phys chapter 82 [9-25
advertisement

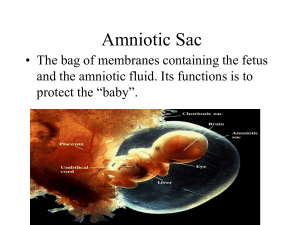
Phys Chapter 82 Transport of Fertilized Ovum Takes 3-5 days for fertilized ovum to go through remainder of fallopian tube into uterus Transported by feeble fluid current in tube resulting from epithelial secretion plus action of ciliated epithelium that lines tube – cilia always beat towards uterus o Weak contractions of fallopian tube may also aid ovum passage Fertilized ovum enters uterus as blastocyst (about 100 cells) Implantation Blastocyst usually remains in uterine cavity for 1-3 days before implantation in endometrium Before implantation, blastocyst obtains nutrition from uterine endometrial secretions called “uterine milk” Implantation results from action of trophoblast cells – secrete proteolytic enzymes that digest and liquefy adjacent cells of uterine endometrium o Some fluid and nutrients released actively transported by same trophoblast cells into blastocyst, adding more sustenance for growth Early Nutrition of Embryo During second half of monthly cycle, secretion of progesterone causes endometrium stromal cells to convert into large swollen cells containing extra quantities of glycogen, proteins, lipids, and some minerals necessary for development of conceptus When conceptus implants in endometrium, continued secretion of progesterone causes endometrial cells to swell further and store even more nutrients Endometrial stromal cells then called decidual cells and total mass of cells called decidua As trophoblast cells invade decidua, the stored nutrients in the decidua are used by the embryo for growth and development o During first week after implantation, this is the only source of nutrition o Embryo continues to obtain at least some of its nutrition this way for up to 8 weeks, although placenta begins to provide nutrition after about 16th day after fertilization Function of Placenta While trophoblastic cords from blastocyst are attaching to uterus, blood capillaries grow into cords from vascular system of embryo Blood sinuses supplied with blood from the mother develop around outsides of trophoblastic cords around day 21 Trophoblast cells send out more and more projections (placental villi) into which fetal capillaries grow Mother’s blood flows from uterine arteries to large maternal sinuses that surround villi and then back into uterine veins of mother Nutrients and other substances pass through placental membrane mainly by diffusion like in alveolar membranes of lungs and capillary membranes in adult body Placental Permeability and Membrane Diffusion Conductance In early months of pregnancy, placental membrane is still thick because it is not fully developed, and thus permeability is low o At this time, surface area is small because the placenta has not grown significantly, so total diffusion conductance is small In later pregnancy, the permeability increases because of thinning of the membrane diffusion layers and surface area expands many times over It is rare for breaks to occur in placental membrane to allow fetal blood into mother’s circulation and even more rare for mother’s blood to enter fetal circulation Near end of pregnancy, mean PO2 of mother’s blood in placental sinuses is about 50 mm Hg, and mean PO2 in fetal blood after becoming oxygenated in placenta is about 30 mm Hg Three reasons why fetus is able to survive on this low PO2 level o Fetal hemoglobin has higher affinity for O2, so these levels in fetal blood are the same as 20%-50% more in adult blood o Hemoglobin concentration of fetal blood is about 50% greater than that of mother o Bohr effect – hemoglobin can carry more oxygen at low PCO2 than at high PCO2 – fetal blood entering placenta carries large amounts of carbon dioxide, but much of this diffuses from fetal blood into maternal blood – loss of CO2 makes fetal blood more alkaline, whereas increased CO2 in maternal blood makes it more acidic – this causes fetal blood’s ability to combine with oxygen and decreases this ability of maternal blood PCO2 of fetal blood is 2-3 mm Hg higher than maternal blood, but easily allows for diffusion because of extreme solubility of CO2 in placental membrane Other nutrients diffuse the same way oxygen does o Glucose, fatty acids, ketone bodies, potassium, sodium, and chloride ions can diffuse with relative ease from maternal blood into fetal blood In late stages of pregnancy, fetus uses as much glucose as entire body of mother o To provide enough glucose, trophoblast cells lining placental villi provide for facilitated diffusion of glucose through placental membrane Hormonal Factors of Pregnancy Human chorionic gonadotropin secreted by syncytial trophoblast cells into fluids of mother as trophoblast develops o Can be detected in maternal blood as early as 8-9 days after fertilization (shortly after blastocyst implants in endometrium) o Level peaks between 10-12 weeks of pregnancy, then drops back down to a lower level it maintains for the rest of pregnancy o Most important function is to prevent involution of corpus luteum at end of monthly cycle, causing it to instead secrete even larger quantities of progesterone and estrogens, preventing menstruation and causing the endometrium to continue to grow and store large amounts of nutrients o Causes decidua-like cells of endometrium to become actual decidual cells (greatly swollen and nutritious) about time blastocyst implants o Corpus luteum is absolutely necessary to maintain pregnancy for first 7 weeks, and even up to 12 weeks, but begins to slowly involute after 13-17 weeks o HCG exerts interstitial-cell-stimulating effect on testes of male fetus, resulting in production of testosterone at time of birth – small secretion of testosterone during gestation is what causes fetus to grow male sex organs instead of female organs Estrogens and progesterone – secreted by corpus luteum and syncytial trophoblast cells of placenta o Toward end of pregnancy, placental estrogens increase to about 30 times mother’s normal level of production o Estrogens secreted by placenta not synthesized de novo, but formed almost entirely from androgenic steroid compounds formed in mother’s adrenal glands and adrenal glands of fetus – androgens transported by blood to placenta and converted by trophoblast cells into estradiol, estrone, and estriol Cortices of fetal adrenal glands are extremely large and about 80% consists of fetal zone, whose primary function is to secrete androgen precursor of estrogens during pregnancy During pregnancy, extreme quantities of estrogens cause enlargement of mother’s uterus, enlargement of mother’s breasts and growth of breast ductal structure, and enlargement of mother’s external genitalia o Estrogens also relax pelvic ligaments of mother so sacroiliac joints become relatively limber and pubic symphysis becomes elastic Progesterone – secreted in moderate quantities by corpus luteum at beginning of pregnancy and later secreted in tremendous quantities by placenta o Causes decidual cells to develop in uterine endometrium, which plays an important role in nutrition of early embryo o Decreases contractility of pregnant uterus, thus preventing uterine contractions from causing spontaneous abortion o Contributes to development of conceptus even before implantation because it increases secretions of mother’s fallopian tubes and uterus to provide appropriate nutritive matter for developing morula and blastocyst – reason to believe it also affects cell cleavage in early embryo o Helps estrogen prepare mother’s breasts for lactation Human chorionic somatomammotropin – begins to be secreted by placenta at about 5th week of pregnancy and increases progressively throughout remainder of pregnancy in direct proportion to weight of placenta o Causes at least partial development of breasts and can cause lactation o Causes formation of protein tissues in same way growth hormone does (much weaker version of growth hormone though) o Causes decreased insulin sensitivity and decreased utilization of glucose in mother, thereby making larger quantities of glucose available to fetus o Promotes release of free fatty acids from fat stores of mother, providing this alternative energy source during pregnancy Other Hormonal Factors in Pregnancy Anterior pituitary gland enlarges at least 50% during pregnancy and increases production of corticotropin, tyrotropin, and prolactin – secretion of FSH and LH is almost totally suppressed as a result of inhibitory effects of estrogens and progesterone from placenta Increased corticosteroid secretion o Glucocorticoids moderately increased throughout pregnancy to help mobilize amino acids from mother’s tissues to be used for synthesis of tissues in fetus o Aldosterone – about twofold increase, reaching peak at end of gestation – causes tendency to reabsorb excess sodium from renal tubules and thus retain fluid, occasionally leading to pregnancy-induced hypertension Increased thyroxine secretion from thyroid gland – caused at least partly by thyrotropic effect of HCG secreted by placenta and small quantities of TSH (human chorionic thyrotropin) also secreted by placenta Increased PTH secretion – causes calcium absorption from mother’s bones, maintaining normal calcium ion concentration in mother’s extracellular fluid even while fetus removes calcium to ossify its own bones – secretion even more intensified during lactation because growing baby requires much more calcium than fetus does Relaxin – secreted by ovaries and placenta – secretion increased by stimulating effect of HCG when corpus luteum and placenta secrete large quantities of estrogen and progesterone o Causes relaxation of ligaments of pubic symphysis and softens cervix at time of delivery Response of Mother’s Body to Pregnancy Uterus becomes about 22x its normal size, breasts double in size, vagina enlarges and introitus opens more widely Various hormones can cause marked changes in appearance sometimes, resulting in development of edema, acne, and masculine or acromegalic features Average weight gain during pregnancy is 25-35 lbs. with most of this occurring during last 2 trimesters o 8 lbs. or so is fetus o 4 lbs. or so is amniotic fluid, placenta, and fetal membranes o Uterus increases 3 lbs. and breasts increase 2 lbs. o 5 lbs. is extra fluid in blood and extracellular fluid o 3-13 lbs. generally fat accumulation Extra fluid excreted in urine during first few days after birth (after loss of fluid retaining hormones from placenta) Metabolism during Pregnancy Basal metabolic rate increases about 15% during latter half of pregnancy o Because of this, she can frequently become overheated o Also because of extra baby weight, she has to use greater amounts of energy for muscle activity By far, greatest growth of fetus occurs during last trimester of pregnancy – weight almost doubles during last 2 months o Mother doesn’t just absorb enough nutrients to provide for this, so in advance, mother’s body stores these nutrients in placenta and normal storage spots of mother’s body If mother does not have appropriate stores of nutrients, she can become deficient in calcium, phosphates, iron, and vitamins o Iron is important for hemoglobin formation for both baby and mother because of increased blood levels o Vitamin D is important to aid in calcium absorption o Vitamin K is often added to mother’s diet shortly before birth so that baby will have sufficient prothrombin to prevent hemorrhage, particularly brain hemorrhage, caused by birth process Changes in Maternal Circulatory System Blood flow through placenta and maternal cardiac output increases during pregnancy Maternal blood volume increases during pregnancy – as much as 30% above normal o Occurs mainly during latter half of pregnancy due to aldosterone and estrogens and fluid retention of kidneys o Bone marrow becomes increasingly active and produces extra RBCs to go with excess fluid volume o At time of birth, mother has 1-2 extra liters of blood About ¼ of this is lost during delivery Maternal respiration increases during pregnancy o Need for more oxygen (20% above normal) o High levels of progesterone during pregnancy can increase minute ventilation because progesterone increases respiratory center’s sensitivity to CO2 Also causes decrease in arterial PCO2 by several mm Hg in mother o Growth of uterus presses against diaphragm, so total excursion of diaphragm is decreased Maternal kidney function during pregnancy o Rate of urine formation is slightly increased because of increased fluid intake and increased load of excretory products o Renal tubules’ reabsorptive capacity for sodium, chloride, and water is increased by as much as 50% as a consequence of increased production of salt and water retaining hormones o Renal blood flow and glomerular filtration rate increase by up to 50% during pregnancy due to renal vasodilation Increased glomerular filtration rate occurs as compensation for increased tubular reabsorption of salt and water Normal volume of amniotic fluid is 0.5-1 L o On average, water in amniotic fluid is replaced once every 3 hours and sodium and potassium are replaced once every 15 hours o Large portion is derived from renal excretion by fetus o Certain amount of absorption occurs by way of GI tract and lungs of fetus o Some fluid is formed and absorbed directly through amniotic membranes (so there is still some turnover of amniotic fluid after in utero death of fetus) Preeclampsia – rapid rise in arterial blood pressure in mother to hypertensive levels during last few months of pregnancy with leakage of large amounts of protein into urine o Characterized by excess salt and water retention by mother’s kidneys and by weight gain and development of edema in mother o Impaired function of vascular endothelium and arterial spasm occur in many parts of mother’s body, most significantly in kidneys, brain, and liver o Both renal blood flow and glomerular filtration rate are decreased o Glomerular tufts thicken and contain protein deposit in basement membranes o Can result from autoimmune or allergy in mother caused by presence of fetus o Can be initiated by insufficient blood supply to placenta, resulting in placenta’s release of substances that cause widespread dysfunction of maternal vascular endothelium o In patients with preeclampsia, maternal arterioles fail to undergo usual adaptive changes (remodeling of maternal arterioles into large blood vessels with low resistance to blood flow caused by trophoblast invasion), causing insufficient blood supply to placenta, which causes placenta to release substances that enter mother’s circulation and cause impaired vascular endothelial function, decreased blood flow to kidneys, excess salt and water retention, and increased blood pressure Suggested factors for inducing this include inflammatory cytokines such as tumor necrosis factor-α and interleukin-6 Placental factors that impede angiogenesis can also contribute to increased inflammatory cytokines and preeclampsia Antiangiogenic proteins “soluble fms-related tyrosine kinase 1” (s-Flt1) and “soluble endoglin” are increased in blood of women with preeclampsia – these are released by placenta into maternal circulation in response to ischemia and hypoxia of placenta Eclampsia – extreme degree of preeclampsia characterized by vascular spasm throughout body, clonic seizures in mother (sometimes followed by coma), greatly decreased kidney output, malfunction of liver, often extreme hypertension, and generalized toxic condition of body o Usually occurs shortly before birth o Without treatment, a high percentage of mothers with this will die o With optimal and immediate use of vasodilating drugs to reduce arterial pressure, followed by immediate termination of pregnancy (by C-section if necessary), mortality of eclamptic mothers has been reduced to 1% or less Parturition (birth) Towards end of pregnancy, uterus becomes progressively more excitable until it develops such strong rhythmical contractions that the baby is expelled o Major contributing factors include progressive hormonal changes that cause increased excitability of uterine musculature and progressive mechanical changes Hormone factors that increase uterine contractility o Increased ratio of estrogens to progesterone – progesterone inhibits uterine contractility (hence why it’s important to maintain pregnancy in the first place) and estrogens increase number of gap junctions between adjacent uterine smooth muscle cells (and have other effects) to increase uterine contractility From 7th month onward, estrogen secretion continues to increase while progesterone rate decreases o Oxytocin causes contraction of uterus Uterine muscles increase oxytocin receptors and, therefore, increase responsiveness to oxytocin during latter few months of pregnancy Rate of oxytocin secretion considerably increased during labor Irritation or stretching of uterine cervix, as occurs during labor, causes neurogenic reflex to increase secretion of oxytocin o Fetus’s pituitary gland secretes increasing quantities of oxytocin o Fetus’s adrenal glands secrete large quantities of cortisol (possible uterine stimulant) o Fetal membranes release prostaglandins in high concentration during labor (can increase intensity of uterine contractions) Mechanical factors that increase uterine contractility o Stretch of uterine musculature – natural stretch reflex of smooth muscles Intermittent stretch, as occurs in uterus because of fetal movements, can elicit smooth muscle contraction (hence why twins are usually born earlier than single babies) o Stretch or irritation of cervix Labor can be induced by rupturing membranes so head of baby stretches cervix more forcefully than usual or irritates it in other ways Onset of Labor During most of pregnancy, uterus undergoes periodic episodes of weak and slow rhythmical contractions (Braxton Hicks contractions) o Become progressively stronger toward end of pregnancy o Change suddenly to become exceptionally strong contractions that start stretching the cervix and later force baby through birth canal Positive feedback – stretching of cervix by fetus’s head finally becomes great enough to elicit strong reflex increase in contractility of uterine body, which pushes baby forward, which stretches cervix more, etc. Once strength of uterine contraction becomes greater than critical value, each contraction leads to subsequent contractions that become stronger and stronger until maximum effect is achieved 2 types of positive feedback increase uterine contractions during labor o Stretching of cervix causes entire body of uterus to contract – this contraction stretches cervix even more because of downward thrust of baby’s head o Cervical stretching causes pituitary gland to secrete oxytocin, which increases uterine contractility Uterine contractions cause pain signals that elicit neurogenic reflexes in spinal cord to abdominal muscles, causing intense contractions of abdominal muscles Mechanics of Parturition Uterine contractions begin at top of uterine fundus and spread downward over body of uterus Intensity of contractions is great in top and body of uterus but weak in lower segment of uterus adjacent to cervix In early part of labor, contractions might occur every 30 minutes, but as labor progresses, this time diminishes to once every 1-3 minutes – intensity of contractions increases greatly in this time, with only a short period of relaxation between contractions Combined contractions of uterine and abdominal muscles during delivery put about 25 lbs. of downward force on fetus during each strong contraction Strong contractions impede or sometimes even stop blood flow through placenta and would cause death of fetus if contractions were continuous Overuse of uterine stimulants can cause uterine spasm instead of rhythmical contractions, leading to death of fetus Baby’s head acts as a wedge to open structures of birth canal as fetus is forced downward First stage of labor – period of progressive cervical dilation, lasting until cervical opening is as large as head of fetus – can last 8-24 hours in first pregnancy or as little as a few minutes with experienced mothers Second stage of labor – once cervix is dilated fully, fetal membranes rupture and amniotic fluid is lost suddenly through vagina – fetus’s head then moves rapidly into birth canal – can last from 30 minutes in first pregnancies to 1 minute with experienced mothers Separation and Delivery of Placenta For 10-45 minutes after birth of baby, uterus continues to contract to a smaller and smaller size, which causes shearing effect between walls of uterus and placenta, thus separating placenta from implantation site Separation of placenta opens placental sinuses and causes bleeding – usually averages about 350 mL o Smooth muscle fibers of uterine musculature are arranged in figure eights around blood vessels as vessels pass through uterine wall o Contraction of uterus after delivery of baby constricts vessels that had previously supplied blood to placenta o Vasoconstrictor prostaglandins formed at placental separation site cause additional blood vessel spasm Labor Pains Cramping pain in early labor caused mainly by hypoxia of uterine muscle resulting from compression of blood vessels in uterus – not felt when visceral sensory hypogastric nerves, which carry visceral sensory fibers leading from uterus, have been sectioned During second stage of labor, more severe pain is caused by cervical stretching, perineal stretching, and stretching and tearing of structures in vaginal canal itself – pain conducted by somatic nerves instead of visceral sensory nerves Involution of Uterus after Parturition During first 4-5 weeks after parturition, uterus involutes – weight becomes less than half its immediate postpartum weight within 1 week and in 4 weeks, if mother lactates, uterus may become as small as it was before pregnancy o Results from suppression of pituitary gonadotropin and ovarian hormone secretion during first few months of lactation During early involution of uterus, placental site on endometrial surface autolyzes, causing vaginal discharge called lochia, which is first bloody and then serous in nature, continuing for about 10 days after delivery – after this time, endometrial surface becomes re-epithelialized and ready for normal, nongravid sex life again Lactation Breast development stimulated by estrogens of monthly female sexual cycle Estrogens stimulate growth of mammary glands plus deposition of fat to give breasts mass Far greater growth occurs during high-estrogen state of pregnancy, and only then does glandular tissue become completely developed for production of milk All through pregnancy, large quantities of estrogens secreted by placenta cause ductal system of breasts to grow and branch o Simultaneously, stroma of breasts increases in quantity and large quantities of fat are laid down in stroma Growth hormone, prolactin, adrenal glucocorticoids, and insulin are also important for ductal system because of their roles in protein metabolism Progesterone required for full development of lobule-alveolar system o Once ductal system has developed, progesterone (acting synergistically with estrogen and other hormones) causes additional growth of breast lobules, with budding of alveoli and development of secretory characteristics in cells of alveoli Both estrogen and progesterone inhibit the actual secretion of milk – milk secretion is enhanced by prolactin Concentration of prolactin in blood rises steadily from 5th week of pregnancy until birth of baby Because of inhibitory properties of estrogen and progesterone, no more than a few mL of fluid are secreted each day until after baby is born Colostrum – fluid secreted during the last few days before and the first few days after birth – contains essentially the same concentrations of proteins and lactose as milk, but has almost no fat and maximum rate of production is 1/100 that of milk production Immediately after baby is born, sudden loss of both estrogen and progesterone secretion from placenta allows lactogenic effect of prolactin from pituitary gland to assume natural milk-promoting role, and over next 1-7 days, breasts begin to secrete copious quantities of milk instead of colostrum Secretion of milk requires adequate background secretion of most of mother’s other hormones as well (GH, cortisol, PTH, and insulin) – necessary to provide amino acids, fatty acids, glucose, and calcium required for milk formation After birth of baby, basal level of prolactin secretion returns to nonpregnant level over next few weeks o Every time the mother nurses her baby, nervous signals from the nipples to the hypothalamus cause 1020x surge in prolactin secretion that lasts about an hour o This prolactin acts on the mother’s breasts to keep mammary glands secreting milk into alveoli for subsequent nursing periods o If nursing is discontinued, breasts lose their ability to produce milk within a week or so Milk production can last several years if the child continues to suckle, but milk formation normally decreases considerably after 7-9 months Hypothalamus inhibits prolactin production (prolactin inhibitory hormone) In most nursing mothers, the ovarian cycle and ovulation do not resume until a few weeks after cessation of nursing because the nervous signals from the breasts inhibit secretion of gonadotropin-releasing hormone by hypothalamus – this suppresses formation of pituitary gonadotropic hormones (LH and FSH) o After several months of lactation, especially in mothers who only nurse their babies some of the time, the pituitary begins to secrete sufficient gonadotropic hormones to reinstate monthly cycle, even though nursing continues Milk does not flow easily from alveoli into ductal system and thus does not continually leak from breast nipples o Milk must be ejected from alveoli into ducts before baby can obtain it – caused by combined neurogenic and hormonal reflex that involves posterior pituitary hormone oxytocin When baby suckles, it receives virtually no milk for first half minute or so o Sensory impulses transmit through somatic nerves from nipples to mother’s spinal cord then to hypothalamus, where they cause nerve signals that promote oxytocin secretion at the same time they cause prolactin secretion o Oxytocin is carried in blood to breasts, where it causes myoepithelial cells (which surround outer walls of alveoli) to contract, thereby expressing milk from alveoli into ducts – then baby’s suckling becomes effective in obtaining milk Many psychogenic factors or generalized SNS stimulation can inhibit oxytocin secretion and consequently depress milk ejection – this is why mothers need undisturbed period of adjustment after childbirth if they are to be successful at nursing their babies Milk Composition and Metabolic Drain on Mother Caused by Lactation Human milk has greater concentration of lactose than cow milk, but cow milk has more protein than human milk – human milk has about 1/3 the ash (calcium and other minerals) as cow milk At height of lactation, mother may produce 1.5 L of milk per day (more if mother had twins) Exact composition and caloric content of milk depends on mother’s diet and other factors such as fullness of breasts Large amounts of metabolic substrates are lost from mother (things that go into the milk) o Lactose in milk is converted from mother’s glucose o Unless mother is drinking large quantities of milk and has adequate intake of vitamin D, the output of calcium and phosphate by lactating mammae will often be much greater than intake of these substances o If calcium and phosphate levels insufficient, parathyroid glands enlarge greatly and bones become progressively decalcified – usually not a problem during pregnancy, but can become more important during lactation Multiple types of antibodies and other anti-infectious agents are secreted in milk along with nutrients – neutrophils and macrophages are also secreted in milk, including those that destroy E. coli When cow’s milk is used to supply nutrition for baby in place of mother’s milk, protective agents in it are usually of little value because they are normally destroyed within minutes in internal environment of human body