Plantar Fasciitis Algorithm
advertisement
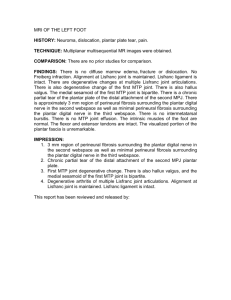
Katie Barta Michael DeDonder Brenda Hozie Shannon Lynch Kelci McFarland • Plantar fascia • The plantar fascia is a thick band of connective tissue that supports the arches of the foot. It absorbs the ground reaction forces from weight-bearing activities and distributes them throughout the foot. http://www.aidmyplantar.com/foot-anatomy.php • Definition and Mechanism of Injury • Plantar fasciitis is a condition which causes heel pain. Individuals can acquire such pain from a sudden increase in activity, an increase in standing or being in a weight-bearing position for a long period of time, and/or a change in the biomechanics of the foot and subtalar joint. The diagnosis is usually related to more of a repetitive stress to the plantar fascia rather than an acute trauma. This repetitive stress causes an inflammatory process of the fascia leading to pain during ambulation. http://www.heel-that-pain.com/plantar_fascia/ • Biomechanics/Anatomy • • • • • • • • Rearfoot valgus High plantar arches Increased longitudinal medial plantar arches Ankle equinous – leads to pronation of rearfoot and midfoot; straining of the plantar fascia Forefoot varus – leads to pronation of rearfoot and midfoot; straining of the plantar fascia Rearfoot varus – leads to rapid and excessive pronation of STJ right after initial contact; causes strain on plantar fascia Pes Plano Valgus– leads to rapid and excessive pronation of STJ right after initial contact; causes strain on plantar fascia Pes cavus – leads to each foot striking ground more often; limited pronation of STJ limits pes cavus from absorbing GRF • Age (over 40 yrs) • Injury to the plantar fascia from cumulative stress overload • Occupational • • • • • teachers construction workers cooks nursing military • Sports Related • repetitive strain injury (long distance runners) • beginning new running program • rapid increase in length or levels of activity • Obese (BMI greater than 30) • Sedentary • Limited ankle dorsiflexion or decreased calf muscle flexibility • Flat foot (over pronation) • High plantar arches • Poor biomechanics (previously discussed) or structural abnormalities • Improper shoe selection • How do these reflect which path we choose to take? • When considering different causes of heel pain activity level, type of activity and in some cases age will be a factor. Biomechanics can also be a contributing factor to plantar fasciitis, but should also be considered for other diagnoses such as Achilles tendinopathy, bursitis, or nerve pathologies. • Pain on medial undersurface of the heel • Pain in the morning when stepping out of bed and taking first steps of the day • Stabbing pain • Sensation of tightness and/or tenderness along arch of foot • Pain with prolonged standing • Pain when standing up after sitting for a long period of time • Pain after an intense weight-bearing activity such as running • Pain when climbing stairs • Pain when walking barefoot or in shoes with poor support • Symptoms may decrease during the day as the body warms up, but will worsen again at the end of the day due to extended walking. • Plantar fasciitis does not have a specific test that can rule in the diagnosis. The following list, along with signs, symptoms, and mechanism of injury, can lead to the conclusion of plantar fasciitis diagnosis versus some other diagnosis. • Positive tender to palpation • Positive dorsiflexion, toe extension PROM reproduction of pain • Potential change in navicular drop test – biomechanical change • Negative radiographs • Negative Morton’s neuroma test • Negative Thomas test • Negative neural test • Limited ankle ROM • Abnormal foot 4 points of normalcy Heel Pain Yes Neural Pain Not Plantar fasciitis Nerve Entrapment Neuroma No Not plantar fasciitis Sharp ache Location of pain Calcaneal Not plantar fasciitis Bursitis Plantar Midfoot Not plantar fasciitis Tarsal tunnel Peroneal teninopathy Achilles tendinopathy Severs No increased pain with weight-bearing Increased pain with weight-bearing Cancer – Refer out Not plantar fasciitis Pain at initial weight-bearing Plantar fasciitis: Including pain with passive toe extension, limited ankle dorsiflexion Pain with prolonged weight-bearing Calcaneal stress fracture • The best way to diagnosis plantar fasciitis is to determine the location and type of pain the patient is experiencing. Once those are considered the algorithm can be used to rule in/out plantar fasciitis. Remember, however, to use all of the subjective and objective findings to aid in the diagnosis of plantar fasciitis versus other foot/ankle pathologies. • • • • • • • • • Aldridge, T. (2004). Diagnosing Heel Pain in Adults Title, 70(2). American Physical Therapy Association. (2013). Physical Therapist's Guide to Plantar Fasciitis. Retrieved April 2013, from Move Forward: http://www.moveforwardpt.com/SymptomsConditionsDetail.aspx?cid=a2395ee9-08bb-47cc-9edc1943e2fdbf2e Cole, C., Seto, C., & Gazewood, J. (2005). Plantar fasciitis: evidence-based review of diagnosis and therapy. American family physician, 72(11), 2237–42. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16342847 Dubin, J. (2007). Evidence Based Treatment for Plantar Fasciitis. Retrieved April 2013, from http://www.dubinchiro.com/plantar.pdf Dutton, M. (2004). Orthopaedic: Examination, evaluation, & intervention. New York, NY: McGraw-Hill. Mayo Clinic. (2013). Risk Factors. Retrieved April 2013, from Plantar Fasciitis: http://www.mayoclinic.com/health/plantar-fasciitis/DS00508/DSECTION=risk-factors Orchard, J. (2012). Plantar fasciitis. Bmj, 345(oct10 1), e6603–e6603. doi:10.1136/bmj.e6603 Ribeiro, A. P., Trombini-Souza, F., Tessutti, V., Rodrigues Lima, F., Sacco, I. D. C. N., & João, S. M. A. (2011). Rearfoot alignment and medial longitudinal arch configurations of runners with symptoms and histories of plantar fasciitis. Clinics, 66(6), 1027–1033. doi:10.1590/S1807-59322011000600018 Tu, P., & Bytomski, J. R. (2011). Diagnosis of heel pain. American family physician, 84(8), 909–16. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22712192