Neuro Study Guide - My Illinois State
advertisement

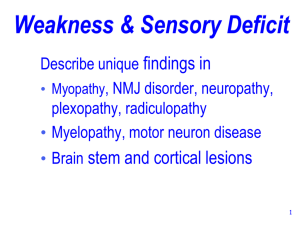
MENNONITE COLLEGE OF NURSING AT ILLINOIS STATE UNIVERSITY Diagnostic Reasoning for Advanced Practice Nursing 431 MODULE: NEUROLOGICAL SYSTEM OBJECTIVES: Upon completion of this module, the student will be able to: 1. Describe the overall neurological assessment process, including mental status, cranial nerves, sensory, motor, coordination, and reflexes. 2. Perform an appropriate neurological assessment on a client. 3. Incorporate appropriate aspects of the complete neurological assessment into the routine examination of clients. REQUIRED READINGS: Read applicable sections of the course textbook. EQUIPMENT NEEDED: Ophthalmoscope Penlight Reflex hammer Hand-held visual acuity card with 14” measure Cotton ball Tuning fork Safety pin or broken Q-tip Key, paper clip, coins Aromatic substance MODULE: NEUROLOGIC SYSTEM STUDY QUESTIONS: 1. Define/Describe: a. Aphasia b. Athetosis c. Ataxia d. Clonus e. Fasciculation f. Graphesthesia g. Hyperesthesia h. Myoclonus i. Proprioception j. k. l. m. Romberg Spasticity Stereognosis Tremor 2. List the cardinal symptoms of the neurologic system. 3. What are the five main components of the neurological examination? 4. Name the cranial nerves and describe the main function of each, including their motor and/or sensory function. 5. Describe the sensory pathway from receptor to the sensory cortex for each of the following sensory components: a. Touch b. Pain c. Temperature d. Vibration e. Proprioception 6. Describe the pathway of the reflex arc. 7. Differentiate upper and lower motor neuron dysfunction. 8. Describe the function of the cerebellum. How would you test? 9. List the components of the Mental Status exam. 10. If you are screening for sensory intactness and using only two tests, why would vibration and pain be good choices? 11. What is the appropriate method of testing pain sensation? 12. What does the recognition of dullness when testing for pain mean? 13. Define the grading system for deep tendon reflexes. 14. Describe a Babinski reflex and its clinical significance. NEUROLOGICAL ASSESSMENT I. History A. Headaches: type of pain (quality), warning prodromal signs, location, radiation, factors that worsen or improve the pain, duration and frequency of pain, associated symptoms (nausea, vomiting, duration and frequency of paresthesias, weakness, seizures, muscle stiffness or soreness, fever, weakness). Time of day of onset, age at previous onset, hospitalizations, drug therapy and effects. Family history of similar type of headache. Medications: BCPs B. Seizure: unpleasant odor or taste; focal numbness, pain, prickling; auditory whistling, ringing; visual disturbances, shapes, colors, movements, hallucinations, repetitive movements of a body part, muttering, crying; nonattention, generalized convulsions. C. Transient neurological dysfunction: aphasia, unconsciousness, motor or sensory deficits, weakness, tinnitus, vertigo, abnormal sensations D. Pain: ask patient to outline the affected area using one finger. Quality, precipitating and relieving factors, associated symptoms. E. Weakness: focus on activities of daily living and involved body parts 1. Distal vs. proximal—lower extremities a. Tripping over carpet or cords (distal) b. Stepping up to a bus or getting up from a chair (proximal) 2. Distal vs. proximal -- Upper extremities a. Writing, shaking hands (distal) b. Lifting arms, combing hair (proximal) F. Stroke: what was patient doing at onset; presenting symptoms, any of the following: altered level of consciousness, aphasia, headache, stiff neck, cranial nerve symptoms (blindness, tinnitus, vertigo), weakness numbness, paralysis, trouble with gait uncoordination, seizures 1. Associated symptoms: chest pain, dysrhythmia, valvular heart disease, MI, diabetes, BCPs 2. Course since onset 3. Functional capacity II. Physical Assessment: Refer to course textbook for the particular of the neurologic exam. However, a screening exam of the neuro system is outlined below—to be used for a general assessment on a well physical examination A. Assessment of mental status B. Evaluation of cranial nerves—remember most of this can be done with HEENT exam C. Assessment of motor function, including 1. Walking 2. Knee bends (if patient is able) 3. Hopping 4. Balance (Romberg) 5. Heel-toe walking D. Evaluation of sensory function, including 1. Vibratory sensation in the hands and feet 2. Sharp and dull testing in the hands and feet E. Assessment of coordination 1. Hand coordination 2. Position sense F. Assessment of DTRs G. Developmental status at appropriate ages Neuromuscular Changes in the Elderly Permanent neuronal loss occurs with aging: brain weight decreases by 5-17%. Reaction time also decreases secondary to decreases in lens transparency, pupil size, and changes in the vitreous humor and retina, decreased numbers of axons and slowed conduction at the synapse. Deep tendon reflexes decrease as well as conduction velocities in peripheral nerves. The hearing threshold deteriorates with age and there is a decrease in directional hearing. Neurological findings in the elderly may include changes in mental status, weakness, abnormal reflexes, and abnormal posture and gait. NEUROLOGICAL: COMMON ABNORMALITIES Assessment Findings Impaired ability to remember words Aphasia Dysarthria Concrete response to proverb interpretation Loss of sense of smell Visual field defects Pupillary reactions (dilation, constriction, abnormal reactions to light) Ptosis Abnormal extraocular movements Diplopia Facial asymmetry Incoordination Unsteady, wide-based, slapping gait Staggering, unsteady, wide-based gait with difficulty turning Gait with hip and knee flexion, short shuffling steps, minimal arm swing Steppage gait—with foot drop Difficulty performing knee bends Symmetrical distal sensory loss Loss of discriminative sensation Hyperactive reflexes Causes Causes include mental retardation, depression, dementia, anxiety, thiamine deficiency, chronic alcoholism, head injury May be due to a stroke, diffuse cortical damage, or a progressive lesion Damage to the central or peripheral nervous system Schizophrenia, organic brain syndrome, mental retardation Head injuries or tumor Lesions of the optic tract or occipital lobe, glaucoma, temporal or parietal lobe lesion, pituitary tumor Drug use, third nerve or optic nerve lesions Damage or paralysis of the third nerve, tumor, aneurysm, head trauma, vascular lesions, meningitis Lesions of the 4th or 6th cranial nerves; causes include increased intracranial pressure, pressure from a tumor or aneurysm, syphilis, meningitis, vascular lesions, head trauma Multiple sclerosis, myasthenia gravis, cerebral atheroma Bell’s palsy, upper motor neuron paralysis, flattened nasolabial folds (hemiparesis), abnormal facial movement Sensory loss, cerebellar lesions Sensory ataxia Cerebellar ataxia Parkinson’s disease Lower motor neuron disease Proximal hip girdle weakness Peripheral neuropathy Lesion of the sensory cortex or posterior columns Upper motor neuron disease