Slide 1 This Articulate Module addresses the following learning
advertisement

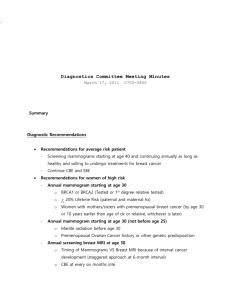
Slide 1 Mammographic Screening • Primary Learning Objective – Discuss the identification and management of individuals at risk for breast cancer • Secondary Learning Objective – Discuss the use and significance of mammography as a tool for breast cancer screening – Discuss issues related to breast cancer screening This Articulate Module addresses the following learning objectives as they pertain to mammographic screening for breast cancer Discuss the use and significance of mammography as a tool for breast cancer screening Discuss issues related to breast cancer screening Answer these two questions. Why is the diagnostic accuracy of this test improved with advancing age? What is the significance of densities and calcifications in mammography? Slide 2 Mammography remains the Gold-Standard, First-Line Breast Imaging Screening Modality • Screening Mammography • Asymptomatic patient • Negative clinical breast exam • Starting at age 40; annually thereafter • Diagnostic Mammography • Symptomatic patient • Suspicious findings on clinical breast exam Title: Gold Standard Slide 3 Mammographic Screening for Breast Cancer • This is a figure from an article in the Huntsville (Alabama) Times. • It clearly demonstrates that the mortality rate from breast cancer has significantly decreased since 1990. • This decrease is due to both the use mammographic screening of women leading to early detection of cancer and improved treatment regimens for women with breast cancer. Slide 4 Warner, E. Breast Cancer Screening New Eng J Med 365, 1025-1032, 2011. • This table demonstrates that the current guidelines for screening mammographies varies with the organizations making the guidelines. • Each guideline agrees that women between the ages of 50 and 69 should be screened; however, whether or not it is every year or every other year varies. • In the 50 to 69 age group, mammography has been reported to reduce breast cancer-related deaths by up to 30%. • For women 70 years or older, the decision about screening should be individualized. Consideration must be given to co-morbidities. • For of women between 40 and 49 years of age , the decision about screening should be individualized based on the patient’s risk factors. •In this age group, mammography has been reported to reduce breast cancer-related deaths by up to 17%. TITLE: Breast Screening Guidelines Slide 5 This illustration, with its associated mammogram, shows the soft tissue structures typical of a normal pre-menopausal breast. The mammogram demonstrates a thin skin margin with no retraction of either the skin or the nipple. The glandular tissue is interspersed with fat and there are regular bands of suspensory ligaments known as Cooper's ligaments. There is no dominant or irregular mass and no evidence of microcalcifications that would indicative of a lesion. TITLE: Breast Structures on Mammograms Slide 6 Breast Density vs. Mammography Findings The sensitivity and specificity of mammograms varies with age, being as high as 95% in post-menopausal women. This variability is directly related to the breast density. Increased breast density of a pre-menopausal breast decreases the ability of the technique to resolve masses and microcalcifications from normal glandular tissue. Both are seen as white areas. This problem is demonstrated by the mammogram on the left taken from a younger woman. It clearly demonstrates the dense white areas typically seen in this patient population, especially in those young women who never have been pregnant. In contrast, the mammogram on the right is from a post-menopausal woman. The fibroadipose tissue that replaces glandular tissue has little density. on mammograms. In younger patients, additional tests such as ultrasonography, nuclear medicine study, and MRI have been useful in resolving breast lesions Slide 7 Mammography Terminology • Analog Mammography (Plain Film Mammography) - x-ray beam directly captured on a film cassette. - outdated and obsolete. • 2D Digital Mammography (Digital Mammography) - x-ray beam captured on digital detector → converts x-ray beam into electronic signal → transferred to a computer → viewed on high- resolution monitor → allows for > image manipulation. - can allow for 30% to 40% decrease in radiation dose. - should be used as Gold-Standard method for screening and diagnostics. Title: Terminology Slide 8 Digital vs. Conventional Mammography These are two mammograms of the same breast. The one on the left is a digital mammogram and the one on the right is a conventional film mammogram. The ability to resolve abnormal lesions from normal breast tissue is best seen with digital mammography. Although more expensive, digital mammography offers a distinct advantage for detecting lesion in women with dense breasts, with a reported sensitivity of 78% vs. 51% for film. Slide 9 Analog versus 2D Digital Mammogram Less Dense Breasts Analog Mammogram 2D Digital Mammogram More Dense Breasts Analog Mammogram 2D Digital Mammography Images 2D Digital Mammogram Slide 10 Mammography Terminology • 3D Digital Mammography (Breast Tomosynthesis) - camera moves over breast, taking multiple-angle images, creating a 3D image, and thus minimizing the impact of overlapping breast tissue. - allows for even > image manipulation. - earlier detection of smaller breast cancers. - be care in ordering! → it may NOT get paid for! Title: 3D Mammography Slide 11 Screening for Breast Cancer Warner, E. Breast Cancer Screening, New J Med 365, 1025-1032, 2011. This figure, from a recent New England Journal of Medicine article on Breast Cancer Screening, demonstrates that in the last 20 years there has been a steady decrease in the incidence of invasive breast cancer. The article states that this is equally due to improved adjuvant therapies and to increasing use of screening mammography. The decision to screen either a particular population or a specific patient for a disease involves weighing benefits against costs. In a cost-benefit assessment screening for breast cancer leads to reduced risk of death resulting in a gain in the number of lifeyears. The article points out that the costs include: financial, risk of radiation, patient inconvenience, and anxiety, the cost of a diagnostic workup in false positive cases and in over diagnosed the case. The ratio of benefit to cost varies with age of the patient. Screening mammography for women 50 to 69 years of age has been universally recommended; in large part due to increased sensitivity of the mammography due to reduced density and possibly due to slower tumor growth. However, there is little costbenefit to screening women beyond 74 years of age, due to life expectancy of 5-10 years. Slide 12 Mammography • Three mammographic abnormalities that are suspicious for cancer include: • Mass • Microcalcifications • Asymmetric Density Mammographic abnormalities suspicious for cancer include: mass, microcalcifications and/or an asymmetric density Screening mammograms are two x-rays are taken of each breast. One is side-toside (medial-lateral) and the other is from top to bottom (cranial - caudal). The breast is pressed between two pieces of plastic just enough so breast tissue can best be seen on the mammogram. This process lasts for a few seconds and is not harmful and minimizes the necessary x-ray dose. The amount of radiation exposure during mammography is about the same as receiving a dental x-ray. It has been estimated that if 10,000 women have yearly mammograms for ten years, the radiation from mammograms will cause one additional breast cancer death. Slide 13 Mammography Average-size lump found by woman practicing occasional breast self-exam (BSE) Average-size lump found by woman practicing regular breast self-exam (BSE) Average-size lump found by first mammogram Average-size lump found by getting regular mammograms Mammography is better at detecting breast lesions that self-exam. Smaller breast lesions are commonly found on routine self-exam as compared to occasional self-exam. Similarly, smaller lesions are detected with routine mammograms as compared to the first mammogram. Overall, mammograms can detect a lesion well before they are clinically evident. This is demonstrated in this mammogram that depicts a small, irregular, mass that was not palpable. Slide 14 Microcalcifications Microcalcifications are seen on mammograms as small white dots. Their presence is often indicative of ductal carcinoma in situ. The diagnosis of ductal carcinoma in situ (DCIS) was rare before the introduction of screening mammography. DCIS accounts for approximately 25% of all cases of breast cancer, with more than 90% of them being detected only by imaging. The risk of cancer is 75% when the microcalcification have a ductal distribution, are fine, and/or have a linear and branching appearance. There a 30% risk of cancer when the calcification are clustered, fine, irregular, and/or granular. (Ref: Adapted from DeMay RM: The Art & Science of Cytopathology, ASCP Press, Chicago, 1996) Slide 15 Mammography Clinical Finding Infiltrating Carcinoma (%) Infiltrating Carcinoma Mean (cm) Nodal Metastases (%) DCIS (%) Microcalcifications on Mammogram 26 0.6 6 71 Density on Mammogram 94 1.1 14 4 Palpable Mass 94 2.4 58 2 After Table 23.1 in Robbins This table correlates the clinical findings with the subsequent pathology. DCIS rarely presents as a palpable mass or as a density on a mammogram. However, it is commonly identified by the presence of microclcifications on a mammogram. In contrast, a mammographic diagnosis of infiltrating carcinoma is primarily made by the presence of a dense lesion rather than by the presence of microcalcifications. Slide 16 BIRADS: Breast Imaging, Reporting, and Data System • Originally designed to utilize standardized descriptors to characterize mammographic findings, including: – Densities/Nodules/Masses/“Asymmetries” – Calcifications – Associated Changes (skin thickening, skin retraction, nipple retraction, architectural distortion, axillary adenopathy) – Categorized findings as BIRADS Category 0-5 – Later adapted for image reporting of Ultrasound and MRI Title: BIRADS Slide 17 BI-RADSTM Mammogram Categories Category Assessment Recommendation 0 Incomplete assessment Additional Imaging Needed 1 Negative Routine screening 2 Benign / stable findings Routine screening 3 Probably benign Short interval follow-up 4 Suspicious abnormality Biopsy recommended / urged 5 Highly suggestive of malignancy Appropriate action to be taken This table is for your own information. What is your interpretation and which category would you put it in? Slide 18 Breast Ultrasound • Best performed in a targeted-fashion to a particular area of interest in the breast and not in a screening fashion to the entire breast. • Breast modality to distinguish cystic versus solid lesions. • Best modality to characterize solid lesions. • Useful in detecting and defining intraductal lesions in the evaluation of suspicious nipple discharge. Title: Breast Ultrasound Slide 19 Breast MRI • Should be utilized selectively in appropriate selected patients. • Two categories for utilization: – Potential Diagnostic Utilities – Potential Screening Utilities T Slide 20 Breast MRI - Diagnostic Tool • Evaluating a patient with a “difficult” clinical breast exam and dense breasts on mammography. • Characterizing breast anatomy in the absence of a mammographic or ultrasound lesion (BI-RADS 2 breast imaging) in a patient with a clinically suspicious finding on clinical breast exam. • Evaluating clinical concerns in a breast with an augmentation / implant. • Evaluating clinical concerns a mastectomy patient with implant reconstruction. • Evaluating clinical concerns a mastectomy patient with autologous tissue flap reconstruction. • Ruling out multicentric ipsilateral disease or concurrent contralateral disease in a patient with a newly diagnosed breast cancer. • Monitoring tumor response to preoperative neoadjuvant systemic chemotherapy in a patient with newly diagnosed breast cancer. Slide 21 Breast MRI - Screening Tool • Annual screening of any patient with a documented hereditary breast cancer gene mutation. YES! YES! YES! • ???Annual screening of a patient with a strong family history of breast cancer but who has had documented negative genetic testing??? CONTROVERSIAL? • ???Annual screening of a patient with a strong family history of breast cancer but who has declined genetic testing??? CONTROVERSIAL? • ???Annual screening of a patient with a personal history of breast cancer??? CONTROVERSIAL? • ???Annual screening of a patient with a personal history of radiation therapy to the chest for another type of cancer, such as Hodgkin’s disease, when treated between the ages of 10 and 30 years old??? CONTROVERSIAL? Slide 22 Recap of Key Points • Mammography is best in post-menopausal women because of reduced density. – It identifies abnormal microcalcifications in most ductal carcinomas in-situ that can’t be identified on physical exam – It is capable of identifying smaller lesions that would go undetected by palpation. • Use ultrasound in a targeted manner not as a screening method • MRI uses include: – Hereditary breast cancer gene mutation – Patients with implants – R/O multicentric disease – Monitoring chemo effects before surgery Mammography is best in done on post-menopausal women because of reduce density. Abnormal microcalcifications identify most ductal carcinomas in-situ that can’t be identified on physical exam Mammography is capable of identifying smaller lesions that go undetected by palpation.