File
advertisement

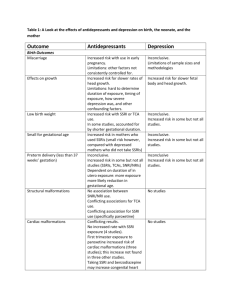
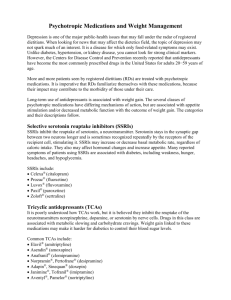
Antidepressants PRITE Review Samir Sabbag PGY-3 Psychiatry August 24, 2009 Overview Goal in Depresion Achieve complete remission With Treatment News – if remission: lower relapse rate Bad News – remitters have frequent relapses Good Suicide rates higher at ages 18-24 All effective Antidepressants boost DA, 5HT and NE Monoamine(MA) Hypothesis of Depression MA Boost Therapeutic Action 5HT NE DA 5HT NE DA NE DA 5HT NE DA NE DA 5HT 5HT NE DA 5HT Selective Serotonin Reuptake Inhibitors (SSRIs) Available SSRIs Fluoxetine (Prozac) Paroxetine (Paxil) Sertraline (Zoloft) Citalopram (Celexa) Escitalopram (Lexapro) Fluvoxamine ( Luvox) Mechanism of action All SSRIs inhibit reuptake of 5HT by presynaptic neurons SSRI Therapeutic Indications Depression OCD (give higher doses) Panic Disorder PTSD (help with intrusive and avoidant sx) GAD Premenstrual Dysphoric disorder Social Anxiety disorder Eating disorders (Fluoxetine) SSRI ½ lives and metabolites Fluoxetine Active Metabolite: 7-9 days Sertraline : longest ½ life 4-6 days! : 26h Active Metabolite: 3-5 days No active metabolites Citalopram : 35h Escitalopram : 27-32h Paroxetine : 21h (most likely to cause withdrawal reaction) Fluvoxamine : 15h SSRIs Plasma Protein binding Highly bound Fluoxetine, Sertraline and Paroxetine Least bound Escitalopram CYP 450 Fluvoxamine: marked 1A2, 2C and 3A Fluoxetine 2D6 effect on CYP and Paroxetine Least likely to cause problems Citalopram, Sertraline and Escitalopram SSRIs - General Side Effects Restlessness, psychomotor retardation, mild parkinsonism and dystonic movements (5HT-2A in basal ganglia) Myoclonus, sleep disturbance and nocturnal awakening (2A in brainstem) Sexual dysfunction, apathy and decreased libido (2A and 2C in spinal cord) N/V (5HT-3 in hypothalamus and brainstem) Increased bowel motility, GI cramps and diarrhea (5HT3 and 4 in GI tract) GI Sx Most common SE leading to discontinuation SSRIs - General Side Effects Suicide increased thoughts/actions in children, adolescents and young adults <25 Closely monitor first few weeks when starting SSRI Pregnancy Hematologic Small increase in anencephaly, craniosynostosis and omphalocele (as per population registries) Prolonged bleeding time - functional impairment of platelet aggregation Endocrine Can decrease glucose concentrations acutely SSRIs - General Side Effects Most common SE associated with long term treatment: Dysfunction – continues as long as the drug is taken Sexual Sleep disturbances Extremely vivid dreams or nightmares Bruxism, restless legs, nocturnal myoclonus Yawning associated with fatigue – effect of SSRI on hypthalamus Not Citalopram and Escitalopram Most selective inhibitors of serotonin reuptake Citalopram may have some sedative effects (H1) Citalopram Escitalopram Fluoxetine 5HT2C receptor block NE and DA release Increased energy Activation/anxiety Antibulimic/anorexic effects Boosts antidepressant action of Olanzapine in Bipolar Depression NE reuptake blockade Fluoxetine Of the SSRIs, most likely to cause headaches Can cause anxiety, specially during 1st weeks of use on the long run decrease anxiety SSRI most likely to cause insomnia Sertraline Atypical Depression Overeating and oversleeping Extreme sensitivity with interpersonal loss or rejection Severe psychomotor retardation Mood reactivity Sigma 1 action anxiolytic weak DA and NE reuptake inhibition Improves energy, motivation and concentration Helps with atypical depression Fist line in Panic d/o (also Paroxetine) Paroxetine Anticholinergic (M1) calming/sedating Good for anxiety sx weak NE reuptake inhibition antidepressant effects Nitric Oxide Synthetase (NOS) and 2D6 Sexual dysfunction Paroxetine Withdrawal reaction with sudden d/c Anticholinergic rebound Substrate and inhibitor for 2D6 Rapid decline in plasma when d/c First line in Panic disorder (also Zoloft) Anticholinergic activity Dry mouth, constipation, sedation Paroxetine Fetal abnormalities Cardiac malformation (R Ventricular outflow obstruction) Pulmonary hypertension Seen with doses >25mg in 1st trimester More frequent and pronounced weight gain than other SSRIs Fluvoxamine Not normally used as antidepressant Used for OCD, Panic d/o, PDD, Aggression in autism SSRI with the most DDI of all Serotonin Syndrome Constellation of sx composed, in order of appearance, by 1. 2. 3. 4. 5. 6. Diarrhea Restlessness Extreme agitation, hyperreflexia, autonomic instability with fluctuation of vital signs Myoclonus, seizure, hyperthermia, rigidity, shivering Delirium, coma, status epilepticus, cardiovascular collapse Death Serotonin Syndrome SSRI + MAOI, MAOB Inhibitors, L-Tryptophan, Lithium, SSRIs, SNRIs, TCAs, Buspirone, Meperidine, Nefazodone, Trazodone, Linezolid may raise SSRI to toxic levels Treatment Remove offending agent Supportive care nitroglycerine, methysergide, cooling blankets, chlorpromazide, dantrolene, benzodiazepines, anticonvulsants, mechanical ventilation, paralyzing agents Serotonin Syndrome May resemble NMS Serotonin Syndrome more likely to have Myoclonus Hyperreflexia GI symptoms NMS more likely to have Muscular rigidity SSRI Discontinuation Syndrome Abrupt discontinuation of SSRI Especially Shorter ½ lives Least Fluvoxamine and Paroxetine likely: Fluoxetine Longer ½ life Symptoms Dizziness, weakness, nausea, h/a, anxiety, rebound depression, poor concentration, upper respiratory sx, paresthesias. Tricyclic and Tetracyclic Antidepressants (TCAs) Tricyclics Which of the following is a secondary TCA? Protriptyline Clomipramine Maprotiline Amitriptyline Doxepine Available TCAs Tertiary Amines Secondary Amines Clomipramine Desipramine Imipramine Protriptyline Trimipramine Nortriptyline Amitriptyline Doxepin Tetracyclics Maprotyline Amoxapine Pharmacologic Actions Significant metabolism - 1st pass effect CYP450 2D6 (many meds may rise levels to toxic) Half-lives from 10-70 hours Longer Nortriptyline, Maprotiline and Protriptyline Pharmacologic Actions TCA’s block reuptake pumps NE and/or 5HT Most 5HT selective Clomipramine Most NE selective Desipramine TCA Receptor Structure Serotonin reuptake block NE reuptake block SIDE EFFECTS SIDE EFFECTS Histamine 1 receptor block Weight gain Doxepin most antihistaminergic of the TCAs SIDE EFFECTS Muscarinic (M1) receptor block Bethanecol Tx urinary retention (M1) Anticholinergic SE Can aggravate Narrow Angle Glaucoma Avoid TCAs in this condition – Amitriptyline Can cause Anticholinergic Delirium Especially if TCA used with dopamine receptor antagonist or anticholinergics Treatment: IM or IV physostigmine Least Anticholinergic Amoxapine, Nortriptyline Desipramine, Maprotiline SIDE EFFECTS Alpha-1 adrenergic receptor block Most common cause of TCA d/c Orthostatic Hypotension Overdose with TCAs TCAs – block voltage-sensitive Na channels – coma, seizures Heart – arrhythmia, death Brain OD –monitored with EKG Most frequent cause of death: arrhythmia EKG changes: PR, QRS, QTc prolongation Very common cause for discontinuation: Tachycardia Uses in Depression Melancholic Features Depressed mood Severe anhedonia Early morning awakening Weight loss Profound guilt Very effective More likely to induce mania than bupropion or SSRIs Better response Melancholic features, prior major depressive episodes, family hx In the US Clomipramine only approved for OCD Other Uses Panic disorder Imipramine – FDA approved OCD Only – most studied drug GAD Doxepin Clomipramine – use first SSRIs Pain and Migraine prophylaxis Amitriptyline TCAs have caused SUDDEN DEATH in children and adolescents! – used most often Childhood enuresis Imipramine Special Considerations Amoxapine May cause Parkinsonian sx Avoid in Parkinson’s Disease Blood levels of 4 TCAs can be monitored Nortriptyline, Desipramine, Clomipramine and Imipramine Nortriptyline: THERAPEUTIC WINDOW TCAs have low risk for inducing seizures Except for Maprotiline May cause seizures when dose increased too fast or kept at hight doses Clomipramine and Amoxapine May lower seizure threshold DO NOT give TCAs during ECT! serious cardiac effects Special Considerations Nortriptyline least Desipramine and Protriptyline most likely to cause orthostatic hypotention activating of the TCAs Relative contraindication for TCA use Bundle branch block Cardiac disease or age >40 Do EKG prior to TCA use Drug Interactions CYP 1A2, 2D6 and 3A4 dirty drugs Birth control pills and nicotine decrease TCA levels Fluoxetine, Fluvoxamine and Paroxetine increase TCA levels x4!! (CYP 2D6) If used together use lower dose of TCA Antipsychotics and Methylphenidate increase TCA levels Monoamine Oxidase Inhibitors (MAOIs) Therapeutic Indications Depression Atypical Depression Panic Disorder Bulimia PTSD Migraine ADD Available MAOIs Irreversible Phenelzine Tranylcypromine Reversible/Selective MAO-A (RIMA) Moclobemide Isocarboxazid (not in the US) Selective MAO-B Selegiline (transdermal patch) Pharmacokinetics MAOIs inhibit MAO A and B Stops MAO from destroying NE, 5HT and DA Increasing these neurotransmitters Irreversible MAO enzyme synthesized again in 2 weeks Need for dietary restrictions Washout period needed when starting a new antidep. Reversible MAO enz synthesized again in 24-48h Flexible dietary restrictions Irreversible MAOIs MAOI MAOI Two things to know about MAOIs: Serotonin Syndrome fentanyl SSRIs SNRIs clomipramine meperidine (Demerol) Hypertensive Crisis Mainly NE Tyramine (Sublimaze) Lithium/Carbamazepine Tryptophan Other opioids (methadone, tramadol) Hypertensive Crisis Tyramine in diet + MAO-A inhibition in gut NORMALY, in someone not taking MAOIs… NE NE MAO-A destroys NE Alpha-1 receptors Hypertensive Crisis Tyramine containing products Aged Cheese Tap beers Smoked fish Fava beans NE MAO-A NE Alpha-1 receptors MAO-A Hypertensive Crisis Irreversible MAOI + NE NE Alpha-1 receptors Interesting facts Selegiline Inhibits MAO-B no destruction of MAO-A in the gut not involved with intestinal tyramine reaction no dietary restrictions HTN crisis Can also be caused by DDI pseudoephedrine Side Effects Most frequent side effect Orthostatic Hypotension Other SE Insomnia Dizziness Weight Paresthesias gain Edema Sexual Switch to mania dysfunction Contraindicated in pregnancy and nursing Bupropion (Wellbutrin) Pharmacokinetics NE and DA reuptake inhibitor 3 formulations available DRI immediate release (TID) sustained release (BID) extended release (QD) Bupropion 3 active metabolites hydroxybupropion threohydroxybupropion erythrohydroxybupropion NRI Therapeutic Indications Depression Seasonal Affective Disorder (SAD) DA reward pathways ADHD the only FDA approved antidepressant fist line treatment: phototherapy Smoking cessation comparable efficacy to SSRIs second line agent appropiate for comorbid ADHD and depression Hypoactive sexual desire self or additive to other antidepressants (SSRIs) The Good, the Bad and the Ugly The GOOD No sexual dysfunction Safe in pregnancy (class B) No anticholinergic effects No weight gain No drowsiness No orthostatic hypotension/cardiovascular Side Effects The BAD Insomnia but increases REM sleep Anxiety Not good for panic d/o or anxiety GI distress (especially nausea) Restlessness/Agitation Hypertension Psychotic symptoms Side Effects The UGLY Seizures Incidence is 0.05% with 300mg or less Risk increases with doses >400mg per day May 0.1%!! cause death with OD Uncontrollable seizures Sinus bradycardia Cardiac arrest Selective SerotoninNorepinephrine Reuptake Inhibitors (SNRIs) SNRIs Venlafaxine (Effexor) Depression GAD Social anxiety disorder Desvenlafaxine Succinate (DVS)(Pristiq) Duloxetine (Cymbalta) Depression GAD Diabetic Neuropathic Pain Pharmacokinetics Selective NE and 5HT reuptake inhibitors TCAs do too, but not selective (SE!) Potent inhibitor of NE and 5HT Weak inhibitor of DA reuptake At lower doses – act like SSRIs At higher doses – inhibit NE and 5HT No activity in Cholinergic (M1) Histaminergic (H1) Adrenergic (alpha1) Pharmacokinetics Half lives – 3.5 hours ODV – 9 hours Duloxetine – 12 hours Venlafaxine Discontinuation Syndrome! P450 Venlafaxine – 2D6 Active metabolite O-desmethylvenlafaxine (ODV) Duloxetine – 2D6 and 1A2 Side Effects Venlafaxine Most common: nausea, sedation, dry mouth, dizziness, anxiety, nervousness, insomnia, weigh loss, constipation Sexual dysfunction HTN at higher doses Midryasis – monitor patients with acute narrow-angle glaucoma Platelet aggregation (serotonin-related impairment) In pts with liver disease – decreased clearance Side Effects Duloxetine Most common Nausea SE leading to discontinuation Liver toxicity Avoid in Hepatic insufficiency ESRD Uncontrolled No HTN narrow-angle glaucoma Mirtazapine (Remeron) Pharmacokinetics Does NOT work by inhibiting reuptake of NE and 5HT! Mechanism of Action Antagonist Mirtazapine of central presynaptic alpha-2 adrenergic receptors Increased release of NE and 5HT from neurons Blocks postsynaptic 5HT-2 and 3 receptors Decreases anxiety, stimulates appetite, relieves insomnia, decreased nausea and diarrhea Strong antagonist of histamine H1 receptors sedation at low dose – weaker at higher doses Therapeutic Indications Depression melancholic features elderly Augmentation with SSRIs or Venlafaxine counteract nausea, agitation and insomnia NO CYP 450 effects! Cancer patients GI side effects of chemotherapy sedation and stimulation of appetite Side Effects Weight gain and stimulation of appetite Somnolence in more than 50% of persons avoid alcohol and sedating OTC potentiates sedative effects medications ↑ cholesterol, triglycerides and ALT Dizziness In some orthostatic hypotension Agranulocytosis Low incidence of sexual SE Nefazodone and Trazodone Nefazodone Shortest ½ life of all antidepressants 2-3 hours! Active metabolites hydroxynefazodone (principal) mCPP (meta-chlorophenylpiperazine) 5HT effects – migraine, anxiety and weight loss Nefazodone Orthostatic hypotension, dry mouth, sedation No sexual dysfunction No anticholinergic SE Increases REM sleep Cytochrome P450 3A4 elevation of Antianxiety, antidepressant and somnolence Alprazolam Triazolam Haldol Digoxin Therapeutic Indications Depression Panic disorder Premenstrual dysphoric disorder GAD Chronic pain PTSD Chronic fatigue syndrome Nefazodone When switching from SSRI to Nefazodone Won’t protect from withdrawal symptoms High risk for hepatotoxicity Trazodone Active metabolite mCPP (metachlorophenylpiperazine) Migraine, anxiety, weight loss Strong anti H1 effect Use in insomnia ↓ REM sleep ↑ total sleep time ↓ number and duration of nighttime awakenings Trazodone More risk of orthostatic hypotension than Nefazodone (alpha 1) ½ life 5-9 hours Can cause priapism