Instructions Performance Measures Residential
advertisement

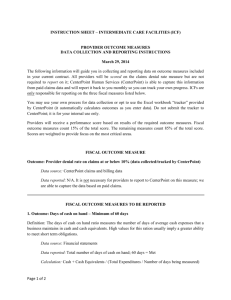
INSTRUCTION SHEET – MASTER- RESIDENTIAL ONLY PROVIDER PERFORMANCE MEASURES DATA COLLECTION AND REPORTING INSTRUCTIONS January 28, 2015 The following information will guide you in collecting and reporting data on performance measures included in your current contract. All providers will be scored on the claims denial rate measure but are not required to report on it; CenterPoint Human Services (CenterPoint) is able to capture this information from paid claims data and will report it back to you monthly so you can track your own progress. Providers who deliver mental health, intellectual/developmental disabilities and substance abuse services (all disability service types) are responsible for reporting on the measures listed below. Please indicate only numbers on the reporting template. Do not add symbols (eg %). Please copy and save your reporting template to allow you to enter the following quarters’ data on the same template for submission. If your template becomes corrupted for any reason, you may access a clean copy on the CenterPoint website at www. cphs.org. See below for instructions if you have not served any CenterPoint clients in a given quarter. You may use your own process for data collection or opt to use the Excel workbook “tracker” provided by CenterPoint (it automatically calculates outcomes as you enter data). Do not submit the tracker to CenterPoint; it is for your internal use only. If you use the “tracker” to calculate quarterly data, move new client referrals with less than 14 calendar days available for service to the next reporting quarter. Providers will receive a performance score based on results of the required outcome measures. Fiscal outcome measures count 15% of the total score. The remaining measures count 85% of the total score. Scores are weighted to provide focus on the most critical areas. Timely reporting will be appreciated and expected (see table at the end of the document). Failure to submit reports on or before the expected due date may result in a Plan of Correction. A pattern of failure to submit in a timely manner will have contract implications. EXCLUDED from reporting: Hospitals, ICFs, PRTFs, and MDs (prescribers) in solo or MD (prescriber) group practices only; Solo and group practices that serve 24 or fewer clients. When the 25th client is served (defined as a billable event), the reporting template must be completed and submitted quarterly for the remainder of the contract year. If a solo or group practice serves 24 or less clients an email attesting to that fact must be submitted quarterly to ProviderOutcomes@cphs.org. Agencies that serve 3 or fewer clients. When the 4th client is served (defined as a billable event), the reporting template must be completed and submitted quarterly for the remainder of the contract year. If an agency serves 3 or fewer clients for the quarter an email attesting to that fact must be submitted quarterly to ProviderOutcomes@cphs.org . Page 1 of 4 FISCAL PERFORMANCE MEASURE 1. Outcome: Provider denial rate on claims at or below 10% (data collected/tracked by CenterPoint) Data source: CenterPoint claims and billing data Data reported: N/A. It is not necessary for providers to report to CenterPoint on this measure; we are able to capture the data based on paid claims. Open Access MH/SA/I-DD providers are responsible for reporting on the following performance measures found in your current contract with CenterPoint. Please use the reporting template provided and report according to the schedule located at the end of this document. FISCAL PERFORMANCE MEASURES 2. Outcome: Days of cash on hand – Minimum of 60 days Definition: The days of cash on hand ratio measures the number of days of average cash expenses that a business maintains in cash and cash equivalents. High values for this ratio usually imply a greater ability to meet short term obligations. Data source: Financial statements Data reported: Total number of days of cash on hand; 60 days = Met Calculation: Cash + Cash Equivalents / (Total Expenditures / Number of days being measured) 2a. Outcome: Current ratio of 1.0- ONLY reported if Days of Cash on Hand is less than 60 days (indicate na on the reporting template if #1 is met) Definition: The current ratio is used to measure liquidity. The value of the current ratio measures the number of dollars held in current assets per each dollar of current liabilities. High values for this imply good ability to pay short–term obligations. Data source: Financial statements Data reported: Ratio; 1.0 =Met Calculation: Current assets / Current liabilities 2b. Outcome: Long-term debt to net assets ratio – Maximum ratio of 2.5:1- ONLY reported if Days of Cash on Hand is less than 60 days (indicate na on the reporting template if #1 is met) Definition: The long term debt to net assets ratio is used to measure the company’s assets that are financed with loans and financial obligations lasting more than one year. The ratio provides a general measure of the financial position of the company, including its ability to meet financial requirements for Page 2 of 4 outstanding loans. A year-over-year decrease in this metric would suggest the company is progressively becoming less dependent on debt to grow their business. Data source: Financial statements Data reported: Ratio; 2.5:1 = Met Calculation: Long term debt / Total Net Assets CLINICAL PERFORMANCE MEASURE 3. Outcome: Integration of Care – Annual Primary Care Physician (PCP) visit. NOTE: Reporting required for Medicaid-funded clients only; all disability groups; limited to clients receiving Enhanced Benefits. Definition: Evidence of at least one visit to a PCP within the previous 12 months at the time of review for Medicaid clients as defined above. Data source: Provider peer review forms Data reported: Percent of Medicaid-funded client charts in compliance; 70% = Met Calculation: Number of charts indicating annual PCP visit / Total number of charts reviewed (expressed as a percentage) REPORTING SCHEDULE Note: Current CenterPoint Medicaid contract addendums for Calendar Year 15 (CY15) are in effect for January 1, 2015- June 30, 2015 as DMA will be moving to the Fiscal Year effective July 1, 2015. Current CenterPoint State funded contracts for Fiscal Year 15 (FY15) are based on a fiscal year that began on July 1, 2014 and are in effect until June 30, 2015. CenterPoint intends to continue reporting requirements on the current performance measures in contracts offered for FY16 (July 1, 2015- June 30, 2016). At that time two additional reporting periods will be added to extend reporting through the life of the contract. To avoid confusion between CY and FY quarters as DMA transitions to the fiscal reporting year, we have identified Reporting Periods that mimic the traditional quarters in both a calendar year and a fiscal year. Submit the reporting template to CenterPoint at ProviderOutcomes@cphs.org according to the following schedule. To simplify data collection, CenterPoint provided a “tracker” that automatically calculates outcomes as you enter the data. You may use this option or your own process. Please remember that it is not required that you use the tracker and it is not necessary to submit it to CenterPoint. You only need to submit the reporting template type that applies to your practice. Page 3 of 4 Reporting Period Reporting Period 1 Reporting Period 2 Reporting Period 3 Reporting Period 4 Page 4 of 4 DUE DATE April 30, 2015 July 30, 2015 October 30, 2015 January 30, 2016 REPORTING PERIOD January - March 2015 April – June 2015 July – September 2015 October – December 2015