adolescent health history
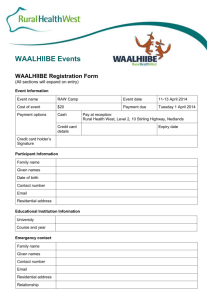
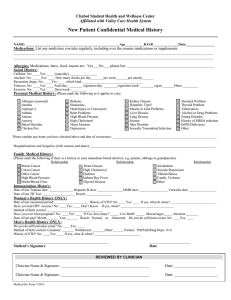
advertisement
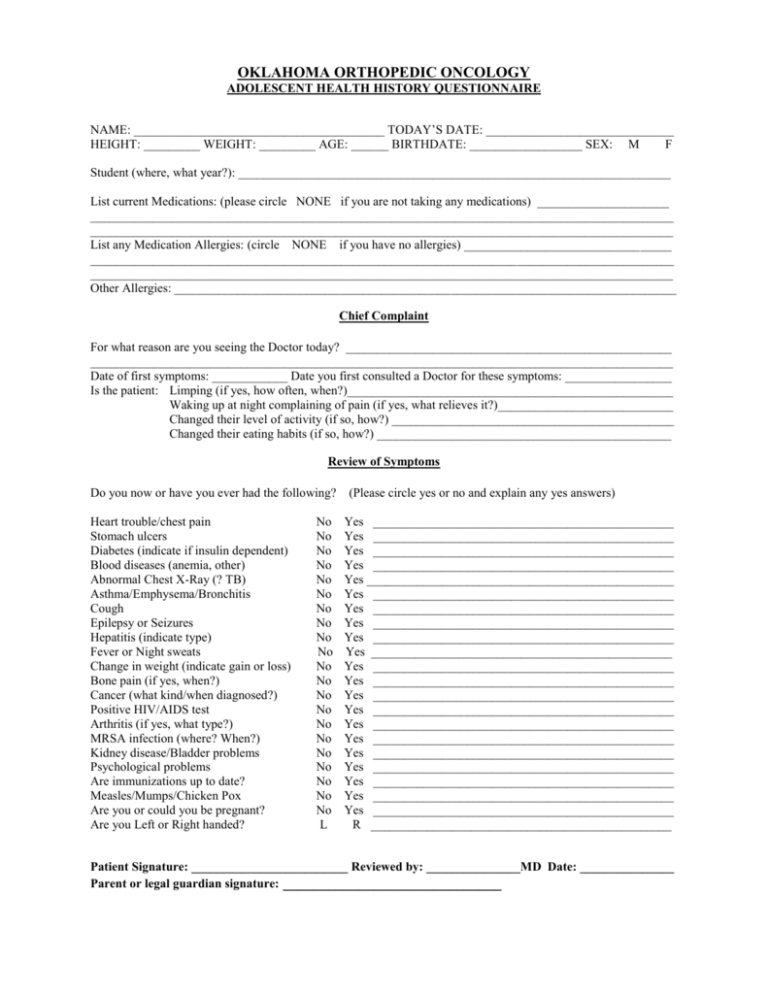
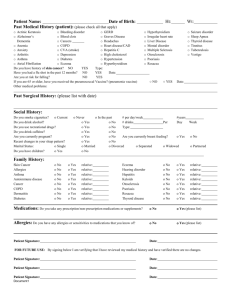
OKLAHOMA ORTHOPEDIC ONCOLOGY ADOLESCENT HEALTH HISTORY QUESTIONNAIRE NAME: ________________________________________ TODAY’S DATE: ______________________________ HEIGHT: _________ WEIGHT: _________ AGE: ______ BIRTHDATE: __________________ SEX: M F Student (where, what year?): _____________________________________________________________________ List current Medications: (please circle NONE if you are not taking any medications) _____________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ List any Medication Allergies: (circle NONE if you have no allergies) _________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ Other Allergies: ________________________________________________________________________________ Chief Complaint For what reason are you seeing the Doctor today? ____________________________________________________ _____________________________________________________________________________________________ Date of first symptoms: ____________ Date you first consulted a Doctor for these symptoms: _________________ Is the patient: Limping (if yes, how often, when?)____________________________________________________ Waking up at night complaining of pain (if yes, what relieves it?)____________________________ Changed their level of activity (if so, how?) _____________________________________________ Changed their eating habits (if so, how?) _______________________________________________ Review of Symptoms Do you now or have you ever had the following? Heart trouble/chest pain Stomach ulcers Diabetes (indicate if insulin dependent) Blood diseases (anemia, other) Abnormal Chest X-Ray (? TB) Asthma/Emphysema/Bronchitis Cough Epilepsy or Seizures Hepatitis (indicate type) Fever or Night sweats Change in weight (indicate gain or loss) Bone pain (if yes, when?) Cancer (what kind/when diagnosed?) Positive HIV/AIDS test Arthritis (if yes, what type?) MRSA infection (where? When?) Kidney disease/Bladder problems Psychological problems Are immunizations up to date? Measles/Mumps/Chicken Pox Are you or could you be pregnant? Are you Left or Right handed? No No No No No No No No No No No No No No No No No No No No No L (Please circle yes or no and explain any yes answers) Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes _________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ Yes ________________________________________________ R ________________________________________________ Patient Signature: _________________________ Reviewed by: _______________MD Date: _______________ Parent or legal guardian signature: _____________________________ HEALTH HISTORY QUESTIONNAIRE PAGE -2Past Medical / Surgical History List previous surgeries and approximate dates: _______________________________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ Any abnormal reactions to anesthesia? ______________________________________________________________ _____________________________________________________________________________________________ Any hospitalizations for non-surgical condition? (What condition/When?): _________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ Do you have any other chronic health conditions that we should know about? (neurofibromatosis, hepatitis, etc) ____________________________________________________________________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ Family History Any family history of significant medical illness, or cancer? (If yes, please describe problem and relationship to you): ________________________________________________________________________________________ _____________________________________________________________________________________________ _____________________________________________________________________________________________ Adolescent Social History In what type of dwelling do you live? ______________________________________________________________ Are there any siblings? No Yes (if yes, how many?) ______ Any health problems? _________________________ Are there stairs in your home? ____________________________________________________________________ Do you have any pets? No Yes (What/How many?) __________________________________________________ Do you smoke currently? No Yes Packs per day? _________________for_________years Quit Smoking? No Yes ______This year______>1 year ______>5 years_____ >10 years Do you drink alcoholic beverages? _______Never _____Occasionally ______Regularly Do you have a history of substance abuse? No Yes (If yes, what substance)______________________________ Do you exercise? ____ Daily ____Weekly ____Monthly ____Rarely ____Never What do you like to do for exercise? _______________________________________________________________ What do you do for fun? _________________________________________________________________________ Team Sports/Physical Education class?______________________________________________________________ Patient Signature: _________________________ Reviewed by: _______________MD Date: ______________ Parent or legal guardian signature: _____________________________