pulmonary embolism, Atrial Fibrillation, Acute pain - VGH-care
advertisement

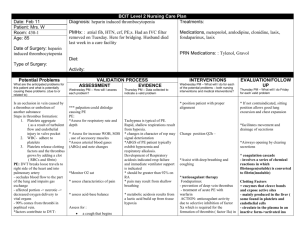
Date: Feb 18 Patient: Mrs S Room: 200 bed2 Age: 83 BCIT Level 2 Nursing Care Plan Diagnosis: Choleycytitis Treatments: PMHx: CAD, AFib, COPD, PE, HTN, Anemia< SOB, OSTEo, Date of Surgery: Diet: DAT Type of Surgery: did not do surgery Activity: AAT Medications: Lasix, Digoxin, Nitroglycerin patch, Oxycodone Simvastin, Vit. D, calcium carbonate, PRN Medications: Acetaminophen Potential Problems What are the anticipated problems for this patient and what is potentially causing these problems. (due to or related to) Pulmonary Embolism ( History of - so greater risk) s an occlusion in vein caused by a thrombus or embolism of another substance Steps in thrombus formation: 1. Platelets aggregate ( as a result of turbulent flow and endothelial injury in valve pocket 2. WBC- adhere to platelets 3. Platelets release clotting factors and the thrombus grows by adding a clot ( RBCs and fibrin) PE: DVT breaks loose travels to right side of the heart and into pulmonary artery - occludes blood flow to the part of the lung and impairs gas exchange - affected portion -> necrotic -> VALIDATION PROCESS ASSESSMENT EVIDENCE Wednesday PM – How will I assess each problem? *** palpation could dislodge causing PE PE: *Assess for respiratory rate and depth * Assess for increase WOB, SOB , use of accessory muscles *Assess arterial blood gases (ABGs) and note changes Thursday PM – Data collected to indicate a valid problem INTERVENTIONS Wednesday PM – What will I do for each of the potential problems – both nursing interventions and medical interventions? * position patient with proper alignment Change position Q2h – EVALUATION/FOLLOW UP Thursday PM – What will I do Friday for each valid problem * If not contraindicated, sitting position allows good lung excursion and chest expansion *facilitates movement and drainage of secretions *Airways opening by clearing secretions * assess characteristics of pain *Assist with deep breathing and coughing *. Mobilize pt Q3h to prevent blood stasis. * coagulation cascade - involves a series of chemical reactions in which fibrinogen(soluble) is converted to fibrin(insoluble) * assess acid-base balance *Anticoagulant therapy Assess for : Warfarin -Treatment of thromboembolic complications associated with atrial fibrillation Clotting Factors = enzymes that cleave bonds and expose active sites - mainly produced in the liver ( some found in platelets and endothelial cells - circulate in the plasma in an inactive form->activated ina *Monitor O2 sat a cough that begins suddenly, and may produce bloody sputum (mucus): significant amounts of decreased oxygen delivery to vital organs - 90% comes from thrombi in popliteal vein. *factors contribute to DVT: hypercoagulbility of the blood, venous wall damage, stasis of blood flow visible blood or lightly blood streaked sputum (phlegm) sudden onset of shortness of breath at rest or with exertion splinting of ribs with breathing (for example, bending over or holding the chest) fainting dizziness sweating anxiety rapid breathing rapid heart rate chest pain: Diagnostic Tests for PE: Electrocardiogram ultrasound examination of the legs, or a lung perfusion scan -treatment of venous thrombosis, pulmonary embolism Action: Coumarin anticoagulants inhibit synthesis of prothrombin - interfering with action of vitamin K Intrinsic Pathway (contact activation pathway) - occurs more slowly -All components are within the blood -initiated when factor XII (clotting factor) is activated by the contact of blood with subendothelia collagen damage or an artificial surface Thrombin is the final activated clotting factor and converts fibrinogen to fibrin *CT angiogram is a type of computed tomography (CT) scan. It is fast, noninvasive, and fairly accurate, particularly for large clots. In this test, contrast material is injected into a vein. The contrast material travels to the lungs, and a CT scanner generates images of blood in the arteries to determine if a pulmonary embolism is blocking blood flow. A CT angiogram is the imaging test most often used to diagnose pulmonary embolism Diagnostic tests Spiral CT angiogram: pulmonary nodules are well evaluated because breathing misrepresentations are eliminated. - continuously obtains images as the patient is passed through the gantry. V/Q Scan: Is used to identify defects in blood perfusion of the lung in patients with suspected PE. Perfusion Scan: 1.Patient is given a peripheral IV injection of radionuclidetagged MAA (macroaggregated albumin) 2. While the patient lies in the appropriate position, a gamma ray detector is passed over the fixed sequence - the activated clotting factor acts on the next precursor - because a single activated product can act on many precursors-> amplification - must reach a certain concentration before clotting can occur _ there are two pathways that lead to the activation of clotting factor X and the synthesis of prothrombinase ( factor Xa) ! Extrinsic pathway ( tissue pathway) - primary pathway -occurs rapidly ( within seconds of trauma) -initiated by tissue factor ( extrinsic to the blood) (– protein that is the primary cellular initiator of blood coagulation) - on the surface of subendothelial cells ( fibroblasts) - released by damage endothelial cells patient and records radionuclide uptake on Polaroid or x-ray film. 3. patient is placed in a supine, prone, and various lateral positions, which allows for anterior, posterior and lateral and oblique views Ventilation Scan 1.Pt. breathes through a closedsystem mask with a mouth piece. A radionuclide tracer is then administered into the system. Ultra sound X-Ray Atrial Fibrillation (ACTUAL) - is the result of disorganized current flow within the atria. Fibrillation interrupts the normal contraction of the atria. - is characterized by rapid, chaotic atrial depolarization from a reentrant pathway. At extremely rapid rates the entire atrium may not be able to recover from one depolarization wave before the next one begins, resulting in mechanical and electrical disorganization of the atria without effective atrial contraction. - The AV node is bombarded with more impulses than it can conduct so a rapid ventricular response comparable to the atrial rate cannot occur. - Because of the atrial disorganization the “atrial kick” is lost -> decreases cardiac out put by 30%. - With increasing ventricular rates allowing less filling time, Ausculate the heart for tachycardia ( greater than 100beats) and bradycardia ( less than 60 beats) * assess for signs of reduced cardiac output: rapid, slow, or weak pulse, hypotension, dizziness, syncope, SOB, restlessness, chest pain, fatigue * Stimulants increase the automaticity of the heart which can precipitate dysrhythmias 1. Deliver heart medications. pt. is on Warfarin 2. Maintain fluid balance. Input = output. If input increases and output is decreased pulmonary or peripheral edema can occur. 3. Allow environment for physical and emotional rest as stress can increase cardiac demands. This also reduces oxygen demands. cardiac output declines even further and may result in dyspnea, angina pectoris, heart failure, and shock -may be a pulse difference between apical and radial pulses. * blood pools in the atria because of lack of adequate contraction of atrial appendages. Pooling blood is prone to clot, forming a mural thrombus, which increases the risk of cerebral and peripheral vascular emboli> COPD ( ACTUAL) COPD - Inflammation and fibrosis of the bronchial wall, hypertrophy of the submucosal glands and hypersecretion of mucus and loss of alveolar tissue and elastic lung fibers. Inflammation and fibrosis of the bronchial wall, along with excess mucus secretion, obstruct airflow and cause, mismatching of ventilation and perfusion. Destruction of alveolar tissue decreases the surface area for gas exchange, and the loss of elastic fibers impairs the expiratory flow rate, increasing air trapping, and predisposes to airway collapse. 1.Ausculate lungs after coughing as needed to note and document significant change in breath sounds: *Decreased or absent lung sounds -indicate presence of mucous plug or other major airway obstruction *presence of fine crackle-may indicate cardiac involvement or secretion trapping *wheezing -indicates increasing airway resistance *course sounds -indicate presence of fluid along larger airways Position head of bed in upright and high Fowler’s position - favors lung expansion; the diaphragm is pushed downward. If patient is bedridden, turning from side to side at least Q2h promotes better aeration of all lung lobes 2. Assess for change in resp rate and depth -rate and rhythm changes are early signs of resp compromise * Teach patient deep breathing techniques 3Assess characteristics of or changes in secretions: consistency, quantity and color 4. Note any color in changes in lips, buccal mucosa, nail beds - cyanosis occurs when at least 5g of *Assist patient with coughing, deep breathing, and splinting - improves productivity of cough *Administer low- flow oxygen therapy as indicated (e.g., 3L/min by nasal cannula) . If insufficient , switch to highflow o2 apparatus (Venturia mask) for more accurate oxygen delivery Consult respiratory Encourages a more complete exhalation COPD patients who chronically retain carbon dioxide depend on “hypoxic drive” as their stimulus to breathe. When applying oxygen, close monitoring is imperative to prevent unsafe increases in the patient Pa O2 which could result in apnea. - reduce airway resistance, treat infection, and facilitate secretion haemoglobin are desaturated 5. Assess hydration status: skin turgor, mucous membranes, tongue -Airway clearance is impaired with inadequate hydration and subsequent secretion thickening. 6. Monitor pulse oxygen saturation and ABGs -hypoxia can result from increased pulmonary secretions and resp. fatigue Acute Pain (due to gallbladder stone, c/o pain in abdominal area) Acute pain is frequently associated with anxiety and hyperactivity of the sympathetic nervous system Pain has sensory and emotional components Gate Control TheoryMelzack The interplay among these connections determines when painful stimuli go to the brain: 1. When no input comes in, the inhibitory neuron prevents the projection neuron from sending signals to the brain (gate is closed). 2. Normal somatosensory input happens when there is more large-fiber stimulation 1. assess pt pain behaviour. (grimacing, guarding, wincing, avoiding movement) 2. assess pt pain level on a scale of 1-10 & LOTARP pain Q1hr 3. assess pt’s last dose of analgesic and frequency 4. Monitor autonomic responses (diaphoresis, HR, RR, change in BP, nausea, pallor, pupil dilation) 5. assess pt knowledge or preference for the array of pain relief strategies available 6. evaluate pt response to meds/theraputic interventions therapist for chest physiotherapy and nebulizer treatment *Administered bronchodilators, expectorants, anti-inflammatory (steroids) and antibiotics, as ordered * Incentive Spirometer – improves deep breathing and prevents atelectasis 10x hour *Pace activities for patient with reduced energy 1. Help pt into a comfortable position. Provide pt with a heating pad or warm blanket to help alleviate pain. 2. administer appropriate analgesic if pt is do for next dose. (Refer to pops list and WHO pain scale). Also educate pt to report pain, especially if it is not controlled. 3. evaluate the pt’s response to pain and medication and medications or therapies aimed at relieving pain. (Q1hr) 4. provide rest periods to facilitate comfort, sleep and relaxation. Can also provide distractions such as conversation, tv, 5.Assess and document the intensity of the pain and each new report of pain at regular intervals (systematic ongoing assessment and documentation provide the direction for pain treatment plans and adjustments based removal (or only large-fiber stimulation). Both the inhibitory neuron and the projection neuron are stimulated, but the inhibitory neuron prevents the projection neuron from sending signals to the brain (gate is closed). 3. Nociception (pain reception) happens when there is more small-fiber stimulation or only small-fiber stimulation. This inactivates the inhibitory neuron, and the projection neuron sends signals to the brain informing it of pain (gate is open). on the pt’s response 1.Epidural Need to explain 2. PCA Need to explain Discharge planning How is she coping? What type of support does she have? Does she have a supportive friends that can come and help with household chores, making meals when she is at home? Does she have someone to take her to all the appointments Does she have visitors? Does she have a thermometer at home? Where does she live? Whom does she live with? Meals on Wheels (Vancouver) 604-732-7638 Community nurseVancouver -604-263-7377