Antipsychotic Drugs and Mood Stabilizers
advertisement
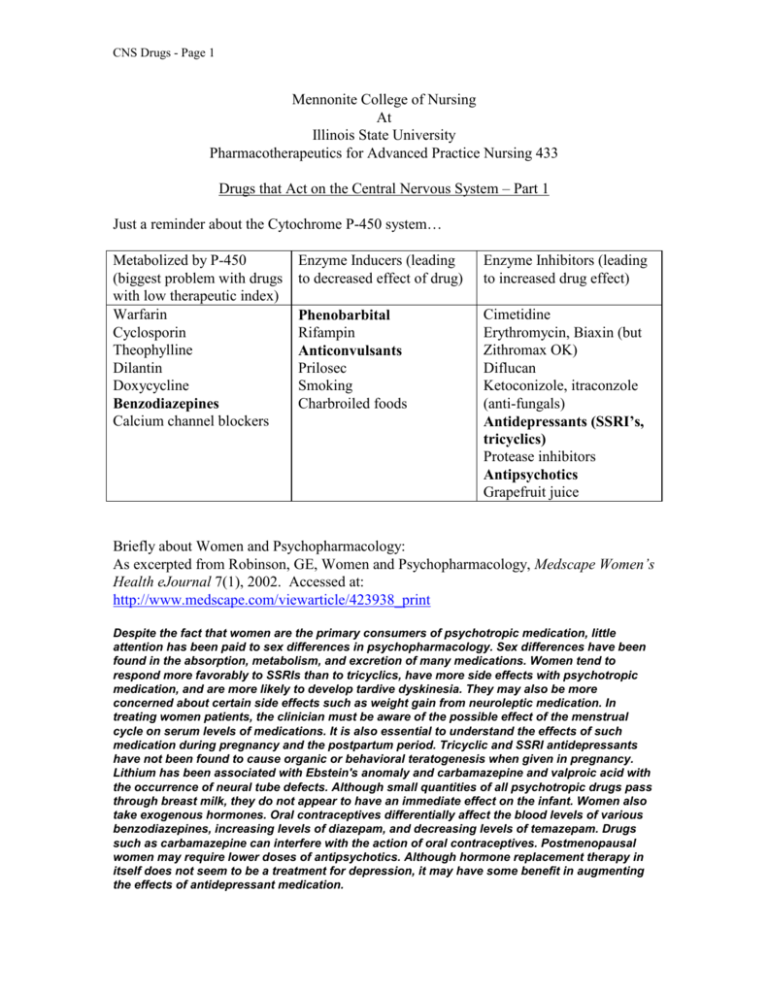
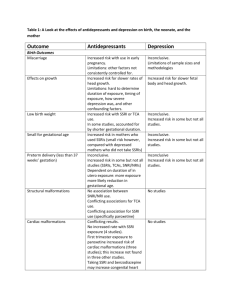
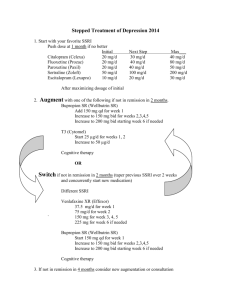
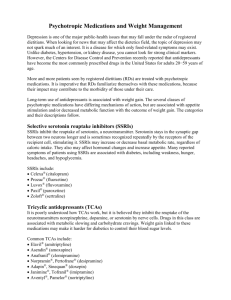
CNS Drugs - Page 1 Mennonite College of Nursing At Illinois State University Pharmacotherapeutics for Advanced Practice Nursing 433 Drugs that Act on the Central Nervous System – Part 1 Just a reminder about the Cytochrome P-450 system… Metabolized by P-450 (biggest problem with drugs with low therapeutic index) Warfarin Cyclosporin Theophylline Dilantin Doxycycline Benzodiazepines Calcium channel blockers Enzyme Inducers (leading to decreased effect of drug) Enzyme Inhibitors (leading to increased drug effect) Phenobarbital Rifampin Anticonvulsants Prilosec Smoking Charbroiled foods Cimetidine Erythromycin, Biaxin (but Zithromax OK) Diflucan Ketoconizole, itraconzole (anti-fungals) Antidepressants (SSRI’s, tricyclics) Protease inhibitors Antipsychotics Grapefruit juice Briefly about Women and Psychopharmacology: As excerpted from Robinson, GE, Women and Psychopharmacology, Medscape Women’s Health eJournal 7(1), 2002. Accessed at: http://www.medscape.com/viewarticle/423938_print Despite the fact that women are the primary consumers of psychotropic medication, little attention has been paid to sex differences in psychopharmacology. Sex differences have been found in the absorption, metabolism, and excretion of many medications. Women tend to respond more favorably to SSRIs than to tricyclics, have more side effects with psychotropic medication, and are more likely to develop tardive dyskinesia. They may also be more concerned about certain side effects such as weight gain from neuroleptic medication. In treating women patients, the clinician must be aware of the possible effect of the menstrual cycle on serum levels of medications. It is also essential to understand the effects of such medication during pregnancy and the postpartum period. Tricyclic and SSRI antidepressants have not been found to cause organic or behavioral teratogenesis when given in pregnancy. Lithium has been associated with Ebstein's anomaly and carbamazepine and valproic acid with the occurrence of neural tube defects. Although small quantities of all psychotropic drugs pass through breast milk, they do not appear to have an immediate effect on the infant. Women also take exogenous hormones. Oral contraceptives differentially affect the blood levels of various benzodiazepines, increasing levels of diazepam, and decreasing levels of temazepam. Drugs such as carbamazepine can interfere with the action of oral contraceptives. Postmenopausal women may require lower doses of antipsychotics. Although hormone replacement therapy in itself does not seem to be a treatment for depression, it may have some benefit in augmenting the effects of antidepressant medication. CNS Drugs - Page 2 Antipsychotic Drugs and Mood Stabilizers Antipsychotic drugs are used to treat: serious mental illness such as the bipolar affective disorder, depressive and druginduced psychoses, schizophrenia, and autism extreme mania certain movement disorders (e.g., Tourette’s syndrome) some medical conditions (nausea and intractable hiccups). The antipsychotics are also referred to as tranquilizers or neuroleptics because they produce a state of tranquility and work on abnormally functioning nerves. Antipsychotics Groups Examples Phenothiazine chlorpromazine (Thorazine) fluphenazine (Prolixin) perphenazine (Trilafon) prochlorperazine (Compazine) thioridazine (Mellaril) trifluoperazine (Stelazine) Thioxanthene thiothixene (Navane) Butyrophenone haloperidol (Haldol) Dihydroindolone molindone (Moban) clozapine (Clozaril) quetiapine (Seroquel) “Atypical Antipsychotics” nd (2 generation) risperidone (Risperdal) olanzapine (Zyprexa) aripiprazole (Abilify) ziprasidone (Geodon) asenapine (Saphris) iloperidone (Fanapt) lurasidone (Latuda) Combination medications (Example) olanzapine (Zyprexa) + fluoxetine (Prozac) = Symbyax (for depression with bipolar; treatment of resistant depression Note: The phenothiazines are associated with a high incidence of anticholinergic side effects because they are closely related to the antihistamines. CNS Drugs - Page 3 Underlying Pathophysiology In mental illness, there are certain areas of the brain where dopamine activity is abnormally increased and others where it is abnormally decreased. Mechanism of Action: The antipsychotics attempt to re-establish dopamine pathways and other neurotransmitter systems and restore normal activity. Many of the antipsychotics are believed to have a common mechanism of action. They are believed to block dopamine receptors in the brain and thus to decrease the dopamine concentration in the CNS. Specifically, the phenothiazines block the receptors that dopamine normally binds to postsynaptically in certain areas of the CNS, such as the limbic system and the basal ganglia. These are the areas associated with emotions, cognitive functioning, and motor functions. This results in a tranquilizing effect in psychotic patients. Both the therapeutic and toxic effects of these agents are the direct result of the dopamine blockade in these areas. Drug Effects The antipsychotics have many effects throughout the body. Besides blocking the dopamine receptors in the CNS, they also block alpha receptors, which results in hypotension and other cardiovascular effects. Many of the adverse effects of these drugs stem from their ability to block histamine receptors: anticholinergic effects. Body System Central nervous system Cardiovascular Gastrointestinal Genitourinary Hematologic Dermatologic Metabolic and endocrine 1 Antipsychotics: Adverse Effects Side/Adverse Effects Sedation, delirium, neuroleptic malignant syndrome1, extrapyramidal movement disorders, dystonia, parkinsonism2, akathisia3, tardive dyskinesia4, seizures Orthostatic hypotension, syncope, dizziness, ECG changes, conduction abnormalities Dry mouth, constipation, paralytic ileus, hepatotoxicity Urinary hesitancy, urinary retention, impaired erection, priapism, ejaculatory problems Leukopenia, agranulocytosis (especially with Clozaril) Photosensitivity, hyperpigmentation, rash, pruritis Galactorrhea (due to blockage of ≥ 72% of D2 receptors → ↑ prolactin release), irregular menses, amenorrhea, decreased libido, increased appetite (weight gain 10# with Zyprexa and Clozaril, 5# with Risperdal, 1# with Geodon), polydipsia, impaired temperature regulation (These symptoms are from increased prolactin levels, resulting from stimulation of hypothalamic-pituitary dopamine system.) NMS = combination of catatonic rigidity, stupor, unstable BP, hyperthermia, profuse sweating, dyspnea, and incontinence. Sometimes occurs as a toxic reaction to potent neuroleptic (antipsychotic) agents in CNS Drugs - Page 4 therapeutic doses. Condition lasts 5-10 days after discontinuationof drug. Mortality rate up to 20%. Treatment: bromocriptine, dantrolene if usual treatment for hyperthermia is ineffective. 2 3 Likelihood of worsening Parkinson’s Disease with Risperdal and Zyprexa than with Seroquel or Clozaril akathisia = inability to sit down because the thought of doing so causes severe anxiety. 4 tardive dyskinesia= a condition of slow, rhythmical, automatic stereotyped movements, either generalized or in single muscle groups. (e.g. facial grimacing, finger movement, jaw swinging, repetitive chewing, tongue thrusting). Usually from prolonged use of phenothiazines or butyrophenones (Haldol). Result of a denervation supersensitivity after prolonged receptor blockade, leading to increased number of postsynaptic dopamine receptors. Must catch early to reverse! (Can also happen with Reglan) Black box warning regarding use of atypical antipsychotics in elderly patients with dementia-related psychosis: NOT approved for behavioral disorders in elderly with dementia increased mortality (heart failure, sudden death, pneumonia increased risk of cerebrovascular adverse events including stroke previously used “off-label” in nursing homes to control “sundowning” (wandering the halls and developing agitation during nighttime hours) Hyperglycemia (severe) and DM → ketoacidosis/coma/death with atypical antipsychotics ? alteration in pancreatic beta cells ? alteration in glucose transporters on hepatic and skeletal muscle ? ↑ BMI CNS Drugs - Page 5 Choosing an Antipsychotic There is very little difference between antipsychotics in the mechanism of actions; therefore selection of an antipsychotic is based primarily on the least undesirable drug side effect and the patient’s type of psychosis. Of the currently available antipsychotic agents, no single drug stands out as being either more or less effective in the treatment of the symptoms of psychosis. It should also be stressed that antipsychotic drug therapy does not provide a cure for mental illness, but is only a way of chemically controlling the symptoms of the illness. 1st Generation Antipsychotic Agents and Their Comparative Properties Drug Name Antipsychotic Potency Phenothiazines Chlorpromazine Low Fluphenzine High Thioxanthenes Thiothixene High Butyrophenones Haloperidol High Dihydroindolone Molindone Intermediate Dibenzoxdiazepine Loxapine Intermediate Sedation Anticholinergic Cardiovascular Extrapyramidal symptoms High Low High Low High Low Low High Low Low Low High Low Low Low High Intermed. Intermediate Intermediate Intermediate Intermed. Intermediate Intermediate Intermediate See: “Comparison of Atypical Antipsychotics” chart for information on 2nd generation antipsychotic agents. Drug Interactions Antipsychotic + antacids decreased absorption of phenothiazines Antipsychotic + antihypertensives may potentiate hypotension Antipsychotic + CNS depressants additive effects increased CNS depression Patient Teaching Take as prescribed…do not double, omit, or skip doses May be several weeks before an improvement is experienced. Phenothiazines may cause drowsiness, dizziness, or fainting, so change positions slowly. Sunscreen is needed when taking phenothiazines…they cause photosensitivity. Avoid taking antacids within 1 hour of a dose of a phenothiazine Notify MD or NP immediately for fever, sore throat, yellow discoloration of the skin, or uncontrollable movements of the tongue when taking a phenothiazine Do not take phenothiazines or haloperidol with alcohol or with any other CNS depressant. CNS Drugs - Page 6 Antidepressants Antidepressants are the pharmacologic treatment of choice for: Depression Dysthymia (chronic depression = >50% of year X 2 years) Schizophrenia Eating disorders Personality disorders Obsessive-compulsive disorder Migraine headache Chronic pain syndrome (often use Elavil @ h.s.) Peptic ulcer disease Sleep disorders Generalized anxiety disorder Diabetic neuropathy Fibromyalgia OTHER USES YOU HAVE HEARD OF? 3 theories regarding cause of depression biogenic amine hypothesis: postulates that depression results from a deficiency of neuronal and synaptic catecholamines (primarily norepinephrine) and mania from an excess of amines at the adrenergic receptor sites in the brain. permissive hypothesis: implicates reduced concentrations of serotonin as the predisposing factor in patients with affective disorders. While depression results from decreases in both the serotonin and catecholamine levels, mania results from increased catecholamine but decreased serotonin levels. dysregulation hypothesis: essentially a reformulation of the biogenic amine hypothesis. It views depression and affective disorders not simply in terms of decreased or increased catecholamine activity but as a failure of the regulation of these systems (new leading theory) Pharmacotherapeutic Treatment The drug categories most commonly used in the treatment of affective disorders are the selective serotonin-reuptake inhibitors (SSRIs), the tricyclic (TCA) and tetracyclic antidepressants, and the monoamine oxidase inhibitors (MAOIs). CNS Drugs - Page 7 Selective serotonin-reuptake inhibitors (SSRIs) considered first-line drugs for treatment of depression o proven efficacy o favorable adverse-effect profile o long-term tolerance o once-daily dosing (** Prozac now available in weekly form) o wide therapeutic index very safe, very few drug-drug or drug-food interactions take approximately the same amount of time (4-6 weeks) to reach maximum clinical effectiveness as it does for the TCAs and MAOIs highly bound to plasma proteins such as albumin have the capacity to inhibit cytochrome P-450 Examples: o Celexa (citalopram) o Luvox (fluvoxamine) o Paxil (paroxetine) o Prozac (fluoxetine) – now available in once/week dosing o Zoloft (sertraline) Generic name Buproprion Maprotiline Trazodone Fluoxetine Sertraline Paroxetine Venlafaxine Citalopram HBr SSRI (and heterocyclic) Side Effects Brand name Sedation Toxicity in Anticholinergic overdose effects Wellbutrin 0 + 0 Ludiomil ++ ++++ ++ Desyrel ++++ + 0 Prozac 0 0 0 Zoloft 0 + + Paxil 0 0 0 Effexor 0 0 0 Celexa 0 0 0 CV Effects 0 ++ + 0 + 0 0 0 SSRI Discontinuation Syndrome – a cluster of symptoms caused by sudden cessation of SSRI use CNS Drugs - Page 8 Tricyclic antidepressants (TCAs): Inhibit the reuptake of norepinephrine and/or serotonin Proven efficacy Considered second-line now that SSRIs are available All are equally effective, but differ in terms of anticholinergic, sedative, and orthostatics side effects. TCA Side Effects Generic Brand name Sedation Toxicity in Anticholinergic CV name overdose effects Effects amitriptyline Elavil ++++ ++++ ++++ ++++ clomipramine Anafranil ++++ ++++ ++++ ++++ desipramine Norpramin + ++++ + ++++ doxepin Sinequan ++++ ++++ +++ +++ imipramine Tofranil +++ ++++ +++ ++++ nortriptyline Pamelor +++ ++++ +++ ++++ trimipramine Surmontil ++++ ++++ ++++ ++++ Disadvantages: Narrow therapeutic index and potential for overdose may be lifethreatening Examples: o Anafranil (clomipramine) o Elavil (amitriptyline) o Norpramin (desipramine) o Pamelor (nortriptyline) o Sinequan (doxepin) o Surmontil (trimipramine) o Tofranil (imipramine) Monoamine oxidase inhibitors (MAOIs): Considered “last” line agents for the treatment of depression that is not responsive to other pharmacologic therapies Useful clinically for the treatment of any type of depression but especially useful for the atypical types such as those characterized by reverse vegetative symptoms (increased sleep and appetite) or by marked panic, phobic, or other anxiety symptoms Inhibit monoamine oxidase, the enzyme that normally metabolizes the neurotransmitters NE and serotonin increased amount of NE and serotonin available to the receptors decreased sx. of depression CNS Drugs - Page 9 Problem: A hypertensive crisis occurs in approximately 8% of the patients on MAOIs. o Occurs if taken with wine and cheese or with Sudafed o It is believed to occur when MAO inactivates GI and liver tyramine, which then enters the bloodstream. (Tyramine is normally degraded by MAO in the intestines). This tyramine displaces presynaptic NE, and this NE in conjunction with the increase in the NE stored and released from nerve terminals through the actions of the MAOIs becomes too much, and hypertension ensues. o Chief complaints in such patients are severe occipital headache, stiff neck, flushing, palpitations, diaphoresis, nausea and vomiting and elevated BP. o Once ingestion occurs, it is considered a medical emergency and immediate treatment should be sought. o Foods and beverages to avoid (high tyramine content) Cheese, especially aged or matured Pickled or smoked fish (herring) Yeast or protein extract Beef or chicken liver Fermented or aged protein foods Beer, red wine, sherry Fava or broad bean pods Spoiled or overripe fruit o Food and beverages to be consumed with some caution (variable tyramine content; some people may be sensitive to these foods) Yogurt and sour cream Chocolate and caffeine-containing beverages Soy sauce, Miso soup Sauerkraut o Medications to avoid Cold medications (containing ephedrine, phenylephrine or phenylpropanolamine) Meperidine (Demerol) Local anesthetics with epinephrine Weight-reducing pills, pep pills, stimulates (amphetamines, methamphetamine, methylphenidate) Methyldopa, quanetidine, reserpine, clonidine Nasal and sinus decongestants Inhalants for asthma Dopamine, metaraminol L-dopa, L-tryptophan Tricylic antidepressants or other MAOIs Cocaine Examples o Marplan (isocarboxazid) o Nardil (phenelzine sulfate) CNS Drugs - Page 10 o Parnate (tranylcypromine) Other antidepressants (heterocyclics) Wellbutrin [alias Zyban] (bupropion) = aminoketone o Dopamine reuptake blocker o Good for use in depressed patients who do not respond to or cannot tolerate SSRI’s o Similar to SSRIs in its energizing effects o Little or no effect on MOA or the neurotransmitters serotonin and NE o No effect on sexual function; good for depressed patients treated with SSRIs who develop sexual dysfunction (impotence and delayed ejaculation in males and anorgasmia in females) Desyrel (trazodone) = triazolopyridine and Serzone (nefazodone) = phenylpiperazine o Tend to be sedative and orthostatics in their chemical effects Effexor (venlafaxine) [also available in XR formulation] o Is a serotonergic noradrenergic reuptake inhibitor (SNRI) o Because it blocks NE as well as serotonin, its adverse effects and drug interactions more closely resemble those of the TCAs o Unlike some newer agents, have been shown to be effective even in severe depression when compared to placebo and the SSRI fluoxetine (Prozac) o Also being used to treat hot flashes (lower dose = Effexor XR 37.5 mg) Remeron (mirtazapine) = tetracyclic o Increases both NE and serotonin o Onset of action and efficacy similar to the TCAs Ludiomil (maprotiline) = tetracyclic o Used in depressive illness associated with dysthymic disorder, manicdepression, and major depressive disorder Choosing a Medication for Depression Some questions to ask: o Has the patient ever had a response to this medication? o Has someone within the family had a response to this type of drug? TCAs are highly lethal when taken as an overdose…many providers are reluctant to prescribe them to severely depressed patients Probably best to stay away from MAOIs: o Using an SSRI concurrently with an MAOI is contraindicated. o These drugs must be separated by a period of 14 days when given in sequence. Failure to observe this “washout period” can result in a serious interaction called serotonin syndrome. Signs/symptoms can include: mental status changes, altered muscle tone, autonomic nervous system instability, and even coma and death CNS Drugs - Page 11 SSRI’s are frequently prescribed in combination with TCAs o A small dose of a sedating TCA at bedtime may help a patient who experiences trouble sleeping because of the SSRI’s stimulating effect. o But exercise caution: SSRI’s may slow the rate at which the TCA is metabolized and increase the risk of TCA toxicity. Observe carefully for signs of possible toxicity such as increased heart rate, hypotension, and arrhythmias and confirm that the dose of TCA is minimal When used appropriately, SSRIs offer safe, effective relief to patients with various emotional disorders o Generally considered more tolerable because they have no effect on cholinergic or adrenergic systems and don’t affect histamine o Less dangerous when taken as an overdose, although they still must be used cautiously in severely depressed patients o However, be aware that SSRIs can cause several sets of opposite, or contradictory effects: one or the other in different patients or even both extremes in the same patient at different times. Such a response may masquerade as the underlying condition being treated: Anxiety and sedation The SSRIs increase serotonin, which can cause sedation, but they can also cause a decrease in dopamine, which frequently causes akathisia (anxiety, tremors, and motor restlessness). You may have trouble identifying the SSRI as the culprit, especially in patients who are also taking antipsychotic medications such as haloperidol [Haldol], which are well known for causing the same problems. Stimulation followed by a “crash” or letdown Warn your patient not to abruptly stop taking an SSRI on her own. Tell her to decrease the dosage gradually under your supervision. Anorexia and weight gain Although some patients report anorexia, and two serotoninrelated drugs indicated specifically for weight loss (fenfluamine [Pondimin] and dexfenfluramine [Redux]) were removed from the market for causing mitral valve disease and pulmonary hypertension, other patients report weight gain (which can lead to the patient refusing to take the med) Warn your patient about the possibility of both adverse reactions. Mood swings Designed to elevated mood, the SSRIs also can cause irritability and occasional mania. Assess for changes in the patient’s mental status. CNS Drugs - Page 12 Also think of other reasons for symptoms: o Attention-deficit disorder high anxiety; if can’t take Ritalin, try imipramine (Tofranil) or Prozac o Check labs and EKG – mitral valve prolapse high level of anxiety o With situational depression (divorce, death, etc.), get good history, check other meds that may cause depression (such as Inderal, Indocin) Keep in mind: 33% of geriatric patients are depressed, especially males. o Look at sedation of proposed med; if patient can’t remember taking meds, DON’T use TCAs. o Note: Prozac is a parent drug that breaks down into norfluoxetine – long 1/2 –life (72 hours), even longer in geriatrics (don’t use in geriatrics) o Zoloft with 15-20 hour ½-life and once daily dosing is good o Best to start at lower dose Remember: the meds are used to return the person to a normal mood; do not usually cause euphoria Don’t give large number of TCAs…will take them all! Use SSRIs instead. o Prozac doesn’t cause suicide…but does give patient enough energy to see how hopeless things are. Counsel, follow-up, keep connected. Sexual side effects: Management strategies o Watchful waiting o Dosage reduction o Drug holiday o Switching antidepressants o Add-on therapy Side Effect Profiles of TCAs, SSRIs, and other agents1 Drug Type Anticholinergic effects amitriptyline doxepin imipramine desipramine nortriptyline venlafaxine nefazodone fluoxetine paroxetine sertraline TCA TCA TCA other other other other SSRI SSRI SSRI +++ ++ ++ + + + + + ++ ++ 1 Orthostatic hypotension +++ +++ +++ ++ ++ + ++ + + + Sedation Agitation/ RestlessNess Headache Migraine Sexual Dysfunction Weight Gain +++ +++ ++ + ++ + ++ + ++ + 0 0 + + + ++ 0 ++ + + + + + + + +++ +++ +++ +++ +++ ++ ++ ++ + + ++ + +++ +++ +++ ++ ++ ++ + + 0 0 + + + +++ = frequently (>20% incidence); ++ = occasionally (10-19% incidence), + = rarely (1-9% incidence); 0 = not reported (0% incidence) Dosing Initiation of therapy CNS Drugs - Page 13 o Start with small dose of TCA and increase every 2-3 days to reach desired dose o SSRIs can be started at full therapeutic dose o See again in 1 week. o Treat for at least 3 weeks…if no change, reconsider dose, diagnosis, medication, need for blood level (for TCAs such as imipramine, nortriptyline) Maintenance therapy o Maintain medication 6-12 months following remission o Taper medication slowly Abrupt discontinuation of anticholinergic antidepressants (TCAs) may result in a withdrawal syndrome (cholinergic rebound) of malaise, muscle aches, chills, cold sweats, nausea, vomiting, abdominal cramps, diarrhea, anxiety, headaches, sleep disturbance, dizziness, motor restlessness, and/or irritability Check what’s going on in the patient’s life before tapering If taking something in AM with coffee, may get lethargic; if take at noc, may not sleep well at first after decreasing dose. Inform patient that they may at times, need to increase dose temporarily during taper Questions/concerns Question of risk of suicidal behavior with SSRIs and TCAs; especially in children and adolescents < 24 years old. (Black Box Warning) Reports suggest a possible interaction between Aricept (donepezil) used for Alzheimer’s patients, and Paxil (paroxeine), an SSRI. Paxil is a potent cytochrome P450 2D6 inhibitor that may slow the metabolism of Aricept, leading to insomnia, confusion, severe diarrhea, etc. Zoloft and Celexa are weaker inhibitors and may be less likely to interact with Aricept. Possible connection between SSRIs and cerebral vasoconstriction and stroke OSA may affect response to antidepressants (2015) Other “Off-Label” Applications of SSRIs include: Premature ejaculation Migraine headache prophylaxis Neurocardiogenic syncope Question: What about interactions between herbal products and SSRIs? Review handouts: Choosing and Switching Antidepressants Combining and Augmenting Antidepressants Treatment-Resistant Depression Discuss: SSRI-induced hyponatremia

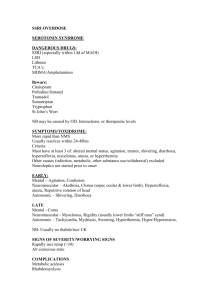
![UW2 - Psychiatric Drugs [2014]](http://s3.studylib.net/store/data/006942877_1-1e1312ddbd9872da620b90364eb238c8-300x300.png)