Child and Youth Mental Health
advertisement

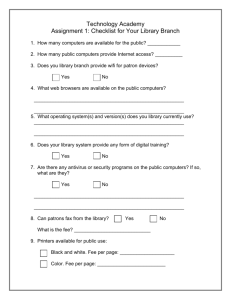
Child and Youth Mental Health Fees Information Revision: June 2015 Table of Contents Overview ............................................................................................................. 5 Community-Based Mental Health Initiative ............................................................... 5 Community GP Mental Health Incentive ................................................................... 5 Eligibility.............................................................................................................. 5 Point of Care Urine Drug Screening Fee ................................................................... 6 MSP Fee Codes.....................................................................................................7 Mental Health Fee Codes ....................................................................................... 7 Explanation of Mental Health Planning Fee ............................................................... 7 Explanation of Mental Health Management Fees ........................................................ 9 Group Medical Visits ............................................................................................. 9 Unattached Complex/High-Needs Patient Attachment Fee ........................................ 11 Non Face-to-face Management Fees ..................................................................... 11 Family Physician Conferencing Fees ...................................................................... 12 Specialist Telephone Advice Fees ......................................................................... 15 Case Study ........................................................................................................ 17 Intentionally left blank Overview Health Community-Based Health Initiative In January 2008, GPSC launched a community based mental health initiative to support GPs providing mental management as part of their comprehensive practice. This mental health initiative links with the Community Patient Conferencing fees to support collaborative care. This community-based mental health initiative includes compensation for creating a mental health plan that will act as a conduit to additional counseling fees over and above the MSP counseling fees. The planning fee and resulting access to an increased number of billable GP management/counseling fees is intended to recognize the significant investment in time and skill such patients require in general practice. These fees are also intended to acknowledge the vital role of the GP in supporting patients with mental illness and addictions to remain safely in their home community. Community GP Mental Health Incentive The GPSC Mental Health incentive was designed to help to compensate the family physician or practice accepting the role of most responsible family physician for the longitudinal coordinated care of that patient for that calendar year who: Have an Axis I diagnosis confirmed by DSM IV criteria; Presents with severity and acuity levels causing sufficient interference in activities of daily living that developing a management plan for the rest of the year would be appropriate. Eligibility Patients are community based, living in their home, in assisted living facilities, or in group homes. Payable only to the most responsible family physician for the majority of the patient’s longitudinal general practice care; Not payable to physicians who have been paid for any specialty consultation fee in the previous 12 months. Not payable to physicians who are employed by or who are under contract and whose duties would otherwise include provision of this care. Not payable to physicians working under salary, service contract, or sessional arrangements and whose duties would otherwise include provision of this care. Point of Care Urine Drug Screening If there is concern that substance use/abuse may be playing a role, the “Point of Care” Urine Drug Screening kit may now be used in any patient where a physician feels it is medically appropriate to screen for one of the 7 substances on the approved sevenanalyte panel that is available. In addition to these seven analytes, urine samples should also be checked for specific gravity and creatinine using the adulteration strips. This is a simple way of establishing the integrity of the sample and is included under the fee codes P15040. POC testing also requires regular quality control monitoring, and supplies for this are included with the panel kits. POC testing of urine in BC will include testing for the following seven substances: amphetamines benzodiazepines cocaine metabolites methadone metabolites opioids oxycodone buprenorphine Note that testing for methadone metabolites is more reliable than testing for methadone alone, as a patient can easily tamper with a urine sample by adding a few drops of methadone. Additional substances can be tested beyond the routine screen when clinically appropriate. These substances need to be clearly identified on the requisition. It is important to remember that not all drugs of abuse are detected with the POC panel. Some drugs (for example, certain benzodiazepines and synthetic opioids), will only be detected with more sophisticated laboratory techniques such as gas chromatography. If more thorough investigation by gas chromatography or mass spectrometry is necessary, this should be indicated on the laboratory requisition. MSP Fee Codes Relevant to Mental Health List of Fee Codes – – – – – Counseling Fees – age appropriate up to 4 MSP counseling fees per year: Code 00120; 2 – 49 years of age Code 15320; 50 – 59 years of age Code 16120; 60 – 69 years of age Code 17120; 70 – 79 years of age Code 18120; 80 + years of age Point of Care Urine Drug Screening Fee – Code 15040 Mental Health Care Fees List of Fee Codes Mental Health Planning Fee – Code G14043 – – – – – Mental Health Management Fee – age appropriate counseling equivalents available after successful billing of Mental Health Planning fee G14043 and once all 4 MSP counseling fees used up: Code G14044; 2 – 49 years of age Code G14045; 50 – 59 years of age Code G14046; 60 – 69 years of age Code G14047; 70 – 79 years of age Code G14048; 80 + years of age Telephone/E-mail Follow Up Fee – Code 14079 Attachment Patient Telephone – Code 14076 Explanation of Mental Health Planning Fee G14043 The Mental Health Planning Fee (14043) requires the GP to conduct a comprehensive review of the patient’s chart/history, assessment of the patient’s current psychosocial symptoms/issues by means of psychiatric history, mental status examination, and use of appropriate validated assessment tools, with confirmation of diagnosis through DSM IV diagnostic criteria. The Mental Health Planning Fee requires a 30 minute face-to-face visit with the patient, with or without the patient’s medical representative. If the visit has been longer than 30 minutes, the office visit may be billed in addition to 14043. If the visit has been 50 minutes or longer, and the extra time fulfills the preamble requirement for counseling, the office counseling visit may be billed in addition to 14043. Effective July 1, 2015, start and end time of the total time for the Mental Health Planning Visit and any additional visit/counseling fee must be submitted to MSP and must be documented in the patient chart. From these activities (review, assessment, planning and documentation) a Mental Health Plan for that patient will be developed that documents in the patient’s chart: - that there has been a detailed review of the patient’s chart/history and current therapies; - the patient’s mental health status and provisional diagnosis by means of psychiatric history and mental state examination; - the use of and results of validated assessment tools. GPSC strongly recommends that these evaluative tools, as clinically indicated, be kept in the patient’s chart for immediate accessibility for subsequent review. Assessment tools such as the following are recommended, but other assessment tools that allow risk monitoring and progress of treatment are acceptable: i) KADS6 Kutcher adolescent depression scale ii) TEFA Teen functional assessment tool iii) GAD-7 for anxiety; iv) Suicide Risk Assessment; such as TASR-A for adolescents - DSM-IV Axis 1 confirmatory diagnostic criteria; - a summary of the condition and a specific plan for that patient’s care; - an outline of expected outcomes; - outlined linkages with other health care professionals (including Community Mental Health Resources and Psychiatrists) as indicated and/or available) who will be involved in the patient’s care, and their expected roles; - an appropriate time frame for re-evaluation of the Mental Health Plan; - that the developed plan has been communicated verbally or in writing to the patient and/or the patient’s Medical Representative, and to other health professionals as indicated. Care begins with the planning process – Sit down with patient; review their conditions and plan for their management – Include self-management goal-setting: important part of developing an effective mental health plan annually – Planning process can include patient questionnaires sent home to complete and bring to the planning visit for review. Effective July 1, 2015, start and end times for the total planning time must be submitted and documented in chart. Fee requires: 30 min face-to-face visit (G14043); If visit is longer than: 30 minutes: – For: 31 min –: 49 min sessions, bill G14043 plus 00100 – For: 50 min or more, bill G14043 plus 00120 1 Payable once per calendar year per patient Payable in addition to a visit/counseling fee billed same day under time conditions above – – – Document the patient’s mental health status diagnosis Psychiatric history Mental state examination (per DSM IV diagnostic criteria) Confirmation of Axis 1 Diagnosis as per criteria; a requirement for patients to be eligible for the GP Mental Health Planning Fee2 1 provided all other MSP pre-amble requirements are met 2 Not intended for patients with self-limiting or transient mental health symptoms eg. brief situational adjustment reaction, normal grief, life transitions etc., for whom a plan for longer term mental health care is not necessary. Mental Health Planning Fee (continued) Use of and results of validated assessment tools such as: i) KADS6 Kutcher adolescent depression scale ii) TEFA Teen functional assessment tool iii) GAD-7 for anxiety iv) Suicide Risk Assessment (such as TASR-A for adolescents)(2) Explanation of Mental Health Management Fee G14044 Once the Mental Health Planning fee (G14043) has successfully been billed, the FP has access to 4 additional counseling equivalent GP Mental Health management fees over the balance of that calendar year once all 4 MSP counseling fees used Minimum time required is 20 minutes; Effective July 1, 2015 both start and end times for counseling (MSP and GPSC fees) must be submitted with fee and documented in chart. Age appropriate code: G14044 for 2–49 years of age All preamble requirements for counseling in effect: “Counseling is defined as the discussion with the patient, caregiver, spouse or relative about a medical condition which is recognized as difficult by the medical profession or over which the patient is having significant emotional distress. Counseling to be claimed as such must not be delegated and must last at least 20 minutes. Counseling is not to be claimed for advice that is a normal component of any visit or as a substitute for the usual patient examination fee, whether or not the visit is prolonged.” GP Group Medical Visits Provides 1:1 patient care in a group setting. Effective way of leveraging existing resources while simultaneously improving quality of care and health outcomes, increasing patient access to care and reducing costs. Can offer patients an additional health care choice, provide them support from other patients and improve the patient-physician interaction. Physicians benefit by reducing the need to repeat the same information many times and free up time for other patients. Appropriate patient privacy is always maintained and typically these benefits result in improved satisfaction for both patients and physicians. All members of the group are receiving medically required treatment (i.e. each member of the group is a patient – family members of a single patient do not constitute a GMV). Not intended for activities related to attempting to persuade a patient to alter diet or other lifestyle behavioural patterns other than in the context of the individual medical condition. Unlike previous billing of 00100, all of which counted toward the HVLIP cap of 50 patients per day, the new fee scale does not. Fee is billable per patient, per half hour or greater portion thereof. If more than one physician (GP &/or Specialist) is present, split the group evenly and each physician bills for those patients. GP Group Medical Visit Fee Codes Fee Code # Patients Fee Code # Patients 13763 3 13773 13 13764 4 13774 14 13765 5 13775 15 13766 6 13776 16 13767 7 13777 17 13768 8 13778 18 13769 9 13779 19 13770 10 13780 20 13771 11 13781 > 20 13772 12 Specialist Group Medical Visit Fee Codes Fee Code # Patients Fee Code # Patients G78763 3 G78773 13 G78764 4 G78774 14 G78765 5 G78775 15 G78766 6 G78776 16 G78767 7 G78777 17 G78768 8 G78778 18 G78769 9 G78779 19 G78770 10 G78780 20 G78771 11 G78781 > 20 G78772 12 Unattached Complex/High-Needs Patient Attachment Fee G14074 Unattached patients (including children and youth) with Mental Health &/or Substance use issues are one of the target populations for the Unattached Complex/High Needs Patient Attachment fee. It is intended to compensate for the often time consuming and intensive process of integrating a new patient with higher needs into a family physician’s practice. Once a Complex/High-needs patient has been accepted into the longitudinal, the other GPSC incentives become available (eg. Mental Health Planning) if the patient meets the eligibility requirements. Fee value is $200 paid in addition to the visit fee, and covers the initial meetings, organization of a medical record, and organization and enactment of appropriate Clinical Action Plan(s) as discussed with the patient. Billing this incentive requires the accepting family physician to collate and review the relevant patient record to date and to meet with the patient to discuss this information and determine what supports will be needed to provide for the patient’s ongoing medical needs, taking into account his/her personal goals of care. Payable only for unattached new patients who have been referred from Acute Care: ER and Admitted, Mental Health/Substance Use Workers/Clinics, Home and Community Care, BC Cancer Agency or Regional Centres, Public Health Colleagues, Ministry of Children and Family Development (MCFD)/local social services professionals, Local Division. Patients who are already attached to a family physician in the same community are not eligible (i.e. Not for transfers between FPs unless moving to a new community or in the case of a sudden departure from practice of the previous FP). Non-face-to-face Management Fees Explanation of GP Telephone/e-mail Follow Up G14079 Telephone or email follow-up fee (G14079). The telephone/e-mail follow-up fee will be available to use up to 5 times in per calendar year following the successful billing of the mental health planning fee (G14043) within the previous 18 months. The 18 month “time clock” will be reset with each revision/rebilling of the planning fee. Service provided by GP or delegated to MOA/Office Nurse under direction of GP. Requires 2-way communication (e-mail from MD and from patient) Applicable to either physician-initiated or patient-initiated follow up For clinical follow-up management by GP who created and billed for the GP Mental Health Planning Fee (G14043) Not for prescription refills/appointment reminders Chart must record the name of the person who communicated with the patient or patient’s medical representative, and capture the elements of care discussed Explanation of Attachment Patient Telephone Fee G14076 Attachment Patient Telephone Fee (G14076) is available for the FP is participating in the GPSC Attachment Initiative who has submitted the Attachment Participation code G14070 (G14071 for Locums) in the same calendar year prior to billing for telephone visits. FPs participating in the “GP for Me” Initiative have access to 1500 telephone calls per family physician per calendar year. Best to use up all 5 Telephone/e-mail fees (G14079) before utilize Attachment Patient Telephone fee (G14076) due to limited number per FP per calendar year. May be delegated to College Certified Allied Health Professional who is working in the FP practice, supporting FP-patient relationship. Eg. RN, NP. MOA is NOT included. Family Physician Conferencing Fees With the introduction of the GPSC Attachment Initiative, billing for community conferences with allied health professionals (AHP) is dependent up whether the FP is participating in the Attachment Initiative or not. Both conference codes are payable when coordination of care and two-way collaborative conferencing with at least one other health care providers is required (e.g., specialists, psychologists or counselors, home care or specialty care nurses, physiotherapists, occupational therapists, social workers, specialists in medicine or psychiatry), as well as with the patient and possibly family members, in order to develop the clinical action plan (and any revisions as clinically indicated over time). The Attachment Patient Conferencing fee is for the communication of a coordinated clinical action plan developed (or revised) for the care of any patient for whom the Attachment participating FP is the Community MRP, regardless of the patient’s location or of the underlying medical condition. The General Practice Community Patient Conferencing fee is for the communication of a coordinated clinical action plan developed (or revised) for the care of community-based patients (living at home, group home or “assisted living”) with more complex needs, including patients with mental health conditions. The maximum units of conferencing that can be billed are different between the 2 Conferencing codes. The Attachment Patient Conference code (14077) has replaced the original 3 conference codes (14015, 14016 & 14017), is more flexible regarding patient condition, location and has removed the need for in person participation when the patient is in a facility. Both have a maximum of 2 units per patient billable on any one calendar day. The same basic GPSC billing rules apply to both sets of Conferencing fees: Not billable for GPs on contract (salary/service/sessional) where care provided under this incentive is already compensated Compensates GP when conferencing for the creation of a coordinated clinical action plan for patients living in the community, with more complex needs, including patients with mental health conditions Not billable for simple advice about patients IN COMMUNITY CARE when initiated by the community care worker (Bill 13005) Involving allied health professionals in the self-management process is billable under community patient conferencing fee (e.g. Bounce Back) Once goals and plan determined, communicating these with the allied health professionals involved in the patient care is appropriate; this may improve patient ability of attaining their goals May be billed in addition to MSP office visit or other GPSC fees Attachment Patient Conferencing Fee G14077 Billable by FP participating in the GP for Me (Attachment) Initiative and who have submitted Attachment Participation Code 14070 in same calendar year prior to accessing the Attachment Patient Conference fees (G14071 if locum) Billable for conferencing with Allied Care Professionals as defined by GPSC for its initiatives, regarding any patient for whom the Attachment Participating FP is the Community MRP. Billable for patients in any location (Community, Hospital, other facility) Conferencing with at least one other health professional (includes specialists and GPs with specialty training) – by telephone or in person Payable in units of $40.00 for each 15 minute unit or major portion thereof, for a total of 18 units per calendar year, max of 2 units on any one calendar day Community Patient Conferencing Fee G14016 Billable by FPs who are not participating in the GP for Me (Attachment) Initiative. Conferencing with at least one other allied care professional as defined by GPSC for its initiatives (includes specialists and GPs with specialty training) – by telephone or in person (14016) Community patients: community based, living in their home, in assisted living facilities, or in group homes Payable in units of $40.00 for each 15 minute unit or major portion thereof, for a total of 6 units per calendar year, max of 2 units on any one calendar day General Practice Urgent Telephone Conference with a Specialist (or GP with Specialty Training) Fee G14018 Conferencing on an urgent basis (within 2 hours of request for a telephone conference) with a specialist or GP with specialty training by telephone followed by the creation, documentation, and implementation of a clinical action plan for the care of patients with acute needs; i.e. requiring attention within the next 24 hours and communication of that plan to the patient or patient's representative. Available for any patient for whom the FP is the community MRP Not dependent of FP participating in GP for Me (Attachment) Initiative Payable to the GP who initiates a two-way telephone communication (including other forms of electronic verbal communication) with a specialist or GP with specialty training regarding the urgent assessment and management of a patient but without the responding physician seeing the patient. Conversation must take place within two hours of the GP’s request and must be physician to physician. Not payable for written communication (i.e. fax, letter, email). Payable at a flat rate of $40 for a maximum of 6 (six) services per patient, per practitioner per calendar year. Limited to one claim per patient per physician per day. Advice about a Patient in Community Care 13005 Value = 50% of 00100 This fee may be claimed for advice by telephone or fax about a patient in community care in response to an enquiry initiated by an allied healthcare worker specifically assigned to the care of the patient. Community Care comprises Residential, Intermediate and Extended care and includes patients receiving Home Nursing care, Home support or Palliative care at home. CYMH patients living in their family home and supported by the Community Mental Health program, living in a supported group home or located in A & D treatment centre would be eligible. Patients located in acute care hospital are not eligible. Allied health care workers are defined for MSP purposes as: home care coordinators, nurses, (registered, licensed practical, public health, and psychiatric), psychologists, mental health workers, physiotherapists, occupational therapists, respiratory therapists, social workers, ambulance paramedics, and pharmacists (not intended for prescription renewal). This fee may not be claimed in addition to visits or other services provided on the same day by the same physician for the same patient. This fee may be billed to a maximum of one per patient per physician per day. This fee may not be claimed by physicians who are on third party call to a facility or applicable to calls about doctor of the day patients to a physician who is on-call for doctor of the day at the time of the request for advice. Similarly the fee does not cover advice provided by doctors who are on-site, on-duty in an emergency department, who are being paid at the time on a sessional basis, or who are working at the time as hospitalists. Specialist/GP with Specialty Training Telephone Advice Fees Developed to compensate specialists for giving telephone advice to other physicians and to patients. GPSC funds the mirror fees for those GPs providing specialty services. For the purpose of these telephone advice fee items the GPSC has defined a General Practitioner (GP) with specialty training as: “A GP who has specialty training and who provides services in that specialty area through a Health Authority supported or approved program”. Telephone advice must be related to the field in which the GP has received specialty training. Conversation must be clinical in nature. Not to be used to book an appointment, arrange for transfer of care that occurs within 24 hours, arrange for laboratory or diagnostic investigations, inform the referring physician of results of diagnostic investigations arrange a hospital bed, expedited consultations or arrange for a transfer of care. CMPA recommendations from liability perspective: Before giving telephone advice, be satisfied you have obtained enough information to be confident the advice is appropriate. With the passage of time, medical information you have received or advice you have given over the telephone may be difficult or impossible to recall. Whether you have given the advice to other professional colleagues or directly to patients, appropriate documentation of the discussion will be important should your advice ever be called into question. Consider having a system in place to make it easier to document your advice. Specialist Telephone advice fees with other Physician (GP or Specialist): G10001 (G14021) – Physician to Physician Rapid Telephone Advice This fee is to be used when another physician (GP or Specialist) requires immediate advice. Specialists (GPs with Specialty Training) can bill this item when they provide telephone advice to the initiating physician within two hours. G10002 (G14022) – Specialist (GP with Specialty Training) Patient Management Advice This fee is to be used when a Specialist (GP with Specialty Training) providing telephone advice to the initiating provider (Specialist, General Practitioner or Allied Care Provider) within seven days of an initiating call. Specialist Telephone Follow-up with Patient G10003 (G14023) – Specialist (GP with Specialty Training) Scheduled Telephone Patient Follow-up Fee This fee is for Specialists (GP with Specialty Training) to have scheduled followup phone visits with their own patients in situations that do not require a faceto-face visit. The telephone follow-up must be pre-scheduled with the patient in order to bill this fee. This fee applies to two-way direct telephone communication (including other forms of electronic verbal communication) between the Specialist and patient, or a patient’s representative. Not payable for written communication (i.e. fax, letter, e-mail). Case Study Anna S, a 15 year old girl, has been referred to you by her school counselor. The counselor’s assessment form indicates that Anna’s attendance has slipped, and while the counselor originally attributed her quieter than normal mood to a recent breakup with her boyfriend, there has been no improvement after 6-7 weeks. Anna has told the counselor that she is feeling depressed and is always tired. Anna arrives in your office early in January. You talk with her and she states that she is not sleeping well and finds most things an effort. You have her complete the 6-item KADS and her score is 10. Her TASR-A review does not identify any urgent issues pertaining to suicide or safety. In taking her family history, you note that there is a family history of depression with her mother requiring treatment 7 years ago. Her father has used drugs in the past, but no longer lives in the family home. Using supportive, non-judgmental problem solving, you encourage and prescribe exercise, regulated eating and positive social activities. She agrees to try to take walks or some other form of mild exercise, initially. She also will try to talk to her mother about what she is feeling. In all, you spend 20 minutes counseling her about her situation and the probable diagnosis of depression. You schedule another visit with her for a few days later, when you can meet with her for a longer visit. You have blocked 30 minutes for Anna’s Mental Health Planning visit. Anna’s score on the KADS today is 14 and she is having more frequent thoughts about dying but no suicidal ideas or plans. The TASR-A is unchanged from the previous visit. You discuss treatment options and Anna agrees to begin counseling with a mental health clinician. You schedule a “check in” for 3 days after this visit using either text message or email and arrange to see her again, in person, next week. You follow up with her via email 3 days later. Service Counseling#1 Diagnostic Code: 311 Service MH Plan (30 min) Fee Code 14043 # Units Diagnostic Code: 311 Service MH Email F/U #1 Diagnostic Code: 311 When you see Anna again 1 week later for a 25 minute counseling session, she says she feels increasingly depressed, is still having sleep difficulties, fatigue and has no interest in school and social activities. Her KADS score is still 14 and she endorses a number of items on the TASRA (including occasional thoughts that life is not worth living) that make you concerned about her wellbeing but you do not think that she is actively suicidal. Fee Code # Units 00120 (MSP #1) 311 Fee Code 14079 # Units Using the TeFA as a guide you establish that she has developed significant functional problems in a variety of domains. She is not psychotic and denies any other drug use. You review with her concerns about her possibly becoming depressed and arrange to see her for a longer mental health assessment in three days’ time. You impress on her the need to call if things get worse and to discuss the situation with her mother. Before that next scheduled visit, you contact the school counselor to update him on Anna’s situation and compare notes. After a 25 minute phone conference, with the counselor, your opinion that Anna is developing a major depressive episode is reinforced. When you next see Anna, her KADS score is 14 and there is no difference in your assessment of her suicide risk using the TASR-A guideline. Given the history you have obtained to date and the persistently elevated KADS scores, you apply the 11 item KADS as the baseline symptom evaluation. You use the PST framework to guide your discussions with her and discuss medication with her, addresses her concerns about potential side effects. She agrees to begin drug therapy treatment with fluoxetine. You complete your assessment using the TeFA and the Short Side Effects Check List (sCKS). She tells you that she found the counseling session with the mental health clinician helpful. You encourage her to use the “Mood Enhancing Prescription” as much as possible and arrange to see her again in a week’s time with the usual proviso for her to call if things get worse or if she becomes suicidal. In all, you spend 20 minutes counseling Anna about her depression. Before her next scheduled visit, you contact the school counselor to update him on Anna’s situation and compare notes. The call lasts 10 minutes. On the same day, you also speak with her mental health clinician (with Anna’s permission), so that everyone has the same information. The call lasts 20 minutes. In total you have spent 30 minutes conferencing on the same day. Service Counseling#2 Fee Code # Units 00120 (MSP #2) Diagnostic Code: 311 Service Comm. Pt. Conf.#1 Fee Code 14077 or 14016 # Units X2 Diagnostic Code: 311 Service Counseling#3 Fee Code # Units 00120 (MSP #3) Diagnostic Code: 311 Service Comm. Pt. Conf.#1 Diagnostic Code: 311 Fee Code 14077 or 14016 # Units X2 You see Anna for 1 regular individual office visit and 2 group medical visits (90 minutes each) that you hold with a total of 10 youth patients at each group visit (each patient in the group is billed 1 unit per 30 min or greater portion) over the next two months and she continues to see the mental health clinician during that time. She seems to be making progress and after the 3rd office visit, you decide to schedule a longer visit to re-assess her mental health status Service Office Visit #1 When you see Anna for a 25 minute counseling session, to re-assess her mental health status, her KADS score is down to 7. She is taking fluoxetine 20 mg. daily and is tolerating it well. She continues to see the mental health clinician on a bi-weekly basis. Her functioning (which you have monitored using the TeFA) has improved somewhat as well. You arrange to see her for another counseling session in 3 weeks’ time. Service Counseling#4 You see Anna for another regular office visit; she seems to be making excellent progress and you decide to schedule a longer visit to re-assess her mental health status again. The visit is scheduled to take place in 3 weeks’ time. At Anna’s next 25 minute counseling session, her KADS score is 3 and has been 5 or less for 3 weeks. She is taking fluoxetine 20 mg. daily and is tolerating it well. She continues to see the mental health clinician on a bi-weekly basis. Her functioning (which you have monitored using the TeFA) has improved substantially as well. Fee Code 00100 # Units Diagnostic Code: 311 Service GMV #1 & 2 Fee Code 13770 # Units X 6 (3 units per GMV) Diagnostic Code: 311 Fee Code # Units 00120 (MSP #4) Diagnostic Code: 311 Service Office Visit #4 Fee Code 00100 # Units Diagnostic Code: 311 Service Counseling#5 Fee Code # Units 14044 (GPSC # 1) Diagnostic Code: 311 Billing notes: You are eligible to bill the appropriate units of 14077 if you are participating in the Attachment Initiative or 14016 if not participating, for the review, organization and revision of the care plan with allied care providers at any time during the year, whether you see the patient the same day or not. When you provided the minute mental health planning visit (14043), if in addition, you conference with other community allied care providers on the same day, you are eligible to bill the 14077 or 14016 units if all criteria are met. In addition, over the next 18 months, u p t o 5 telephone or email management contacts with patient are billable with the 14079. If you are participating in the Attachment Initiative, you also have access to 14076 Attachment Patient Telephone Management fees if you have used all 5 X 14079. After billing the mental health planning fee, you are eligible to access 4 additional mental health management (counseling equivalent) fees over the balance of the calendar year once the 4 MSP counseling fees have been used up.