Diagnostic Musculoskeletal Ultrasound
advertisement
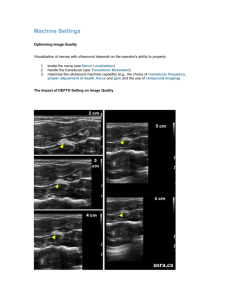
Marc Lederman, DPM West Hartford Podiatry Associates March 29, 2014 Disclosures Consultant- Bioventus Consultant- Bellevue Pharmacy Executive Director, CPMA Outline of the Presentation 1. Basics, Physics and Terminology 2. Indications 3. Scanning of different anatomical sites and structures 4. Office Integration 5. Billing and Coding Diagnostic Ultrasound gives you an increased ability to better evaluate and understand soft tissue pathology and how that relates to the functional mechanics of the structure being evaluated. What is UltraSonography and How Does it Work? Ultrasound is a longitudinal pressure wave. It is generated in a device called the transducer, which is the ultrasound probe. This is unique in that sound waves are used instead of ionizing radiation. The transducer is placed on the skin surface with a coupling gel (ultrasound gel) and the positioning of the probe determines what structure, depth and view is imaged. Physics of Ultrasound The ultrasound unit sends an electrical signal to the transducer which results in a sound wave. The electrical signal is converted to ultrasonic energy and back again as the signal is reflected off the different tissue densities. As the ultrasonic pulse reflects off the various tissues, it is converted back to an electrical impulse which is captured again by the transducer and an image is produced which is viewed on the monitor. Imaged Produced The individual body tissue offers a natural resistance to the transmission of the ultrasonic pulse. This is directly proportional to the average density of the tissue. Various shades of grey, bright signals and those devoid of any contrast become the displayed images. Image Quality An important consideration is the frequency of the transducer used for MSK imaging. For Podiatric use, the frequency of the probe is between 12-18 MHz The higher the frequency, the higher the resolution, but this is at the expense of the depth. Therefore, a higher frequency is used for a superficial tendon or joint, 18MHz, and a lower frequency for the evaluation of a plantar fascia attachment, 14MHz. Equipment MyLab®One by Esaote A Linear transducer with a small head Portable on a stand or desk top Touch screen monitor MyLab is a registered trademark of Esaote S.p.A. Ultrasound Terminology Near Field- These are structures that appear in the upper half of the monitor. Far Field- Scanned structures and their position is near the bottom half of the monitor. Echogenic- These structures generate an echo and are highly reflective, bright or white on the screen, like bone. Anechoic- These do not generate an echo and are seen as darker or black on the monitor, like a ganglion. Terminology Continued Structure patterns which can be Homogeneous (uniform) or Heterogeneous (irregular). Hyperechoic- brighter echo like scar tissue or the surface of bone. Hypoechoic- less echo, like an area of inflammation or a partial tendon tear. Axial resolution- ability to distinguish two objects when they lie directly over each other. Horizontal resolution- two objects side by side and the same distance from the transducer. Terminology Continued Anisotropic- having different optical properties in different directions. The ultrasound image will change as the angle of the transducer changes. Perpendicular to the structure is preferred and as the structure changes direction, for example the posterior tibial tendon, the image will change if you do not keep the probe perpendicular. You can therefore lose signal when evaluating a structure and mistake the image for pathology. Indications for Podiatric Ultrasound Use Plantar Fascia tears or inflammation Plantar Fibroma Achilles Tendon Pathology; tendonosis, tendonitis, partial or complete ruptures, insertional exostosis Cystic masses like a ganglion, inclusion cysts Retrocalcaneal Bursitis Morton's Neuroma Bursitis Ligament strains or tears Indications Continued Ankle sprains and ligament pathology Foreign bodies Stress fractures Ultrasound guided injections Scanning Technique The terms long and short axis are used to describe how one positions the transducer to the patient’s foot and ankle. You must sit comfortably and have the monitor positioned in such a manner to make viewing the screen natural and easy. Use the heel of your hand and fingers to stabilize the transducer to the skin surface and move slowly over the structure to best appreciate the anatomy. Ultrasound Technique When evaluating a structure, you rock the transducer slowly heel to toe, lengthwise with the linear probe and slowly sweep the probe adjusting to stay perpendicular to the structure being studied. On the monitor, you pick the depth, the frequency, the focal point and adjust the grey zone for the best image. The physical exam will guide you to the location and focal point of the ultrasound study. In USER tab, press preset button to select: Very Superficial, Superficial, Medium, or Deep. 17 Adjust TGC—touching in this area will make adjustment available Adjust Overall Gain To adjust the Focus, simply touch the screen in the area on which you want to focus. You will see the focus indicator (the yellow carat on the right-hand side) move up and down. 18 Touch Freeze to freeze the image. Touch Image to acquire a still image of the frame present on screen at time it is touched. Color will activate Color Doppler. PwrD will activate Power Doppler. B+B will allow a split screen and toggle between right or left. M-Mode will activate an M-Mode line, touching a second time will activate M-Mode. 19 Adjust Overall Gain Color (if Doppler license is present) will display Color Doppler imaging to enable blood flow visualization. To relocate the color ROI (region of interest) box, simply touch the screen in the desired area. 20 The benefit of Color Doppler This represents blood flow or inflammation The red color is moving towards the transducer The blue is moving away from the transducer We can see this in tumors, tendon or nerve pathology where typically we would not expect to see blood flow. In the inflammatory phase of a tendon injury (10-14 days post injury) the findings would suggest neovascularization. Buttons can be easily programed to do image and documentary functions (Freeze, Image, Power Doppler etc.) MyLabOne Knobology MyLibrary, on board educational tool. Touch Accept to continue to anatomic segments and views. 23 Very Important Have a landmark. Know the anatomy of the part being examined. Use motion imaging and still images in the evaluation. Some People are Easier to Scan Than Others. Water content, the patient’s BMI, fat content and variations in normal anatomy will effect the scan. Making adjustments in the gain, the depth and the probe frequency can help offset the variables. Using Ultrasound to Evaluate Common Foot and Ankle Pathology The Plantar Fascia The Achilles Tendon Morton’s Neuroma Ganglions Ankle Ligaments First MTP Joint Pathology Ultrasound Guided Injections Long Axis view of the plantar fascia Short axis view of the plantar fascia Normal plantar fascia Abnormal thickness of the fascia Normal Fascial Attachment Abnormal Attachment Long axis view of the Achilles Tendon Normal Achilles Tendon Insertion Achilles Tendon with Calcification Same Long Axis with more depth Tendon Pathology in Motion Short axis view of the Achilles Tendon Short Axis Achilles Tendon Morton’s Neuroma, 3rd innerspace Dynamic Ultrasound Exam Ganglion Angioleimyoma Sub first MTP Using Color Doppler Radiograph of Gout First IPJ Gout First IPJ, Hallux Gout over IPJ with proximal extension of inflammation Gouty Tophi in the IPJ First MTPJ Pain with Motion First MTP intra-capsular lesion Same lesion with joint motion Plantar Fibromatosis Synovial Cyst with Neuroma Evaluation of a Ganglion Aspiration under Ultrasound Ganglion Partial Aspiration of a Ganglion Office Integration Charting: Clinical Presentation including history and c/c Type of machine, settings and patient positioning A description of the scanning technique/location Findings and Impressions When appropriate, include acoustical impedance, measurements, and homogeneous or heterogeneous tissue or mass descriptions. You can template the structure of the note and make it specific for the type of tissue or anatomy being studied. Just like MRI’s or CT scans, the body of the note can be repetitive from patient to patient, so long as you properly and completely report your specific findings and impressions regarding each patient scanned. Daily Use in the Office You do not need a specific room to perform the exams. Have the staff help by imputing the patient demographics and setting up the room. You will be slow in the beginning so put a full appointment aside for basic exams and re-schedule for guided injections . You can integrate the exam images into your EMR. Billing and Coding CPT code 76881- Complete exam used for Joint evaluations. CPT code 76882- imaging soft tissue structures like tendons, fascia and lesions. CPT code 76942- used for guided injections, biopsies and aspirations. Conclusion With the proper training and time Diagnostic Ultrasound can be well integrated into a busy Podiatric Office. Can obtain a specific diagnosis and isolate particular structures. Can observe a structure or joint under motion to better understand the pathology or function. The patient is informed and part of the exam. Conclusion The technique allows for the use of additional modalities such as PRP and cortisone injections. Generate an additional source of practice income. Avoids out of office testing and a quicker diagnosis. References Ronald Adler PhD, MD et al. Atlas of Foot and Ankle Sonography, Lippincott, Williams and Wilkins 2004 Jacobson, Jon MD, Fundamentals of Musculoskeletal Ultrasound, second edition, Saunders, 2013 Ultrasonographic Evaluation in Plantar Fasciitis, Journal of Foot and Ankle Surgery, Karaday, Nuri, MD, et al. p442-446 Chih-Kuang, Chen, MD et al. Ultrasound Diagnosis and treatment of plantar fascia, American J of phys med. Rehabil. 91:182-184 Wen-Cheng, Tsai Ultrasound evaluation of the Plantar Fascia, Scand J Rheumatol 2000; 29:255-259
![Jiye Jin-2014[1].3.17](http://s2.studylib.net/store/data/005485437_1-38483f116d2f44a767f9ba4fa894c894-300x300.png)