Document 6862697
advertisement

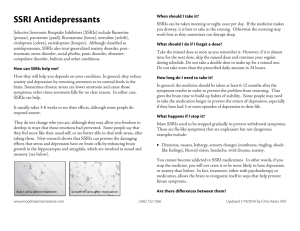
Table 1: A Look at the effects of antidepressants and depression on birth, the neonate, and the mother Outcome Birth Outcomes Miscarriage Effects on growth Low birth weight Small for gestational age Preterm delivery (less than 37 weeks’ gestation) Structural malformations Cardiac malformations Antidepressants Depression Increased risk with use in early pregnancy. Limitations: other factors not consistently controlled for. Increased risk for slower rates of head growth. Limitations: hard to determine duration of exposure, timing of exposure, how severe depression was, and other confounding factors. Increased risk with SSRI or TCA use. In some studies, accounted for by shorter gestational duration. Increased risk in mothers who used SSRIs (small risk however, compared with depressed mothers who did not take SSRIs) Inconclusive. Increased risk in some but not all studies (SSRIs, TCAs, SNRI/NRIs) Dependent on duration of in utero exposure: more exposure more likely reduction in gestational age. No association between SNRI/NRI use. Conflicting associations for TCA use. Conflicting association for SSRI use (specifically paroxetine) Conflicting results. No increased rate with SSRI exposure (4 studies). First trimester exposure to paroxetine increased risk of cardiac malformations (three studies); this increase not found in three other studies. Taking SSRI and benzodiazepine may increase congenital heart Inconclusive. Limitations of sample sizes and methodologies Increased risk for slower fetal body and head growth. Inconclusive. Increased risk in some but not all studies. Inconclusive. Increased risk in some but not all studies. Inconclusive Increased risk in some but not all studies. No studies No studies Other Neonatal Outcomes Behavioural Persistent pulmonary hypertension Long term growth, IQ, behavioural defects. Specific defects. Small risk and not replicated. Increased risk for irritability, jitteriness, seizures with TCA use. Increased risk for irritability, tachypnea, hypoglycemia, temperature instability, weak/absent cry, seizures (1530% of women who were exposed to SSRIs in late pregnancy); transient symptoms. Conflicting results: some studies show higher risk with later gestational exposure to SSRIs while other studies do not. Limited information; majority of studies do not show an association with SSRIs or TCAs. There have been reported subtle effects on motor and developmental control. As well, reaching developmental milestones compared to unexposed neonates has taken longer, but catches up by 19 months. Possible increased risk of autism spectrum disorder, however, small percentage due to SSRI exposure. Limitations: inability to control for severity, whether or not medication had been taken, and other risk factors. In comparing fluoxetine, TCAs, and controls, no difference in IQ, language, development, behavioural development. IQ negatively related to duration of depression. Language negatively correlated with the amount of depressive episodes after delivery. Maternal Outcomes No studies Increased risk for irritability, decreased activity and attentiveness, less facial expressions. No studies Depressed mothers at 18-32 weeks gestation resulted in greater developmental delays in infants. In another study, no difference. Limitations due to bias. Pregnancy-induced hypertension, pre-eclampsia and eclampsia Increased risk (50%-53%). Conflicting data. Limitations: control for depression and other confounding risk factors, linked databases, and medication use reported by the mother. Chaudron LH. Complex Challenges in Treating Depression During Pregnancy. Am J Psychiatry 2013; 170:12-20.