NURS 640 Primary health care for children
advertisement

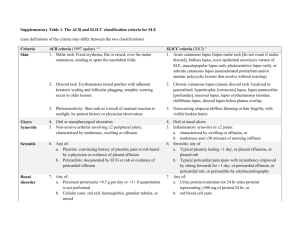
Running Head: SYSTEM LUPUS ERYTHEMTOSUS IN CHILDREN System Lupus Erythematosus in children Shanakay Haughton Coppin State University NUR 640 Dr. Raley and Dr. Dorsey November 21st 2013 1 SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN 2 Problem Systemic Lupus Erythematosus is an autoimmune disease caused by the production of auto-antibodies that affects the cell nucleus (Sato et al., 2012). It is also an inflammatory disease. Lupus can affect multiple organs or system in the body (Ferri, 2012). Lupus is a chronic disease that has periods of remission and flare up (Hay, Levin, Deterding, Abzug, & Sondheimer, 2012). It also has signs and symptoms similar to other disease processes, which can cause a delay in diagnosis (Manson & Rahman, 2009). Epidemiology The incidence of Lupus is 20 to 70 per 100,000 persons (Ferri, 2012). Systemic Lupus Erythematosus is common in girls between the ages of 9 and 15 years old (Sato et al., 2012). The female to male ratio is 9:1. It is not usually seen before the age of five (Manson & Rahman, 2009). It is predominant in Non-Caucasian populations, such as African Americans, Hispanics, Indians, and Australians (Concannon, Rudge, Yan, & Reed, 2013). 10% of individuals diagnosed with Lupus have a family member with lupus (Ferri, 2012). Analysis of the topic with supporting literature Five percent of children born to women will develop the disease (CDC, 2013). It is three times more common in African American than any other ethnic group (Concannon, Rudge, Yan, & Reed, 2013). Girls are more prone to Lupus than boys, which may be linked to hormones (Manson & Rahman, 2009). Children with family history of Lupus or those with genetic tendency can trigger the disease by extreme stress SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN 3 or infection (CDC, 2013). The diagnosis of Lupus is usually made when girls reach puberty or childbearing age (Manson & Rahman, 2009). The kidney is one of the organs commonly affected by Lupus. Neutrophil gelatinase- associated lipocalin is a protein that is secreted by leukocytes during inflammation caused by Lupus (Hammad et al., 2013). This protein causes nephrotoxic and ischemic damage to the kidneys resulting in lupus nephritis (Sato et al., 2012). Lupus nephritis is a common clinical manifestation and a very important marker of morbidity and mortality in children (Concannon, Rudge, Yan, & Reed, 2013). Lupus nephritis is higher in children than adult and most children usually require dialysis and kidney transplant (Concannon, Rudge, Yan, & Reed, 2013). As children under the age of two have nonspecific symptoms such as rash and fever, it makes diagnosing Lupus difficult (Dung, Loan, Nielsen, Zak, & Peterson, 2012). Studies also show that 13% of children have central nervous symptoms such as seizure and psychosis (Concannon, Rudge, Yan, & Reed, 2013). Cardiopulmonary disease was another manifestation found in 35% of children with Lupus, and incidences were higher in African American children (Dung, Loan, Nielsen, Zak, & Peterson, 2012). African American children have 66% more malar rash and 13% more discoid Lupus than other ethnic groups (Concannon, Rudge, Yan, & Reed, 2013). Hematological signs and symptoms are common in children with Lupus, and it affects their quality of life and also their survival rate (Gokee et al., 2012). Anemia is the most common hematological disorder found in Systemic Lupus Erythematous (Sato et SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN 4 al., 2012). Coombs positive hemolytic anemia is present in 86% of children with lupus (Gokee et al., 2012). Diagnosis and Differentials diagnosis Lupus is diagnosed if four or more of the following criteria are met (Ferri, 2012). One of the criteria is Malar rash commonly called the butterfly rash. It is usually present on the cheeks of patients (Ferri, 2012). Discoid rash is another rash that may be seen in patients with lupus. It is an annular, scaly rash on the face, extremities, and scalp, which may lead to scaring (Manson & Rahman, 2009). Some patients with Lupus have photosensitivity which increases rashes in areas of increased sun exposure ("Systemic lupus erythematosus:Primer for managed care", 2012). Mucous membrane ulcers are painless and are usually found on hard palate and nasal septum of Lupus patient (Ferri, 2012). Arthritis of small and large joints are common (Ferri, 2012). Serositis includes pleuritis and pericarditis. Patients with serositits usually complain of chest pain and difficulty breathing (Arnaud, Alexis, Boddaert, & Amoura, 2012). Renal disorder is normally present with proteinuria greater than 0.5mg/dl (Daleboudt, Berger, Broadbent, & Kaptein, 2011). Neurological disorders such as seizures and psychosis are a clinical finding present in children with Lupus (Hay, Levin, Deterding, Abzug, & Sondheimer, 2012). Hemolytic disorders, such as hemolytic anemia, leucopenia, lymphopenia, and thrombocytopenia, are common in Lupus (Manson & Rahman, 2009). Positive ANA is seen in a majority of children with Lupus and also autoantobodies which are double stranded DNA antibody (Hay, Levin, Deterding, Abzug, & Sondheimer, 2012). SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN 5 Differential diagnosis for Lupus is very broad since there are many disease processes with the same signs and symptoms. The most common differential diagnosis for Lupus is rheumatological disorders, rheumatoid arthritis, neoplastic disorder, Reynaud phenomenon, systemic infection ,and thrombotic thrombocytopenic purpura (Manson & Rahman, 2009). A negative ANA test essentially excludes the diagnosis for Lupus (Hay, Levin, Deterding, Abzug, & Sondheimer, 2012). Positive antibodies or antidouble –stranded DNA and Smith antibodies are very specific and sensitive to Lupus (Hay, Levin, Deterding, Abzug, & Sondheimer, 2012). It has a sensitivity of 96% (Ferri, 2012). Management of the problem and Nurse Practitioner role If Lupus is suspected, the following should be drawn a complete blood count with differential, blood urea nitrogen, serum creatinine, urinalysis, ERS, PT, ANA, AntidsDNA, Lupus anticoagulant ,and random spot urine protein ("Systemic lupus erythematosus: Primer for managed care", 2012). Lupus is treated depending on the organ or area of the body that is affected. Immunosuppressive drugs are used as steroid sparing drugs such as Methotrexate to decrease the severity of the disease (Bernknopf, Rowley, & Bailey, 2011). Patients with joint pain and serositis symtoms are controlled by using nonsteroidal anti-inflammatory drugs, or they use low doses of corticosteroids (Ferri, 2012). Patients with arthritis from Lupus can use Hydroxychloroquine and methotrexate which has proven to be very effective (Hay, Levin, Deterding, Abzug, & Sondheimer, 2012). Patients with severe or difficult arthritis can use Leflumomide or anti-TNF agents (Bernknopf, Rowley, & Bailey, 2011). 6 SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN Patients with signs or symptoms that include the skin can use topical or intradermal corticosteroids, which have proven helpful in patients with discoid lesions (Ferri, 2012). Studies show that Hydroxychloroquine and Quinacrine are very effective in treating refractory skin disease (Bernknopf, Rowley, & Bailey, 2011). Patients with hematological manifestations are treated with corticosteroids as first line therapy (Ferri, 2012). Medication such as Azathioprine can be used for thrombocytopenia or hemolytic anemia (Arnaud, Alexis, Boddaert, & Amoura, 2012). Rituximab and intravenous immunoglobin is effective in treating sever leucopenia, autoimmune hemolytic anemia, and autoimmune thrombocytopenia (Bernknopf, Rowley, & Bailey, 2011). The central nervous system or neurological signs and symptoms associated with Lupus are treated symptomatically (Ferri, 2012). Headaches are treated with pain medication. Patients suffering from seizure and psychosis are treated with anticonvulsants and antipsychotics (Bernknopf, Rowley, & Bailey, 2011). However, treatment for other neuropsychiatic symptoms of Lupus have not yet been developed (Arnaud, Alexis, Boddaert, & Amoura, 2012). Renal disease or lupus nephritis can be treated with high doses of monthly intravenous Cyclophosphamide combined with corticosteroid (Daleboudt, Berger, Broadbent, & Kaptein, 2011). This treatment helps to preserve renal function. Mycophenolate mofetil is used for maintenance therapy in patients with renal diseases caused by Lupus (Ferri, 2012). Kidney transplant, plasmapheresis, and hemodialysis are considered for patient with serious kidney involvement. Belimumab is a drug recently approved for treating adults with positive Lupus antibody (Bernknopf, Rowley, & Bailey, 2011). It was not approved for treatment in children. SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN 7 Nurse Practitioners who are aware of new information and treatment for children with rheumatological disease such as Lupus, help to prevent morbidity and mortality ("Systemic lupus erythematosus:Primer for managed care", 2012). Nurse practitioners can manage care in patients with Lupus by educating patients about the disease process and also providing counseling for patients who are at childbearing age. Patient teaching should include the avoidance of sunlight and the use of SPF sunscreen (Hay, Levin, Deterding, Abzug, & Sondheimer, 2012). The patient should also be taught how to reduce or avoid stress if possible. The nurse practitioner should order the initial labs mentioned previously and refer patients to specialists per results. Patients should be referred to a specialist such as a rheumatologist, hematologist for patient with hematological abnormalities, and a nephrologist for those who have renal involvement and a dermatologist for patient with skin rash and cardiologist for patients with cardiac involvement (Arnaud, Alexis, Boddaert, & Amoura, 2012). The nurse practitioner will manage the care of the patient and make sure they are seeing their referred specialist. They can follow up on test results and lab work to make sure they know the progression of the disease process. SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN 8 Reference Arnaud, L., Alexis, A., Boddaert, J., & Amoura, Z. (2012). Late-Onset Systemic Lupus Erythematosus Epidemiology, Diagnosis and Treatment. Journal of Advance medicine, 29(3), 181-189. Bernknopf, A., Rowley, K., & Bailey, T. (2011). A review of systemic lupus erythematosus and current treatment option. Formulary Journal, 46. Centers for disease control and prevention (n.d.). Systemic lupus erythmatosus. Retrieved November 20, 2013 from http://www.cdc.gov/arthritis/basics/lupus.htm Concannon, A., Rudge, S., Yan, J., & Reed, P. (2013). The incidence, diagnostic clinical manifestations and severity of juvenile systemic lupus erythematosus in New Zealand Maori and Pacific Island children: The Starship experience (2000_2010). Lupus, 22(11), 1156-61. Daleboudt, G., Berger, S., Broadbent, E., & Kaptein, A. (2011). Health-related quality of life in patients with systemic lupus erythematosus and proliferative lupus nephritis. Psychology, Health & Medicine, 16(4), 393-404. Dung, N., Loan, H., Nielsen, S., Zak, M., & Peterson, F. (2012). Juvenile systemic lupus erythematosus onset patterns in Vietnamese children: a descriptive study of 45 SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN 9 children. Pediatric Rheumatology, 10(38). Ferri, F. F. (2012). Ferri's clinical advisor 2013: 5 books in 1. St. Louis, Mo: Elsevier Mosby. Gokee, M., Bilginer, Y., Besbas, N., Ozaltin, F., Cetin, M., Gumruk, F., & Ozen, S. (2012). Hematological features of pediatrics systemic lupus erythematosus:suggesting management strategies in children. Pediatric Lupus, 21, 878-884. Hammad, A., Mosaad, Y., Elhanbly, S., Youssef, H., Refaaey, A., Elhusseini, F., & Bakr, A. (2013). Urinary neutrophil gelatinase-associated lipocalin as a marker of severe lupus nephritis in children. Pediatric Lupus, 22, 486-491. Hay, W., Levin, M., Deterding, R., Abzug, M., & Sondheimer, J. (2012). Current diagnosis and treatment (21st ed.). NY, New york: McGrae Hill. Manson, J. J., & Rahman, A. (2009). Systemic lupus erythematosus. Orphanet Journal of Rare Disease, 1(6). Sato, V., Marques, I., Goldenstein, P., Carmo, L., Jorge, L., Titan, S., Barros, R., & Woronik, V. (2012). Lupus nephritis is more severe in children and adolescents than in older adults. Lupus, 21. SYSTEM LUPUS ERYTHEMATOSUS IN CHILDREN Systemic lupus erythematosus:Primer for managed care. (2012). America Journal of managed care, 18. 10