The EEG background
advertisement

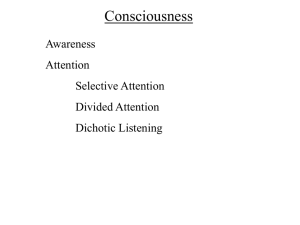
EEG for Dummies/Med Students Funfacts: -EEG (electroencephalogram) uses electrodes placed on the scalp to measure brain electrical activity, BY COMPARING ONE ELECTRODE TO ANOTHER. Montages (the lens through which you view the data): -A-P Bipolar: Good “all-around” montage. Best to compare anterior vs. posterior. Compares pairs of electrodes to one another. Field points TOWARD the abnormal electrode (“sandwiches” it) -Average Reference: Compares all electrodes individually to the same, single fixed point of reference. Abnormal electrode is the “biggest” deflection, with deflections in other electrodes getting bigger the closer you are to the abnormal electrode. -Transverse: Best to compare side to side. Field points TOWARD the abnormal electrode. Lead placement The EEG background: Transverse Bipolar Frequency/rhythm: the speed of the EEG waves. There is no inherently “correct” or “incorrect” wave, it depends on the context (awake, sleeping, etc) Alpha: 8-13 Hz (Hz= waves per second/big box) Beta: >13 Hz. Theta: 4-7 Hz Delta: 1-3 Hz Normal PDRs (by age): -3 months = at least 3Hz -1 year = 5-6Hz -3 years =8 Hz >8 years = > 8.5 Hz Normal Stuff, variants, and Artifacts: 1. Mu waves: frontocentral alpha rhythm that disappears when pt. opens and closes contralateral hands. 2. Blinking: Big symmetric downward deflection in frontal/eye leads, b/c eyes roll up in head when you close your lids. 3. Eye movement: Look at F7 and F8. Eyes up=downward deflection, eyes down= upward deflection, eyes left or right = “open vs. closed window” rule. 4. Muscle artifact: Dark super-fast squiggly lines, or big deflections in one lead without a field change or effect on other leads 5. Breach rhythm: missing part of your skull, so over that region get high amplitude sharp fast discharges. 6. Positive occipital sleep transients(POSTs): sail-shaped, in posterior leads. Occur at end of stage 2 sleep. 7. Lambda: Basically awake POSTs, demonstrate patient is scanning with their eyes/watching TV. Putting blank piece of paper in front of their eyes should end it. 8. BETS (benign epileptiform transients of sleep) tiny temporal spikes. 9) EKG artifact 10) Electrodes shaking Sleep: **NOTE: Normal but scary-looking stuff happens during sleep/wake transitions, be careful what you call abnormal here** -Stage 1 (drowsiness): Central vertex waves, slow lateral eye movements, alpha waves <50% of epoch, intermittent slow waves. Ends with POSTS (Positive occipital sharp transients of sleep, ie upside-down posterior sharps) -Stage 2 (real sleep): K complexes (central-maximum big diphasic slow wave followed by spindles) and spindles (central runs of Beta waves, < 2 seconds), markedly low amplitude background. -Stage 3-4: Delta and theta slowing, >50% of recording. -REM: Rapid eye movements, muscles paralyzed, occasional runs of alpha. Central sawtooth waves. Ways to sort out that something on the EEG is abnormal: 1. Is it different than the rest of patient’s background (look odd, bigger, etc)? Is the background itself wonky? 2. Have you ruled out artifact (blinking, sleep/wake transition, EKG artifact, etc)? 3. Is it spiky? Is it a slow, fat wave? Is it asymmetrical? 4. Does it have a field/phase reversal associated with it? (careful: if abnormal electrode is at end of chain, you may not see the field/phase reversal…hence the need for multiple montages) 5. Is it a seizure (does it evolve in frequency, location/spread; less importantly, does it have change in morphology(sharp) or amplitude while being rhythmic/repetitive, does it have a beginning and end, does it last >10 seconds)? Other specific abnormalities: 1) “Epileptiform activity”= pattern demonstrating increased risk of having seizure, usually from the region you see the activity. Epileptiform patterns include spike and wave, sharps, PLEDs, GPEDs, TIRDA, BIPLEDS. A seizure also counts as epileptiform activity. Slowing by itself is NOT necessarily epileptiform. 2) Spikes= less than 70 ms long. Sharps= greater than 70ms long. Difference is arbitrary. 3. Focal slowing: Intermittent (non-specific neuronal dysfunction in that region) vs. constant (structural lesion) 4. Encephalopathy: Mild (mild slowing 7-8Hz PDR, normal sleep and reactivity), moderate (moderate slowing 4-6Hz, lose sleep architecture but see background activity and variability), severe (<4 Hz, no variability, no sleep architecture), profound (nearly flat). 5. PLEDS (periodic lateralized epileptiform discharges): 0.5-2Hz, big, stereotyped, repetitive. Seen most commonly after infarction/acute injury, or seizure. Usually go away after a few weeks. 6. GPEDS: Generalized periodic epileptiform discharges, basically bilateral PLEDS. 7. Burst suppression: long periods of suppression, punctuated by bursts of sharp/slow. Seen in hypoxia, hypothermia, anesthesia, trauma. 8. BiPLEDS: bilateral INDEPENDENT PLEDs; 70% of people with this have seizures. 9. Triphasic waves: 0.5-2 second interval negative-positive-negative wave. Suggest metabolic or infectious process. 10. FIRDA: Frontally dominant intermittent rhythmic delta activity; big waves; suggests encephalopathy (most commonly metabolic). 11. OIRDA: occipital “ “ “ “ (big, bilateral, synchronous). Associated with absence epilepsy. 12. TIRDA: Temporal “ “ “. Epileptiform from that region; associated with structural lesions (get imaging if you see it). BASICALLY MEANS YOU HAVE EPILEPSY. 13) Status epilepticus: One single lasting longer than 30 minutes, or 30 minutes of seizures not returning to baseline. How to methodically read an EEG: 1. What is the posterior dominant rhythm (PDR) ? (Where is it most noticeable? how many Hz is the occipital rhythm, is it alpha/beta/theta/delta/can’t tell? Is it symmetrical? Big or little amplitude? Rhythmic or irregular? measure from when the eyes are close, but patient is as awake as possible) 2. What does the background look like in general? Is it symmetric, uniform? What rhythms are seen (beta, delta, etc)? 3. ABNORMALITIES: A) Any epileptiform activity? CAN IT BE A NAMED NORMAL VARIANT? Describe them (spikes/sharps/waves/sharplycontoured, frequency, diffuse vs. focal, location, symmetry, continuous/intermittent/episodic/paroxysmal, quantity) B) Any focal slow waves (theta/delta)? Are they intermittent or constant? C) Any seizures (evolving (frequency, spread; less important change in amplitude or clear onset/ending), rhythmic, different from background, etc)? Where do they start/spread to/how long they last/what is their frequency and morphology/what happens clinically? D) Any clinical events (describe them, and if they have EEG correlate; as a general rule, more than 3 seconds of continuous epileptiform activity should impact behavior) 4. Stages of sleep 5. Photic driving? (ie, does PDR synchronize with at least one of the photic frequencies? Is it symmetrical? Does it bring out abnormalities?) 6. Hyperventilation (does it cause physiologic slowing? Does it bring out abnormalities?) 7. EKG? 8. Read the patient’s story, prior imaging, prior EEGs, current meds that could be influencing EEG. Based on that, does that change your read or make you want to look for something specific? “WHAT THE HELL DOES THIS REPORT MEAN?!” 1. Is it normal or abnormal? 2. Are there epileptiform discharges (Sharp/spikes/waves, PLEDs, seizures, etc.)? Epileptiform means INCREASED RISK OF SEIZURE, not necessarily that they are HAVING seizures. 3. Is there slowing or encephalopathy? 4. Are there any events, and are they seizure? 5. How’s the EKG? EXAMPLES: Alpha, Beta, Theta, and Delta waves Stage 1 sleep with central vertex wave, suppressed background: Stage 2 sleep with K complex and spindles Stage 3 sleep (delta predominance) REM Sleep (draw this) Mu rhythm Single spike and wave in temporal lobe (epileptiform) Burst suppression Triphasic waves: PLEDS: Generalized seizure (changed morphology, frequency, amplitude; rhythmic, symmetric)