Plantar Fascia - WordPress.com
advertisement

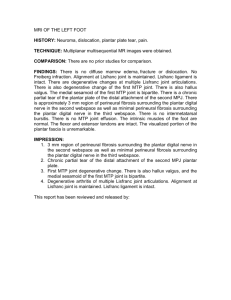
Dear Caitlin, I write to you a junior trainee sonographer, at the beginning of my musculoskeltal training. I work rurally without the support of any sonographers in my practice and I do not have an on-site radiologist. I hope you don’t mind, but Anna Graves has passed on your details because she thought you might be able to assist me with the basic ultrasound prinicples and understandings before undertaking a plantar fascia assessment. No worries if you cant, but I look forward to your response. Thank-you kindly, Jonathon Chidley Jonathon Chidley Dear Jonathon, Thank-you for your email. I would be happy to assist you in your studies. Performing an ultrasound examination of the plantar fascia is a relatively straight-forward examination. As will all sonographic assessments, the priority is to understand the anatomy. The plantar fascia is a flattened tendinous aponeurosis spanning from the calcaneal tubercle, or posterior postion of the calcaneous and the proximal phalanges of the toes. The structure is largely composed of longitudinal collagen fibres into three structural divisions, the medial, central and lateral component. A continuous fascial connection exists between the plantar fascia and the Achilles tendon and the paratendon, which decreases with age (Stecco et al, 2013 and Arherakis et al, 2015). The plantar fascia role involves supports the longitudinal arch of the foot, aiding proprioception and peripheral motor coordination (Stecco et al, 2013). The following is a diagram to aid your visual understanding. To undertake a plantar fascia assessment, position the pateint prone, either with the foot flexed and toes on the bed or with the feet hanging off the edge of the bed. Place the probe over the midline heel with the probe in a longitidinal position. It is important to understand normal sonographic appearances of the plantar fascia. The following image demonstrates the medial plantar fascia insertion at the calcaneous of the right foot. The fascia will present as a flat, homogenous fibrillar structure with no particular vascualrity generally detectable. Below is an image I have taken of a normal plantar fascia insertion measuring 32mm at the widest point. There is no significant bulging, loss of fibrillar patern, it is homogenous (as apposed to being heterogenous and hypechoic) and therefore oresents normally on US. Be certain the assess both the medial and lateral origin aspects and follow them down in longitudinal and transverse to assess the structure entirely. Refer to the diagram above to recall how large the area is you will need to assess. With a good understanding of the normal anatomy of the plantar fascia, you will begin to notice any anamolies. Plantar fasciitis is an inflammatory condition that affects up to 10% of the general population during their lifetime, typically during middle age. Pain typically presents tenderness on dorsiflexion on the medial heel, usually in the morning or at the beginning of activity. Risk factors ineclude biomechanical factors, obesitiy, excess stnadning, ealking and running in inappropriate footwear. Ultrasound provides an ideal modality to assess the plantar fascia demonsrating thickness and heterogenicity in inflammed fascias (Mohseni-Bandpei et al, 2014). The following image is an image I have taken over the semester of a thickened plantar fascia. The fascia measures 7mm and appears hypoechoic and bulges in comparison to a normal plantar fascia (refer back to the image above). Plantar fibromatosis, also known as Ledderhose disease, is a hyperproloferative disease of the plantar fascia resulting in nodule formations. Presentation is typically slow growing palpable nodules which demonstrate pain and swelling after extended exercise, with a predilation to men. Bilateral disease exists in 25% of cases. (Veith et al, 2013). The next image I have included for you is an image I have recently taken of a patient who presented with a area of focal pain and tenderess. The clinical area revealed a focal bulging of the plantar fascia, without any significant increase in vasculairty. A recent ultrasound study has shown that 73% of participants with clinical plantar pain demonstrates plantar fascitis and 51% demonstrates a plantar fibroma. Keep in mind that the two pathologies, therefore, are not mutually exclusive, with 36% of patients demonstrated to have both plantar fibromatosis with platar fascitis (Argerakis et al, 2015). Though less common, it is likely you may also encounter plantar fascia tears or calcaneal spurs in patients presenting with plantar pain. You will also need to understand how to assist in a cortisone injection of the plantar fascia. It will your responsibility to source the equipment for the radiologist, explain the proceedure to the patient, gain informed consent and position the patient appropriately. Position the patient prone with their feet resting off the edge of the bed. Increase the height of the bed and move the ultrasound machine closer towards the patients feet and rotate the screen to allow easy injection and visualisation of the screen for the radiologist. Injections are typically composed of 1mL of 4mg/mL dexamethasone sodium phosphate after an initial 2% lignocaine (McMillan et al, 2012). You will need to have 2*2mL syringes, a drawing up needle, an injection needle (length based on the patient’s individual injection depth), lignocaine, marcaine, cortisone, cholorhexidine, a sterile dressing pack and sterile gloves readily available. Each radiologist has a slightly different protocol for injections, but typically be prepared to sterilise the area with chlorohexidine as the radiologist prepares the injections. My radiologists will inject the initial anaesthatic without US guidance, injection from the posterior heel, with the needle parallell to the sole of the foot. You will simply need to locate the needle once it is in place. The aim in to inject the needle slightly superficial to the plantar fascia origin allowing it to tract distally. Given the ultrasound beam is typically perpendicular to the needle, it is usually visualised well but can be improved with a significant decrease in frequency, appropriate focus and gain. Here is an annotated image of an injection I have performed recently. I hope my correspondance will assist you in you ultrasound assessments. Please, Jonathon, feel free to contact me with any concerns. It has been a pleasure to help. Thank you, CaitGardiner Caitlin Gardiner References Arherakis NG, Positano RG, Positano CJ et al, 2015. Ultrasound Diagnosis and Evaluation of Plantar Heel Pain. JAPMA; 105(2): 135-140. Mohseni-Bandpei MA, Nakhaee M, Mousavi ME, Shakourirad A et al, 2014. Application of Ultrasound in the Assessment of Plantar Fascia in Patients with Plantar Fasciitis: A systemic review. Ultrasound in Medicine and Biology; 40(8): 1737-1754. McMillan AM, Landorf KB, Gilheany et al, 2012. Ultrasound Guided corticosteroid injection for plantar fasciitis randomised controlled trial. BMJ; 344 Stecco C, Corradin M, Macchi V, Morra A, Porzionato A, Biz C and De Caro R, 2013. Plantar fascia anatomy and its relationship with Achilles tendon and paratendon. Journal of Anatomy; 223(6): 665-676. Veith NT, Tschernig T, Histing T and Madry H, 2013. Plantar Fibromatosis- Topical Review. FAI; 34(12): 1742-1746.