mechanism was unclear. There were questions of whether S. aureus
could float freely in the air or attach to textile fibers [6]. Skin scales were
found in the air as early as 1855, and the possibility that they could carry organisms was suggested in 1905. But not until 1962 was it discovered that these desquamated skin scales carry
most of the bacteria dispersed into the air in hospitals [6, 7].
The average human skin surface area is 1.75 m 2 . This surface area comprises approximately 2x10 9 skin scales. A complete layer of cells can be lost and replaced every 24 hours on average. Hence, at least 10 7
skin particles may be shed every day [8, 9]. It was
estimated that each airborne skin particle could carry four viable cocci of S. aureus
Several factors influence dispersal heterogeneity. First, the location of colonization can
affect the dispersal quantity. Perineal carriers tend to be heavy dispersers [5, 11, 12], while some
nasal carriers do not disperse at all. In one study, 62% of 87 nasal carriers dispersed S. aureus into air (13). Second, the skin conditions can also affect the dispersal quantity. Patients with
On the other hand, receiving decolonization or systemic antibiotic treatment for S. aureus can
S1.1 Shedding
Reported ranges in the amount of S. aureus dispersed are summarized in Table S1.
Airborne particles range in sizes from 4 to 20 μm with a median diameter of 14 (13-17) μm [18].
We assumed that the number of particles contained in 1 ft 3 of air is approximately equal to the number that settle on 1 ft 2
in 1 min, which is valid for the particle range we are interested in [19].
2
Therefore, in Table S1, the reported S. aureus air count is converted to the cfu/cm 2 /min for use in the model, assuming all S. aureus in the air completely settle on the horizontal surfaces. In our model, the value used for the shedding parameter was 1x10 -2 cfu/cm 2 /min, which is within the range of the experimental studies.
3
Table S1 . Summary of source literature for shedding parameter
Author/Year Study Design Subject Setting Method S.aureus
count
(cfu/cm 2 /min a )
Williams, 1967
Gehanno, 2009
Experimental study:
Results in this table is from the 5 th experiment
Experimental study
Experimental study
4-year environmental surveillance study in 3 male surgical wards
20-mo surveillance study
Experimental study
Environmental sampling study in hospital wards
3 S.aureus
nasal carriers and 2 non-carriers
19 nasal carriers and 7 non-carriers
127 subjects (staff, students, hospital inpatients, patients with skin diseases)
3,675 patients (1488 were S.aureus
nasal carriers on admission)
307 patients were admitted.
615 laboratory technicians, doctors and nurses: 238 males &377 females.
24 patients infected or colonized with MRSA.
Subjects were fully clothed and exercised for 15 minutes.
Each day subjects wore clothing and exercised in the cubicle.
Subjects undressed in a cubicle during a 2minutes period
Varied ward activities
Varied ward activities
Subjects moved arms and legs in a defined manner at a constant rate.
Patients were in their beds with no movement.
Settling plates in a cubicle
Settling plates in a cubicle
Air sampling through slit samplers of a cubicle
Air sampling through slit samplers for 2 h in wards
Settling plates in the rooms and corners of the ward
Air sampling in a test chamber for 2 min
Air sampling for 10 min, which represents 1 m 3
0.14 – 47.4 cfu/ft
(1.5x10
cfu/cm 2
-4 – 5x10 -2
/min)
2 /min
0 – 27.8 cfu/ft
(0 - 3x10 -2
2 /min
cfu/cm 2 /min)
0.25 – 100 cfu/ft
(1.3x10
-4 – 5x10
3
-2
/2min cfu/cm 2 /min)
0 – 3 cfu/ft 3
(0 – 3.2 x10
/min
-3 cfu/cm 2 /min)
0 – 700 cfu/ft 2 /h
(0 –1.3x10
-2 cfu/cm 2 /min)
0 – 2800 cfu/100 ft 3 /2min
(0 – 1.5x10
-2
/min) cfu/cm 2
1 – 78 cfu/m 3
(1x10 -5 cfu/cm 2
/10min
– 7.8x10
/min)
-4 a) We assumed that the number of microorganisms contained in 1 ft 3 of air is equal to the number that settle on 1 ft 2
in 1 minute [19]. One ft is 30.5
cm. One ft 2 is 930.25 cm 2 .
4
S2. S. aureus survives and remains viable on surfaces and hands for a long period of time
S. aureus is known to survive in a variety of environmental niches by virtue of its
adaptability and resistance to environmental stress [22, 23]. Studies showed that strains causing
epidemics had more prolonged survival than non-epidemic strains. Some staphylococci epidemic
strains may persist on surfaces for months [23-26]. The prolonged survivability of
S. aureus in the environment not only contributes to its ability to disseminate but also makes decontamination in the hospital environment both more difficult and more important.
S2.1 Survival parameter
Many studies have been performed to investigate the survival of various nosocomial
pathogens in hospital, household or in experimental settings [23, 27-33]. However, study
designs, study conditions, and the outcome measures were not all consistent. Measures used
included death rate per unit time [23, 27-29], amount changes or % recovery over time [30-32],
and survival time in days [33]. We selected references with quantitative measures that allow
calculation of the die-off rate (μ) based on the initial and final concentrations over time as shown
μ = 𝑙𝑜𝑔
10
(𝑀
0
) − 𝑙𝑜𝑔
10
(𝑀 𝑡
)
𝑇 𝑠𝑢𝑟𝑣𝑖𝑣𝑎𝑙 where, M t
is 𝑀 𝑜
∗ 10 −μ𝑡 (S1)
S2.2 Survival on porous surfaces
A study was performed to evaluate S. aureus survival on contaminated standardized
sterile fabrics, commonly used in dental clinics [34]. These results suggested that
S. aureus could
5
survive 3-7 days on surfaces including cotton/polyester fabric and paper. Based on these data, we estimated the die-off rate for cotton/polyester fabric as 0.000632 log cfu/min and used it as porous surface die-off rate in our model.
S2.3 Survival on nonporous surfaces
Laboratory experiments on decay rates of six different nonporous surfaces found a much higher level of inactivation using a culture method in comparison to a quantitative PCR method
[29]. From this study, we used the decay rate by culture method on plastic, which was measured
as 0.012 log cfu/h (0.0002 log cfu/min).
S2.4 Survival on hands and skin
One study that involved application of S. aureus on to four volunteers’ fingertips found
that the greatest pathogen loss happened in the first five minutes [31]. The author concluded that
the loss was due to desiccation. After the initial five minutes, the decline was less pronounced.
Here, we used the data of this second phase (after the initial five minutes) assuming a first order decay. The die off rate on fingertips was estimated as 0.00353 log cfu/min in the study mentioned above, and the same was used in our model.
Despite being a commensal organism on skin, S. aureus survives for shorter period of time on hands compared to surfaces. This characteristic is not unique to S. aureus ; other nosocomial pathogens such as Candida species, enterococci, or Klebsiella also have shorter
survival on hands than on surfaces [35-37].
S3. S. aureus picked up by hands and sometimes deposited to nose
A study was conducted in a 12-bed UK adult general ICU to measure the contact rate by healthcare workers with patients (direct contacts), and with patient’s immediate environment
6
(indirect contact) [38]. This study reported that on average each patient was contacted directly
159 (95% confidence intervals (CI) 144-178) and indirectly 191 (95% CI 174 – 121) times/day.
Of note, there were more indirect contacts compared to direct contacts. In our model, nurse visits each patient’s room for 20 minutes per hour. During this time the nurse touches the patient with the same rate that nurse touches the porous and nonporous surfaces i.e. 8 times per hour. While this rate represents contact rates reported in the above study, contact rates in different institutions or different clinical settings may vary.
The rate at which a fingertip touches the nasal and conjunctival mucosa was examined in a study of rhinovirus transmission, where medical and non-medical personnel seated in a
conference room were observed [39]. The average reported rate was on average 0.33 times per
person-hour of observation (i.e. 0.005 times per minute). Another study that examined the frequency with which adults touched their nostrils reported a frequency range of 1 to 30 times
within a continuous 3 h of observation (i.e. 0.0055 to 0.167 times per minute [40]. In this model,
we chose the rate of 0.025 times per minute, the mid-range of these studies.
S4. S. aureus transferred between contacting surfaces.
There are three types of contacts i.e. direct contact of hand and skin, indirect contact of hand and surface, and contact of fingertip and nose. Following each contact, pathogen can be transferred between the two contacting surfaces. Several factors can influence the transfer between surfaces: the nature of the environmental surfaces, moisture, temperature, relative humidity in the air, pressure applied during contact, amount of bacteria on both contact surfaces,
as well as the bacterial species [41, 42].
7
S4.1 Transfer efficiency
Transfer efficiency is a measure of the fraction of the organisms on one surface that is transferred to another contacting surface. In general, surfaces are referred to as one of the following categories: porous and nonporous or textile and non-textile. We used the former category in this study. Despite a wide range of gross characteristics, porous surface was referred to as surface with pores or deep recesses where organisms may reside. Conversely, nonporous surface was frequently hard and smooth surface that does not offer crevices in which microorganism may hide.
S4.2 Transfer from hands to surfaces and from surfaces to hands
A study in 1990 investigated the survival and transfer of 5 different organisms including
S. aureus
[32]. The laminate surfaces were contaminated, and the amount transferred to hands
was measured at 0, 1, 2, and 24 h post contamination. Organisms were transferred more efficiently from laminate surfaces than from clothes. The transfer efficiency from laminate surfaces to hands was the highest at one hour after contamination (43%) and decreased subsequently. Similarly, the transfer efficiency from contaminated clothes to hands was also the highest at one hour after contamination (5%). At 24 h, however, there appeared to be regrowth of
S. aureus . This led to higher measures in transfer efficiency that was concluded to be spurious.
The transfer efficiency of S. aureus from fabrics (100% cotton and 50-50% cottonpolyester) to finger pads of adult volunteers were tested using moist, dry, and re-moistened
pieces of fabrics, with or without friction during contact [41]. Higher levels of transfer occurred
between moist donors and/or recipients surfaces, when friction was applied. Transfer efficiency was reported within a range of <0.1 to 2.5 % cfu depending on the environmental condition.
Another study examined the transfer efficiency of microorganisms from surfaces to hands and
8
from fingertips to lower lip using a different protocol than previously described [42]. The study
found a significant difference in transfer efficiency between porous and nonporous surfaces. The transfer efficiency for nonporous surfaces ranged from 28 to 66%, while for porous surfaces, the transfer efficiency was mostly <1%.
All these studies, although involved different experimental designs and measurement methods, agreed that nonporous surface has higher transfer efficiency than porous surfaces.
Because of the concern that environmental exposure of pathogens is a human risk, transfer efficiency has generally been measured from surfaces to human and not from human to surfaces.
In reality, however, it is likely that each contact results in bidirectional pathogen flows between the contacting surfaces. In this model, we assumed symmetrical transfer efficiency. We chose conservative transfer efficiency values of 0.4 for the nonporous surface, and 0.1 for the porous surface.
S4.3 Transfer from fingertip to nose and from nose to fingertip
To the best of our knowledge, there have been no studies on transfer efficiency from hand to nose. However, bacterial transfer efficiency from fingertip to lower lip was measured to be
within a range of 34 to 41% [42]. In our model, we assume that the transfer efficiency from hand
to nose is much less than the transfer efficiency from fingertip to lip, given there is less direct contact of the fingertip to the anterior nares, where S. aureus resides. We used 0.2 as transfer efficiency for fingertip to nose.
S4.4 Transfer from hand to hand
There are no studies on the transfer efficiency from hand to hand. We assumed the
efficiency from hand to hand to be similar to that from fingertip to lip [42].
9
Reference
1. Verbrugh HA: Colonization with Staphylococcus aureus and the role of colonization in causing infection. In Staphylocci in human disease.
2 nd
edition. Edited by Crossley KB,
Jefferson KK, Archer GL, Fowler Jr VG. Wiley-Blackwell; 2009:255-71.
2. Cimolai N: MRSA and the environment: implications for comprehensive control
measures. Eur J Clin Microbiol Infect Dis 2008, 27 :481-493.
3. Dancer SJ: Importance of the environment in meticillin-resistant Staphylococcus aureus acquisition: the case for hospital cleaning.
Lancet Infect Dis 2008, 8 :101-113.
4. Hare R, Thomas CGA: The transmission of Staphylococcus aureus. Br Med J 1956:840-
844.
5. Hare R, Ridley M: Further studies on the transmission of Staph. aureus.
Br Med J
1958:69-73.
6. Davies RR, Noble WC: Dispersal of bacteria on desquamated skin.
Lancet 1962, 2 :1295-
1297.
7. Davies RR, Noble WC: Dispersal of staphylococci on desquamated skin.
Lancet 1963,
1 :1111.
8. Noble WC, Davies RR: Studies on the dispersal of staphylococci . J Clin Pathol 1965,
18 :16-19.
9. Mackintosh CA, Lidwell OM, Towers AG, Marples RR: The dimensions of skin fragments
dispersed into the air during activity. J Hyg 1978, 81 :471-479.
10. Lidwell OM, Noble WC, Dolphin GW: The use of radiation to estimate the numbers of micro-organisms in airborne particles . J Hyg 1959, 57 :299-308.
11. Boe J, Solberg CO, Vogelsang TM, Wormnes A: Perineal carriers of staphylococci. Br
Med J 1964, 2 :280-281.
12. Solberg C: A study of carriers of Staphylococcus aureus with special regard to quantitative bacterial estimations.
Acta Med Scand 1965, 436 :1-96.
13. Williams RE: Epidemiology of airborne staphylococcal infection.
Bacteriol Rev 1966,
30 :660-674.
14. Meers PD, Yeo GA: Shedding of bacteria and skin squames after handwashing.
J Hyg
1978, 81 :99-105.
15. Plano LR, Garza AC, Shibata T, et al. : Shedding of Staphylococcus aureus and methicillin-resistant Staphylococcus aureus from adult and pediatric bathers in marine
waters. BMC microbiology 2011, 11 :5.
10
16. Gehanno JF, Louvel A, Nouvellon M, Caillard JF, Pestel-Caron M: Aerial dispersal of meticillin-resistant Staphylococcus aureus in hospital rooms by infected or colonised patients.
J Hosp Infect 2009, 71 :256-262.
17. Solberg CO: Spread of Staphylococcus aureus in hospitals: causes and prevention.
Scand
J Infect Dis 2000, 32 :587-595.
18. Noble WC, Lidwell OM, Kingston D: The size distribution of airborne particles carrying
micro-organisms. J Hyg 1963, 61 :385-391.
19. Williams RE: Airborne staphylococci in the surgical ward.
J Hyg 1967, 65 :207-217.
20. Noble WC: The dispersal of staphylococci in hospital wards. J Clin Pathol 1962, 15 :552-
558.
21. Hill J, Howell A, Blowers R: Effect of clothing on dispersal of Staphylococcus aureus by
males and females. Lancet 1974, 2 :1131-1133.
22. Clements MO, Foster SJ: Stress resistance in Staphylococcus aureus.
Trends Microbiol
1999, 7 :458-462.
23. Farrington M, Brenwald N, Haines D, Walpole E: Resistance to desiccation and skin fatty acids in outbreak strains of methicillin-resistant Staphylococcus aureus.
J Med Microbiol
1992, 36 :56-60.
24. Wagenvoort JH, Sluijsmans W, Penders RJ: Better environmental survival of outbreak vs. sporadic MRSA isolates.
J Hosp Infect 2000, 45 :231-234.
25. Layton MC, Perez M, Heald P, Patterson JE: An outbreak of mupirocin-resistant
Staphylococcus aureus on a dermatology ward associated with an environmental reservoir.
Infect Control Hosp Epidemiol 1993, 14 :369-375.
26. Rampling A, Wiseman S, Davis L, et al : Evidence that hospital hygiene is important in the control of methicillin-resistant Staphylococcus aureus . J Hosp Infect 2001, 49 :109-116.
27. Rountree PM: The effect of desiccation on the viability of Staphylococcus aureus.
J Hyg
1963, 61 :265-272.
28. Beard-Pegler MA, Stubbs E, Vickery AM: Observations on the resistance to drying of
staphylococcal strains. J Med Microbiol 1988, 26 :251-255.
29. Masago Y, Shibata T, Rose JB: Bacteriophage P22 and Staphylococcus aureus
attenuation on nonporous fomites as determined by plate assay and quantitative PCR. Appl
Environ Microbiol 2008, 74 :5838-5840.
30. McDade JJ, Hall LB: Survival of Staphylococcus aureus in the environment. I. Exposure
of surfaces. American Journal of Hygiene 1963, 78 :330-337.
11
31. Gontijo Filho PP, Stumpf M, Cardoso CL: Survival of gram-negative and gram-positive
bacteria artificially applied on the hands. J Clin Microbiol 1985, 21 :652-653.
32. Scott E, Bloomfield SF: The survival and transfer of microbial contamination via cloths,
hands and utensils. The Journal of Applied Bacteriology 1990, 68 :271-278.
33. Neely AN, Maley MP: Survival of enterococci and staphylococci on hospital fabrics and
plastic. J Clin Microbiol 2000, 38 :724-726.
34. Cuesta A, Nastri N, Bernat M, Brusca M, Turcot L, Nastri M, Rosa AC: Survival of
Staphylococcus aureus on fomites.
Acta Odontol Latinoam 2008, 21 :141-146.
35. Traore O, Springthorpe VS, Sattar SA: A quantitative study of the survival of two species
of Candida on porous and non-porous environmental surfaces and hands. J Appl Microbiol
2002, 92 :549-555.
36. Noskin GA, Stosor V, Cooper I, Peterson LR: Recovery of vancomycin-resistant enterococci on fingertips and environmental surfaces.
Infect Control Hosp Epidemiol 1995,
16 :577-581.
37. Hart CA, Gibson MF, Buckles AM: Variation in skin and environmental survival of hospital gentamicin-resistant enterobacteria.
J Hyg 1981, 87 :277-285.
38. McArdle FI, Lee RJ, Gibb AP, Walsh TS: How much time is needed for hand hygiene in intensive care? A prospective trained observer study of rates of contact between healthcare
workers and intensive care patients. J Hosp Infect 2006, 62 :304-310.
39. Hendley JO, Wenzel RP, Gwaltney JM, Jr : Transmission of rhinovirus colds by selfinoculation.
N Engl J Med 1973, 288 :1361-1364.
40. Nicas M, Best D: A study quantifying the hand-to-face contact rate and its potential
application to predicting respiratory tract infection. J Occup Environ Hyg 2008, 5 :347-352.
41. Sattar SA, Springthorpe S, Mani S, Gallant M, Nair RC, Scott E, Kain J: Transfer of bacteria from fabrics to hands and other fabrics: development and application of a
quantitative method using Staphylococcus aureus as a model. J Appl Microbiol 2001,
90 :962-970.
42. Rusin P, Maxwell S, Gerba C: Comparative surface-to-hand and fingertip-to-mouth transfer efficiency of gram-positive bacteria, gram-negative bacteria, and phage.
J Appl
Microbiol 2002, 93 :585-592.
12
Supplemental Material II
Table S2. Submodel for a direct contact event between nurses’ hands (NS) and the uncolonized patient (PTu). NS represents the concentration of MRSA cfu on nurses’ hands (MRSA cfu/2000 sq.cm.). PTu represents the concentration of MRSA cfu on the uncolonized patient (MRSA cfu/2000 sq.cm.). The transfer efficiency of MRSA from nurses’ hands to the uncolonized patient’s skin was assumed to be the same as transfer efficiency from the uncolonized patient’s skin to nurses’ hands.
Total surface area
(sq.cm.)
Contact surface area
(sq.cm.)
Transfer efficiency ( sk
)
Nurses (NS)
2000
150
0.35
Uncolonized patient (PTu)
2000
150
0.35
Bidirectional flows between the two contacting surfaces:
13
Differential equations
The diagram of the compartmental model is shown in Figure 1 in the main text. The definitions of the parameters are presented in Table 1, also in the main text. The following are differential equations for the ten compartments.
1) The colonized patient (PT c
)
We assumed that the colonized patient maintains a steady MRSA concentration on the exposed skin and hands (PT c
). This balance was achieved by the gain and loss in MRSA. The colonized patient gained MRSA from the replenishment of the contaminated skin scales and from touching the nose. The replenishing rate was assumed to be the same as the dispersal rate.
Concentration of MRSA in the nose (PT cn
) was assumed constant (1000 cfu/4 cm 2 ). The colonized patient, on the other hand, lost MRSA from natural die-off and from pathogen flows to surfaces and nurses due to touching events. The nurses touched the colonized patient only during the first 20 minutes of the hour.
The change in MRSA on the skin and hand of the colonized patient (PT c
) are given by: 𝑑𝑃𝑇 𝑑𝑡 𝑐
= 𝛼𝐴
−𝑃𝑇 𝑐 𝑝𝑡
− 𝑃𝑇 𝑐
𝐴 𝑓
𝐴 𝑝𝑡
𝐴 𝑐
𝐴 𝑝𝑡 𝜌 𝑛𝑝 𝜏 𝑝𝑡−𝑛𝑝 𝜌 𝑛 𝜏 𝑛
+ 𝑁𝑃 𝑐
−𝑃𝑇 𝑐 𝜇 𝑠𝑘
+ 𝑃𝑇 𝑐𝑛
𝐴
𝐴 𝑐 𝑛𝑝 𝜌 𝑝
𝐴
𝐴 𝑓 𝑛 𝜌 𝑛 𝜏 𝑝𝑡−𝑛𝑝 𝜏 𝑛
− 𝑃𝑇
− 𝑃𝑇 𝑐 𝑐
𝐴 𝑐
𝐴
𝐴 𝑝𝑡 𝑝𝑡
𝐴 𝑐 𝜌 𝜌 𝑠𝑘 𝜏 𝑝 𝜏 𝑝𝑡−𝑝 𝑛𝑠−𝑝𝑡
+ 𝑃 𝑐
𝐴
𝐴 𝑐 𝑝 𝜌 𝑓(𝑡) + 𝑁𝑆 𝑝 𝜏 𝑝𝑡−𝑝
𝐴 𝑐
𝐴 𝑛𝑠 𝜌 𝑠𝑘 𝜏 𝑛𝑠−𝑝𝑡 𝑓(𝑡)
(1) where, m
+, and 𝑓(𝑡) = {
1, 𝑡 ∈ [𝑚 − 1, 𝑚 −
0, 𝑡 ∈ [𝑚 −
2
, 𝑚)
3
2
3
)
(2)
14
The function f ( t ) is a time indicator function for a nurse’s visit in the colonized patient’s room. f ( t ) was equal to one during the first 20 minutes, allowing nurse touching events to occur and equal to 0 during other times.
PT c
was initialized at the equilibrium MRSA level of 6,000 cfu/2000 cm 2 .
2) The porous surface in the colonized patient’s room (P c
)
Changes in MRSA on the porous surface in the colonized patient’s room (P c
), as described in Equation 3, were driven by the deposition of MRSA on the surface, surface touches by the colonized patient, surfaces touches by the nurses during the first 20 minutes of the hour, natural die-off, and daily surface decontamination. 𝑑𝑃 𝑐
= 𝛼𝐴 𝑑𝑡
+𝑁𝑆
𝐴 𝑐
𝐴 𝑛𝑠 𝑝
− 𝑃 𝑐
𝐴
𝐴 𝑐 𝑝 𝜌 𝑝 𝜏 𝑝𝑡−𝑝
+ 𝑃𝑇 𝑐
𝐴
𝐴 𝑐 𝑝𝑡 𝜌 𝜌 𝑝 𝜏 𝑛𝑠−𝑝 𝑓(𝑡) − 𝑃 𝑐 𝜖 𝑑 ℎ(𝑡) − 𝑃 𝑐 𝜇 𝑝 𝑝 𝜏 𝑝𝑡−𝑝
− 𝑃 𝑐
𝐴 𝑐
𝐴 𝑝 𝜌 𝑝 𝜏 𝑛𝑠−𝑝 𝑓(𝑡)
(3) where, m
+, and ℎ(𝑡) = {
1, 𝑡 = 𝑚 ∗ 24
0, 𝑜𝑡ℎ𝑒𝑟𝑤𝑖𝑠𝑒
(4)
The function h ( t ) is a time indicator function that regulates decontamination to every 24 hours.
3) The nonporous surface in the colonized patient’s room (NP c
)
Changes of MRSA on the nonporous surface in the colonized patient’s room (NP c
), as described in Equation 5, were driven by the deposition of MRSA dispersal on the surface, surface touches by the colonized patient, surface touches by the nurses during the first 20
15
minutes of the hour, the natural die-off, and the daily surface decontamination. Structurally, the nonporous surface is similar to the porous surface, except that only the nonporous surfaces can be wiped off following a nurse touch. The wiping rate is as frequent as the rate that nurses touch the nonporous surface. The efficacy of the wipes and the wiping rate is denoted by w
and ns-np
, respectively. 𝑑𝑁𝑃 𝑐
= 𝛼𝐴 𝑑𝑡
+𝑁𝑆
𝐴 𝑐
𝐴 𝑛𝑠 𝜌 𝑛𝑝 𝑛𝑝
− 𝑁𝑃 𝜏 𝑛𝑠−𝑛𝑝 𝑐
𝐴
𝐴 𝑐 𝑛𝑝 𝜌 𝑛𝑝 𝜏 𝑓(𝑡) − 𝑁𝑃 𝑐 𝑝𝑡−𝑛𝑝
𝐴
𝐴 𝑐 𝑛𝑝
+ 𝑃𝑇 𝑐
𝐴
𝐴 𝑐 𝑝𝑡 𝜌 𝑛𝑝 𝜏 𝑝𝑡−𝑛𝑝
− 𝑁𝑃 𝑐
𝐴
𝐴 𝑐 𝑛𝑝 𝜌 𝑛𝑝 𝜏 𝑛𝑠−𝑛𝑝 𝜖 𝑤 𝜔 𝑛𝑠−𝑛𝑝 𝑓(𝑡) − 𝑁𝑃 𝑐 𝜖 𝑑 ℎ(𝑡) − 𝑁𝑃 𝑐 𝜇 𝑛𝑝 𝑓(𝑡)
(5)
4) The uncolonized patient (PT u
)
Changes of MRSA on the skin and hands of the uncolonized patient (PT u
),as described in
Equation 6, were driven by contacts with nurses during the second 20 minutes of the hour, contacts with the two room surfaces, contact with one’s own nose, and the natural die-off on the skin and hand. 𝑑𝑃𝑇 𝑑𝑡 𝑢
−𝑃𝑇 𝑢
= −𝑃𝑇
𝐴 𝑐
𝐴 𝑝𝑡 𝑢
𝐴
𝐴 𝑓 𝑝𝑡 𝜌 𝑛𝑝 𝜏 𝑝𝑡−𝑛𝑝 𝜌 𝑛 𝜏 𝑛
+ 𝑃𝑇
+ 𝑁𝑃 𝑢
𝐴 𝑐 𝑢𝑛
𝐴 𝑛𝑝
𝐴
𝐴 𝜌 𝑝 𝑓 𝑛 𝜌 𝑛 𝜏 𝜏 𝑝𝑡−𝑛𝑝 𝑛
− 𝑃𝑇
− 𝑃𝑇 𝑢 𝑢
𝐴 𝑐
𝐴
𝐴
𝐴 𝑝𝑡 𝑐 𝑝𝑡 𝜌 𝜌 𝑠𝑘 𝑝 𝜏 𝑝𝑡−𝑝 𝜏 𝑛𝑠−𝑝𝑡
+ 𝑃 𝑢
𝐴
𝐴 𝑐 𝑝 𝜌 𝑔(𝑡) + 𝑁𝑆 𝑝 𝜏
𝐴 𝑐 𝑝𝑡−𝑝
𝐴 𝑛𝑠 𝜌 𝑠𝑘 𝜏 𝑛𝑠−𝑝𝑡 𝑔(𝑡)
−𝑃𝑇 𝑢 𝜇 𝑠𝑘 where, m
+, and
(6) 𝑔(𝑡) = {
1,
0, 𝑡 ∈ [𝑚 −
2
3
, 𝑚 − 𝑡 ∈ [𝑚 − 1, 𝑚 −
1
3
)
2
3
) 𝑜𝑟[𝑚 −
1
3
, 𝑚]
(7)
16
The function g ( t ) is a time indicator function regulating the nurse’s visit in the uncolonized patient’s room. g ( t ) was equal to one during the second 20 minutes of the hour, allowing the nurse’s touching events to occur and equals 0 during other times.
5) The porous surface in the uncolonized patient’s room (P u
)
Changes of the porous surface in the uncolonized patient’s room, as described in
Equation 8 were similar to those of the porous surface in the colonized patient’s room except that there was no MRSA dispersal and deposition in the uncolonized patient’s room. Surface touches by the nurse occurred during the second 20 minutes of the hour. 𝑑𝑃 𝑢
= −𝑃 𝑑𝑡
+𝑁𝑆
𝐴 𝑐
𝐴 𝑛𝑠 𝑢
𝐴
𝐴 𝑐 𝑝 𝜌 𝑝 𝜏 𝑝𝑡−𝑝
+ 𝑃𝑇 𝑢
𝐴
𝐴 𝑐 𝑝𝑡 𝜌 𝑝 𝜏 𝑝𝑡−𝑝 𝜌 𝑝 𝜏 𝑛𝑠−𝑝 𝑔(𝑡) − 𝑃 𝑢 𝜖 𝑑 ℎ(𝑡) − 𝑃 𝑢 𝜇 𝑝
− 𝑃 𝑢
𝐴 𝑐
𝐴 𝑝 𝜌 𝑝 𝜏 𝑛𝑠−𝑝 𝑔(𝑡)
(8)
6) The nonporous surface in the uncolonized patient’s room (NP u
)
Changes of the nonporous surface in the uncolonized patient’s room, as described in
Equation 9, were similar to those of the nonporous surface in the colonized patient’s room except that there was no MRSA dispersal and deposition in the uncolonized patient’s room. Surface touches by the nurse occurred during the second 20 minutes of the hour. 𝑑𝑁𝑃 𝑢
= −𝑁𝑃 𝑑𝑡
+𝑁𝑆
𝐴 𝑐
𝐴 𝑛𝑠 𝜌 𝑛𝑝 𝑢
𝐴
𝐴 𝑐 𝑛𝑝 𝜌 𝑛𝑝 𝜏 𝑝𝑡−𝑛𝑝
+ 𝑃𝑇 𝜏 𝑛𝑠−𝑛𝑝 𝑔(𝑡) − 𝑁𝑃 𝑢
𝐴
𝐴 𝑐 𝑢 𝑛𝑝
𝐴 𝑐
𝐴 𝑝𝑡 𝜌 𝑝 𝜏 𝑝𝑡−𝑛𝑝 𝜖 𝑤
− 𝑁𝑃 𝑢
𝐴
𝐴 𝑐 𝑛𝑝 𝜔 𝑛𝑠−𝑛𝑝 𝑔(𝑡) − 𝑁𝑃 𝑢 𝜖 𝑑 𝜌 𝑛𝑝 𝜏 𝑛𝑠−𝑛𝑝 𝑔(𝑡) ℎ(𝑡) − 𝑁𝑃 𝑢 𝜇 𝑛𝑝
(9)
7) The nurses (NS)
Changes of MRSA on the exposed skin and hands of nurses (NS), as described in
Equation 10, were driven by all nurse activities and natural die-off on skin and hands. Activities
17
of nurse included touching the colonized patient and the room surfaces during the first 20 minutes while in the colonized patient’s room, and touching the uncolonized patient and the room surfaces during the second 20 minutes while in the uncolonized patient’s room, and touching one’s own noses. Nurses may also wipe the nonporous surfaces after a nonporous surface touch. Nurses were assumed to have clean skin and hands at the beginning of each 8hour shift. The time indicator for the beginning of the shift is s(t) . 𝑑𝑁𝑆 𝑑𝑡
= −𝑁𝑆
𝐴 𝑐
−𝑁𝑆
−𝑁𝑆
𝐴 𝑛𝑠
𝐴 𝑐
𝐴 𝑛𝑠
−𝑁𝑆
𝐴
𝐴 𝑐 𝑛𝑠
𝐴 𝑓 𝑛𝑠 𝜌 𝜌 𝑝 𝜏 𝑛𝑠−𝑝 𝜌 𝑠𝑘 𝜌 𝑛𝑝
𝐴 𝜏 𝑛 𝜏 𝑛𝑠−𝑝𝑡 𝑔(𝑡) + 𝑃𝑇 𝑢 𝑛𝑠−𝑛𝑝 𝜏 𝑛
+ 𝑁𝑆 𝑓(𝑡) + 𝑃 𝑐 𝑛
𝐴
𝐴 𝑐
𝐴 𝑝 𝑔(𝑡) + 𝑁𝑃
𝐴 𝑓 𝑢 𝑛 𝜌 𝑛 𝜏 𝑛
− 𝑁𝑆 𝜌 𝑝 𝜏 𝑛𝑠−𝑝
𝐴 𝑐
𝐴 𝑝𝑡
𝐴 𝑐
𝐴 𝑛𝑝 𝜌 𝑠𝑘 𝜌 𝑛𝑝 𝑓(𝑡) − 𝑁𝑆 𝜏
𝐴 𝑛𝑠−𝑝𝑡
𝐴 𝜏 𝑛𝑠−𝑛𝑝 𝑐 𝑛𝑠 𝜌 𝑠𝑘
𝐴
𝐴 𝜏 𝑐 𝑛𝑠 𝑛𝑠−𝑝𝑡 𝜌 𝑔(𝑡) − 𝑁𝑆 𝑛𝑝
𝐴
𝐴 𝜏 𝑐 𝑓(𝑡) + 𝑃𝑇 𝑛𝑠−𝑛𝑝 𝑛𝑠 𝜌 𝑝 𝜏 𝑓(𝑡) + 𝑁𝑃 𝑛𝑠−𝑝 𝑐
𝐴 𝑛𝑝 𝑔(𝑡) + 𝑃 𝑔(𝑡) – 𝑁𝑆𝑠(𝑡) − 𝑁𝑆𝜇 𝑠𝑘
𝐴
𝐴 𝑐 𝑝𝑡 𝑐 𝜌 𝑠𝑘
𝐴 𝑐 𝑢 𝜏 𝑛𝑠−𝑝𝑡
𝐴 𝜌
𝐴 𝑐 𝑝 𝑛𝑝 𝜌 𝑝 𝜏 𝑛𝑠−𝑛𝑝 𝜏 𝑓(𝑡) 𝑛𝑠−𝑝
(10) 𝑓(𝑡) 𝑔(𝑡) where, m
+ and 𝑠(𝑡) = {
1,
0, 𝑡 = 𝑚 ∗ 8 𝑜𝑡ℎ𝑒𝑟𝑤𝑖𝑠𝑒
(11)
The other two compartments in the model are MRSA accumulated in the uncolonized patient’s nose and nurse’s nose. They are given by: 𝑑𝑃𝑇 𝑢𝑛 𝑑𝑡 𝑑𝑁𝑆 𝑛 𝑑𝑡
= −𝑃𝑇 𝑢𝑛
𝐴 𝑛
𝐴 𝑓 𝜌 𝑛 𝜏 𝑛
= −𝑁𝑆 𝑛
𝐴 𝑓
𝐴 𝑛 𝜌 𝑛 𝜏 𝑛
+ 𝑃𝑇 𝑢
𝐴 𝑓
𝐴 𝑝𝑡 𝜌 𝑛 𝜏 𝑛
+ 𝑁𝑆
𝐴 𝑓
𝐴 𝑛𝑠 𝜌 𝑛 𝜏 𝑛
(12)
(13)
18
Supplemental material III
Sensitivity Analysis
To understand how our model parameter values affect the inferences resulting from our analysis, we examined the sensitivity of the exposure dose to nurses and the uncolonized patient with varying transfer efficiency, survivability, and nurse contact rate parameters. In all of these sensitivity analyses, direct exposure referred to exposure from the colonized patient to nurses and exposure from nurses to the uncolonized patient, and indirect exposure referred to exposure from both porous and nonporous surfaces to nurses and exposure from both surfaces to the uncolonized patient.
Transfer efficiency and pathogen survivability are the main two parameters that differentiate the type of surfaces we modeled, porous and nonporous. Since our simulations suggested that nonporous surfaces are the dominant exposure source to the uncolonized patient, we chose to examine how this dominance might be affected if the nonporous surface transfer efficiency (ρ np
) values varied anywhere between 0.05 and 0.75 (a value of 0.4 was used in the main simulation analysis). Our outcome exposure variables were not sensitive to changes in ρ np
.
Even at the lower bound, where ρ np
= 0.05, the indirect exposure to nurses in the colonized room remained the dominant source of exposure (Figure S1). Exposure to the uncolonized patient, however, was dominated by direct exposure to the nurse for lower values of ρ np
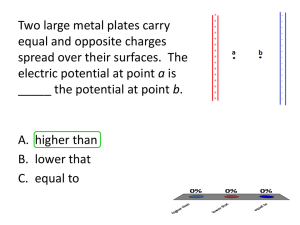
, but as ρ np approached 0.75, exposure was split evenly between direct and indirect (Figure S2). Exposure was even more sensitive to skin transfer efficiency values. The indirect exposure to the nurses
19
remained dominant regardless of the level of skin transfer efficiency, but for low values direct exposure to colonized patients became negligible (Figure S3). Likewise, for the uncolonized patient, the indirect exposure was not dominant when the skin transfer efficiency was high but became dominant for lower values (Figure S4).
Survivability describes how quickly the pathogens die off from surfaces or hands. We examined the sensitivity due to both die-off rates by (1) assigning a range of the nonporous surface die-off rate (μ np
) between 1.6 x 10 -5 and 1.6 x 10 -3 min -1 , where μ np, was assigned 2 x 10 -
4 in the main simulation; and (2) assigning a range of the skin die off rate (μ sk
) between 1x10 -4 and 1x10 -2 min -1 , where μ sk
was assigned 3.53 x 10 -3 in the main simulation. The exposure to the nurse was not very sensitive to the range of nonporous die-off rate used (Figure S5), and the exposure to the uncolonized patients was only somewhat more sensitive (Figure S6). Exposure to either the nurse or uncolonized patients was more sensitive to the skin die-off rates explored, though none of the values resulted in changes in our qualitative conclusions (Figures S7 and S8).
Interestingly, for very low skin die-off rates, the exposure to uncolonized patients began to decrease because their contamination levels were high compared to the contamination levels of the surfaces.
To examine how a human behavioral factor may affect exposure, we examined a range of nurse’s surface and patient contact from 3 to 19 times per hour. In the main simulation, nurses touched each patient and each surface 8 times per hour. Again, although we observed some variation in exposure levels, the dominant exposure sources (indirect versus direct) remain the same (Figure S9 and S10).
To further explore the variable nature of contact rates, we compared a highly touched nonporous surface (2.5 times higher than baseline) with a minimally touched nonporous surface
20
(0.5 times baseline) in terms of its impact on exposures with and without an intervention (Figure
S11 and S12). The highly touched surface was a much larger source of exposure compared to the minimally touched surface. Surface wiping appeared to be superior to daily decontamination in decreasing the exposure dose, primarily due to its increased frequency. Again, since our model structure did not allow for the exploration of spatial heterogeneity, the spatially specific nature of surface wiping was a feature that would provide additional benefits.
Finally, we performed a multivariate sensitivity analysis to examine the potential joint effects of nonporous surface transfer efficiency, skin die off rate and nurse’s contact rate. By comparing all combinations of a high and low value, the results summarized in Table S3 suggest that each parameter roughly contributed an independent effect to exposure. As the number of variables with high values increased the exposure increased. Skin survivability seemed to have the weakest effect and non-porous transfer efficiency the strongest effect on exposure.
21
Figure S1. The proportion of the nurse’s indirect exposure in the colonized patient’s room as a function of the nonporous surface transfer efficiency. Indirect exposure is the sum exposure from the porous and nonporous surfaces to the nurses. Percentage of indirect exposure to the nurses is shown above each bar. Simulation analysis in the main manuscript used 0.4 as the nonporous surface transfer efficiency, resulting in 70% indirect exposure to the nurses in the colonized patient’s room.
Figure S2. The proportion of the uncolonized patient’s indirect exposure as a function of the nonporous surface transfer efficiency. Indirect exposure is the sum exposure from the porous
22
and nonporous surfaces to the uncolonized patient. Percentages of indirect exposure to the uncolonized patient are shown above each bar. Simulation analysis in the main manuscript used
0.4 as the nonporous surface transfer efficiency, resulting in 35% indirect exposure to the uncolonized patient.
Figure S3. The proportion of the nurse’s indirect exposure in the colonized patient’s room as a function of the skin transfer efficiency. Indirect exposure is the sum exposure from the porous and nonporous surfaces to the nurse. Percentage of indirect exposure to the nurses is shown
23
above each bar. Simulation analysis in the main manuscript used 3.53 x10 -3 as the skin transfer efficiency, resulting in 70% indirect exposure to the nurses in the colonized patient’s room.
Exposure from the colonized pa ent Exposure from surfaces
2500
60%
67%
64%
61%
2000
70%
82%
75%
93%
1500
1000
500
0
0.05
0.15
0.25
0.35
0.45
Skin transfer efficiency
0.55
0.65
0.75
Figure S4. The proportion of the uncolonized patient’s indirect exposure as a function of the skin transfer efficiency. Indirect exposure is the sum exposure from the porous and nonporous surfaces to the uncolonized patient. Percentages of indirect exposure to the uncolonized patient
24
are shown above each bar. Simulation analysis in the main manuscript used 3.53 x10 -3 as the skin transfer efficiency, resulting in 35% indirect exposure to the uncolonized patient.
Figure S5. The proportion of the nurse’s exposure in the colonized patient’s room that is indirect as a function of the nonporous surface die-off rate. Indirect exposure is the sum exposure from the porous and nonporous surfaces to the nurse. Percentage of indirect exposure to the nurses is shown above each bar. Simulation analysis in the main manuscript used 2 x 10 -4 min -1 as the
25
nonporous surface die-off rate, resulting in 70% indirect exposure to the nurses in the colonized patient’s room.
Figure S6. The proportion of the uncolonized patient’s indirect exposure as a function of the nonporous surface die-off rate. Indirect exposure is the sum exposure from the porous and nonporous surfaces to the uncolonized patient. Percentages of indirect exposure to the uncolonized patient are shown above each bar. Simulation analysis in the main manuscript used
26
2 x 10 -4 min -1 as the nonporous surface die-off rate, resulting in 35% indirect exposure to the uncolonized patient.
Figure S7. The proportion of the nurse’s indirect exposure in the colonized patient’s room as a function of the skin die-off rate. Indirect exposure is the sum exposure from the porous and nonporous surfaces to the nurse. Percentage of indirect exposure to the nurses is shown above each bar. Simulation analysis in the main manuscript used 35.3 x 10 -4 min -1 as the skin die-off rate, resulting in 70% indirect exposure to the nurses in the colonized patient’s room.
27
Figure S8. The proportion of the nurse’s indirect exposure as a function of the skin die-off rate.
Indirect exposure is the sum exposure from the porous and nonporous surfaces to the uncolonized patient. Percentages of indirect exposure to the nurse are shown above each bar.
Simulation analysis in the main manuscript used 35.3 x 10 -4 min -1 as the skin die-off rate, resulting in 35% indirect exposure to the nurse.
28
Figure S9. The proportion of the nurse’s indirect exposure as a function of the nurses contact rate. The nurse contact rate of surfaces and patients are assumed to be equal. Indirect exposure is the sum exposure from the porous and nonporous surfaces to the nurse. Percentages of indirect exposure to the uncolonized patient are shown above each bar. Simulation analysis in the main manuscript used 8 as the number of times the nurse touches each surface and patient per visit, resulting in 70% indirect exposure to the uncolonized patient.
29
Figure S10. The proportion of the uncolonized patient’s indirect exposure as a function of the nurses contact rate. The nurse contact rate of surfaces and patients are assumed to be equal.
Indirect exposure is the sum exposure from the porous and nonporous surfaces to the uncolonized patient. Percentages of indirect exposure to the uncolonized patient are shown above each bar. Simulation analysis in the main manuscript used 8 as the number of times the nurse
30
touches each surface and patient per visit, resulting in 35% indirect exposure to the uncolonized patient.
Figure S11. Effects of daily decontamination and surface wiping in decreasing exposure to nurses. Three types of exposure are shown here: 1) exposure from the colonized patient, 2) exposure from minimally touched nonporous surface, and 3) exposure from highly touched nonporous surface. The numbers on top of each bar are the percent reduction following the intervention compared to when there is no intervention.
31
Figure S12.
Effects of daily decontamination and surface wiping in decreasing exposure to the uncolonized patient. Three types of exposure are shown here; 1) exposure from nurses, 2) exposure from minimally touched nonporous surface, and 3) exposure from highly touched nonporous surface. The numbers on top of each bar are the percent reduction following the intervention compared to when there is no intervention.
32
33
Table S3. Multivariate sensitivity analysis of nonporous surface transfer efficiency, skin survivability and nurse’s contact rate to surfaces and patients. These three parameters take on high or low values. The nonporous transfer efficiency (ρ np
) is either 0.1 (low) or
0.6 (high). The skin die off rate (µ sk
) is either 1 x 10 -4 min -1 (low) or 1 x 10 -2 min -1 (high). The nurse’s contact rate (τ ns-pt
, τ ns-sf
) is either
2 times per visit (low) or 20 times per visit (high). The outcomes are indirect exposure levels to the nurse, percentage of indirect exposure to the nurse, indirect exposure levels to the uncolonized patient, and percentage of indirect exposure to the uncolonized patient. The color scales rank exposure levels (orange = highest exposure, yellow = lowest exposure).
Nonporous transfer efficiency
Skin survivability
Nurse's contact rate
Indirect exposure to nurse
% Indirect exposure to nurse
Indirect exposure to uncolonized patient
% Indirect exposure to uncolonized patient low low low
37
0
0 low low high
49
0.58
0 low low high high low
70
8.19
20 high
81
54.38
12 high low low
629.33 1254.57 417.39 1609.3 1371.7 1541.44 649.4 1819.26
65
80.62
35.4 high low high
61
50.78
15.47 high high low
79
55.12
59 high high high
85
198.1
37
34