Incidence of deep vein thrombosis related to peripherally inserted
advertisement

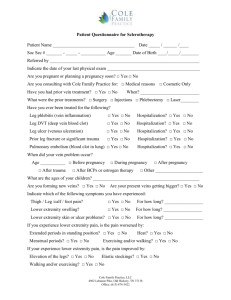
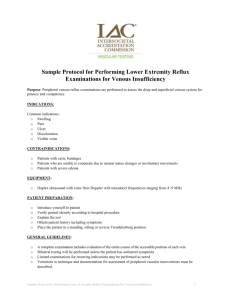
Incidence of deep vein thrombosis related to peripherally inserted central catheters in children and adolescents Josée Dubois, MD MSc, Françoise Rypens, MD, Laurent Garel, MD, Michèle David, MD, Jacques Lacroix, MD and France Gauvin, MD MSc From the Department of Radiology (Dubois, Rypens, Garel), the Department of Pediatrics Division of Hematology (David) and the Division of Pediatric Critical Care Medicine (Lacroix, Gauvin), Centre hospitalier universitaire Sainte-Justine, Montréal, Que. Top Abstract Methods Results Interpretation REFERENCES Abstract Background: Peripherally inserted central catheters (PICC) in children and adolescents are being used with increasing frequency. We sought to determine the incidence and characterize risk factors of deep vein thrombosis associated with peripherally inserted central catheters in a pediatric population. Methods: We conducted a prospective study involving consecutive patients referred to the radiology department of a tertiary care university-affiliated hospital for insertion of a peripherally inserted central catheter. We included patients aged 18 years or less who weighed more than 2.5 kg and had a peripherally inserted central catheter successfully inserted in his or her arm between June 2004 and November 2005. The primary outcome was the occurrence of partial or complete deep vein thrombosis evaluated by clinical examination, ultrasonography and venous angiography. Results: A total of 214 patients (101 girls, 113 boys) were included in the study. Partial or complete deep vein thrombosis occurred in 20 patients, for an incidence of 93.5 per 1000 patients and 3.85 per 1000 catheter-days. Only 1 of the cases was symptomatic. In the univariable analyses, the only variable significantly associated with deep vein thrombosis was the presence of factor II mutation G20210A (odds ratio 7.08, 95% confidence interval 1.11–45.15, p = 0.04), a genetic mutation that increases the risk of a blood clot and that was present in 5 (2.3%) of the 214 patients. Interpretation: The incidence of deep vein thrombosis related to peripherally inserted central catheters in our study was lower than the incidence related to centrally inserted venous catheters described in the pediatric literature (11%–50%). Most data available in the adult and pediatric literature on the incidence of deep vein thrombosis concern centrally inserted venous catheters, which are inserted directly in a central vein (jugular, subclavian or femoral). Typical symptoms of deep vein thrombosis are frequently absent in children and adolescents. Although the diagnosis of deep vein thrombosis is more reliable when based on Doppler ultrasonography or venous angiography,1–10 in most studies these diagnostic tests were performed only when patients presented clinical symptoms of deep vein thrombosis or catheter dysfunction. In studies focused on the pediatric population, the frequency of deep vein thrombosis related to centrally inserted venous catheters has varied from 11% to 50%.1,5,6,8,11 In the past 10 years, peripherally inserted central catheters (PICC) have been used with increasing frequency in children and adolescents. The catheter is inserted percutaneously via a peripheral vein, with its tip residing in the superior vena cava. The main indications for this type of catheter insertion are difficult venous access, home intravenous antibiotic therapy, administration of chemotherapy or other hyperosmolar solution and long-term parenteral nutrition. The risk of deep vein thrombosis related to peripherally inserted central catheters could be greater among children and adolescents than among adults, given the size of the veins. Several studies have published complications related to peripherally inserted central catheters,12–20 but few focused on the pediatric population.13–21 Furthermore, in all of these studies, screening for deep vein thrombosis was not systematic. The real incidence of deep vein thrombosis related to peripherally inserted central catheters and their complications in the pediatric population are therefore unknown. We conducted this study to determine the incidence and characterize the risk factors of deep vein thrombosis related to peripherally inserted central catheters in children and adolescents in our institution. Top Abstract Methods Results Interpretation REFERENCES Methods Study population We conducted this prospective study in a tertiary care university-affiliated pediatric hospital. We considered all consecutive patients referred to the radiology department for insertion of a peripherally inserted central catheter between June 2004 and November 2005 to be eligible for the study. The inclusion criteria were age 18 years or less, weight more than 2.5 kg and successful insertion of the catheter in the arm. Initial exclusion criteria and exclusions after enrolment are shown in Figure 1. Figure 1: Selection of patients for the study. View larger version (26K): [in this window] [in a new window] The Research Center Ethics and Scientific Committees of the Centre hospitalier universitaire Sainte-Justine approved this study. We obtained informed consent from the parents before including patients in the study. Catheter placement One of 3 experienced radiologists (J.D., L.G. and F.R.) inserted all peripherally inserted central catheters, using the same angiography room each time. We used 18-gauge (3.7 French) singlelumen catheters made of polyurethane. We inserted them under fluoroscopic guidance after angiographic opacification of upper-limb veins with an iodine contrast medium injected through a 25-gauge butterfly or Teflon needle inserted in a peripheral vein of the hand, as described previously14 (a detailed description of the procedure is in Appendix 1, available online at www.cmaj.ca/cgi/content/full/177/10/1185/DC2). We used angiographic opacification instead of ultrasonography because it provides better data on the permeability of vessels. We pushed the tip of the catheter under fluoroscopic guidance up to the junction of the superior vena cava and the right atrium. We standardized management of the in-dwelling catheter in hospital and during home care. Trained nurses flushed the catheters daily and after each use with heparinized saline (10 U/mL). The connectors were secured to the skin using Steri-Strip closure strips and covered with nonocclusive dressings. Risk factors We assessed the following variables at inclusion: age, sex, weight, history of deep vein thrombosis, underlying medical condition, presence of bacteremia or septicemia, thrombophilia and hypercoagulability. We systematically tested for 2 hereditary thrombophilias, factor V Leiden and factor II mutation G20210A, in each participant. We defined hypercoagulability as a platelet count greater than 440 x 109/L, a fibrinogen level greater than 4.0 g/L or a D-dimer level greater than 2.0 ng/L. We recorded the following variables at the time of catheter insertion: the number of punctures before successful insertion, the punctured vein (cephalic, basilic or humeral vein), the ratio between the diameter of the vein at the site of insertion and the catheter diameter as measured by venous angiography, and the length of fluoroscopic exposure. We assessed additional variables in patients retained for analysis throughout the study period: infection at the catheter site (diagnosed by clinical assessment and cultures), catheter dysfunction or obstruction (the inability to infuse a solution or the absence of reflux on aspiration), how long the catheter was in place, infusion of hyperosmolar solutions (hyperalimentation or chemotherapy) and blood product transfusion via the catheter. We considered all of these variables to be possible risk factors for deep vein thrombosis. Primary outcome The primary outcome was the occurrence of complete or partial deep vein thrombosis. We defined complete occlusion of the lumen vein as complete deep vein thrombosis and vascular filling defect with residual flow in the vein as partial deep vein thrombosis. We systematically screened all patients to detect the condition as soon as possible, using clinical assessment, Doppler ultrasonography and venous angiography. We considered deep vein thrombosis to be present if it was detected by either ultrasonography or venous angiography because they are the best diagnostic tools to detect the condition.22–25 A nurse trained in clinical examination looked for signs or symptoms of deep vein thrombosis at the time of referral to the radiology department; on days 2, 4, 7, 14, 21 and 28 (give or take 1 day) in the first month; once every subsequent month; and upon withdrawal of the catheter. We clinically suspected deep vein thrombosis when we observed at least 1 of the following symptoms: superficial collateral circulation, jugular swelling, vena cava syndrome, edema, pain, inflammation of the catheterized limb, fever or signs of a thrombotic complication (e.g., pulmonary embolism). We performed systematic ultrasound examinations at the time of referral to the radiology department; on days 2, 4, 7, 14, 21 and 28 (give or take 1 day); and once every subsequent month until removal of the catheter. The same 3 study radiologists (J.D., L.G. and F.R.) performed ultrasonographic examinations with a linear array or small pediatric transducer using grey-scale imaging and Doppler waveform analysis. The criteria for deep vein thrombosis diagnosed by ultrasonography were direct visualization of the thrombus, noncompressibility of the vessel, incomplete filling of the vein and disappearance of respiratory variations on venous flow.26 The presence of any of these criteria confirmed the diagnosis of partial or complete deep vein thrombosis. When one radiologist was unclear or uncertain about the diagnosis, a second radiologist independently performed another Doppler ultrasound. When there was disagreement between the 2 radiologists, they sought the opinion of the third radiologist to gain consensus. The nurse examination and the ultrasound examination were performed independently. We performed venous angiography under digital fluoroscopy before the insertion of the catheter at the time of referral to the radiology department. We also systematically performed venous angiography when the catheter was removed. Two of the 3 study radiologists independently reviewed the angiograms. In cases of discordance, the third radiologist reviewed the angiograms. The final diagnosis was based on the consensus of 2 of the 3 radiologists. When we diagnosed deep vein thrombosis, we always removed the peripherally inserted central catheters as soon as possible. There were no specific guidelines for further management and followup of deep vein thrombosis within the study; the attending physician assumed this responsibility when the catheters were removed. We did not collect data concerning management and follow-up of deep vein thrombosis for the study. Statistical analysis The incidence of deep vein thrombosis was described as rate (number of deep vein thromboses per 1000 patients with a peripherally inserted central catheter) and density (number of deep vein thromboses per 1000 catheter-days). In comparing characteristics of patients who developed deep vein thrombosis with patients who did not, we used a Wilcoxon rank sum for age and weight, and a 2 statistic for sex, underlying medical condition, presence of bacteremia or septicemia, history of deep vein thrombosis, thrombophilia and hypercoagulability. Comparisons were reported as odds ratios (OR) with their 95% confidence intervals (CI). Absolute p values were also calculated and reported. The threshold for statistical significance was p < 0.05 (2-tailed). No adjustment of the p value was made for multiple univariable analyses. We used Fisher's exact test if more than 20% of expected cell counts were less than 5. Concordance between experts was evaluated using a kappa score.27 Top Abstract Methods Results Interpretation REFERENCES Results Study population From June 2004 to November 2005, 728 patients were eligible for the study. Of these, 490 patients were excluded based on enrolment criteria, and an additional 24 were excluded or lost to follow-up after enrolment. No clinical deep vein thrombosis was reported in patients excluded after enrolment. The study population retained for analysis included a total of 214 patients (Figure 1). Clinical characteristics of the 214 patients are shown in Table 1. Twenty percent of the patients were less than 1 year old. The most frequent underlying disease requiring catheter insertion was infectious disease (53.3%), which included mainly pneumonia, mastoiditis and osteomyelitis. We detected congenital thrombophilia due to factor II mutation G20210A in 5 patients (2.3%). We inserted most catheters (72.0%) in the humeral or basilic vein rather than the cephalic vein. Only one puncture was required in most patients (79.4%). Fluoroscopic time was less than 1 minute in 45.0% of the cases. The data we collected during the study showed that catheter infection occurred in 7.5% of the patients and catheter dysfunction in 7.9%. The mean dwell time was 24.3 (min–max 2.7–45.9) days (median 17.0 days, range 1–125). We used hyperalimentation in 11.7% and blood products in 7.5% of patients respectively. View this table: Table 1. [in this window] [in a new window] Incidence of deep vein thrombosis The total number of catheter-days was 5190. Only 1 patient presented clinical signs of deep vein thrombosis (edema of upper limb); all other cases of deep vein thrombosis were asymptomatic. Twenty patients had either a partial or complete deep vein thrombosis, for an incidence rate of 93.5 per 1000 patients and an incidence density of 3.85 per 1000 catheter-days. We observed complete deep vein thrombosis in 3 children, for an incidence rate of 14.0 per 1000 patients and an incidence density of 0.58 per 1000 catheter-days. We diagnosed complete deep vein thrombosis using both venous angiography and ultrasonography in 2 patients, and venous angiography alone in 1 patient. We observed partial deep vein thrombosis in 17 patients, for an incidence rate of 79.4 per 1000 patients and an incidence density of 3.28 per 1000 catheter-days. We diagnosed partial deep vein thrombosis using both venous angiography and ultrasonography in 8 patients, and venous angiography alone in 9 patients. We did not detect deep vein thrombosis using ultrasound alone. Reproducibility between the 2 radiologists was almost perfect (kappa value 0.87). The opinion of the third radiologist was needed on 1 occasion to gain consensus. Risk factors The results of the univariable analyses on possible risk factors predicting the occurrence of deep vein thrombosis related to peripherally inserted central catheters are shown in Table 1 and Figure 2. The only significant risk factor of deep vein thrombosis was the presence of factor II mutation G20210A, which was present in 2.3% of the study population (OR 7.08, 95% CI 1.11–45.15, p = 0.04). Figure 2: Forest plot showing the odds ratios for risk of deep vein thrombosis among 214 children and adolescents who received peripherally inserted central catheters. Note: OR = odds ratio, CI = confidence interval. View larger version (21K): [in this window] [in a new window] Interpretation Top Our results call into question the validity of previous findings from studies on the Abstract incidence rate of deep vein thrombosis related to peripherally inserted central Methods Results catheters in a pediatric population. The reported incidence rates varied from 0% to 14,20,21,22 Interpretation 5%; however, Doppler ultrasonography was performed only in patients REFERENCES who were symptomatic. In our study, we found that symptoms and signs were not reliable diagnostic markers; our use of Doppler ultrasonography in all patients (symptomatic and asymptomatic) revealed an incidence rate of 9.3%. Only 1 of the 20 patients with deep vein thrombosis presented with clinical signs. Our findings suggest that the risk of deep vein thrombosis is lower with peripherally inserted central catheters than with centrally inserted venous catheters. Two studies of centrally inserted venous catheters using serial screening for deep vein thrombosis by Doppler ultrasonography are available in the pediatric literature. In a prospective study of femoral catheter-related deep vein thrombosis in children and adolescents, Talbott and colleagues8 reported the occurrence of deep vein thrombosis in 7 of 20 patients, for an overall incidence rate of 35%. Beck and colleagues1 reported the occurrence of deep vein thrombosis in 17 of 93 children with a centrally inserted venous catheter (subclavian or jugular), for an incidence rate of 18.3%. These rates are higher than the incidence rate related to peripherally inserted central catheters in our study (9.3%). We observed a significant association between factor II mutation G20210A and deep vein thrombosis in our univariable analysis. Factor II mutation G20210A and factor V Leiden are the most commonly found prothrombotic risk factors associated with thrombosis during childhood and adolescence.28–30 The prevalence in our study population was low, similar to that reported in other populations of mainly European descent (2.3%).31,32 Three studies of centrally inserted venous catheters reported an increased risk of deep vein thrombosis (12%–50%) among adults and pediatric patients with cancer.5,21,27 In our study, 6 (13%) of 47 patients with cancer had a deep vein thrombosis. We did not find a statistically significant association between cancer and deep vein thrombosis related to peripherally inserted central catheters. Some data suggest that peripherally inserted central catheters may be safer to use than centrally inserted venous catheters in patients with cancer. In a cohort of 53 children and adolescents with cancer who received peripherally inserted central catheters, no deep vein thrombosis was observed.21 In another prospective study involving pediatric and adult cancer patients with peripherally inserted central catheters, Walshe and colleagues33 reported a deep vein thrombosis incidence rate of 10.6 per 1000 catheter-days. Other possible risk factors of deep vein thrombosis are suggested in the medical literature, such as blood product transfusion,34 infusion of hyperosmolar solutions,35 insertion of peripherally inserted central catheters in cephalic veins36 or use of a catheter too large for the vein through which it is inserted. In our study, we did not find a statistically significant relation between these possible factors and outcome, but this may be due to the small number of patients in our study who had similar risk factors to those listed above. The main limitation of our study is the small number of cases of deep vein thrombosis (3 complete and 17 partial) detected. Although the incidence rate of complete deep vein thrombosis (9.3%) that we observed was higher than the rates reported previously in the literature, this rate was nevertheless significantly lower than we anticipated it would be. The sample size estimated for the study, which we calculated using a higher incidence rate of deep vein thrombosis, may have been insufficient to clearly determine risk factors. However, such a low incidence rate of deep vein thrombosis related to peripherally inserted central catheters may be attributable to other reasons, such as the safety of peripherally inserted central catheters compared with centrally inserted venous catheters, the expertise of the physician who inserted the catheter or the standardized procedure used. Since all of the catheters in our study were inserted in the angiography room, our results cannot be generalized to catheters inserted at the bedside without fluoroscopic control. Our study has several strengths: the sample size was substantial compared with those in previous studies in the pediatric population; the study was done prospectively with consecutive patients, which enhances its representativeness; we monitored patients prospectively and systematically with regular clinical evaluations and examinations with ultrasonography and venous angiography; and all of the diagnoses were adjudicated by at least 2 of 3 radiologists. In summary, the incidence rate of deep vein thrombosis related to peripherally inserted central catheters among patients aged 18 years or younger in our study (9.3%) is higher than that reported in previous studies on this type of catheter, owing to our use of Doppler ultrasonography. However, the incidence is lower than the reported rate related to centrally inserted venous catheters, which suggests that peripherally inserted central catheters are safer. All but 1 of the cases of deep vein thrombosis in our study were asymptomatic, which means that only studies involving systematic and repeated evaluation with Doppler ultrasonography or venous angiography can be considered reliable. Footnotes Une version française de ce résumé est disponible à l'adresse www.cmaj.ca/cgi/content/full/177/10/1185/DC1 This article has been peer reviewed. Contributors: Josée Dubois, France Gauvin, Jacques Lacroix and Michèle David contributed to the study conception and design. Josée Dubois, Françoise Rypens and Laurent Garel contributed to the data acquisition and interpretation. Josée Dubois, France Gauvin and Jacques Lacroix contributed to the data analysis and drafted the manuscript. All of the authors contributed to the critical revision of the manuscript and approved the final version. Acknowledgements: We thank John Podoba (biostatistician) for the statistical analysis and Johanne Lavallée, Anna Proietti and Nathalie Thomas (research assistants) for collecting data and for their clinical assistance. This study was supported by a grant from the Fonds de la recherche en santé du Québec. Competing interests: None declared. REFERENCES 1. Beck C, Dubois J, Grignon A, et al. Incidence and risk factors of catheterrelated deep vein thrombosis in a pediatric intensive care unit: a prospective study. J Pediatr 1998;133:237-41.[CrossRef][Medline] Top Abstract Methods Results Interpretation REFERENCES 2. Bozzetti F, Scarpa D, Terno G, et al. Subclavian venous thrombosis due to indwelling catheters: a prospective study on 52 patients. JPEN J Parenter Enteral Nutr 1983;7:5602.[Abstract/Free Full Text] 3. Lokich JJ, Becker B. Subclavian vein thrombosis in patients treated with infusion chemotherapy for advanced malignancy. Cancer 1983;52:1586-9.[CrossRef][Medline] 4. Valerio D, Hussey JK, Smith FW. Central vein thrombosis associated with intravenous feeding — a prospective study. JPEN J Parenter Enteral Nutr 1981;5:2402.[Abstract/Free Full Text] 5. Glaser DW, Medeiros D, Rollins N, et al. Catheter-related thrombosis in children with cancer. J Pediatr 2001;138:255-9.[CrossRef][Medline] 6. Krafte-Jacobs B, Sivit CJ, Mejia R, et al. Catheter-related thrombosis in critically ill children: comparison of catheters with and without heparin bonding. J Pediatr 1995;126:504.[CrossRef][Medline] 7. Shefler A, Gillis J, Lam A, et al. Inferior vena cava thrombosis as a complication of femoral vein catheterisation. Arch Dis Child 1995;72:343-5.[Abstract/Free Full Text] 8. Talbott GA, Winters WD, Bratton SL, et al. A prospective study of femoral catheter-related thrombosis in children. Arch Pediatr Adolesc Med 1995;149:28891.[Abstract/Free Full Text] 9. Merrer J, De Jonghe B, Golliot F, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA 2001;286:7007.[Abstract/Free Full Text] 10. Trerotola SO, Kuhn-Fulton J, Johnson MS, et al. Tunneled infusion catheters: increased incidence of symptomatic venous thrombosis after subclavian versus internal jugular venous access. Radiology 2000;217:89-93.[Abstract/Free Full Text] 11. Goutail-Flaud MF, Sfez M, Berg A, et al. Central venous catheter-related complications in newborns and infants: a 587-case survey. J Pediatr Surg 1991;26:64550.[CrossRef][Medline] 12. Valk WJ, Liem KD, Geven WB. Seldinger technique as an alternative approach for percutaneous insertion of hydrophilic polyurethane central venous catheters in newborns. JPEN J Parenter Enteral Nutr 1995;19:151-5.[Abstract/Free Full Text] 13. Durand M, Ramanathan R, Martinelli B, et al. Prospective evaluation of percutaneous central venous silastic catheters in newborn infants with birth weights of 510 to 3,920 grams. Pediatrics 1986;78:245-50.[Abstract/Free Full Text] 14. Dubois J, Garel L, Tapiero B, et al. Peripherally inserted central catheters in infants and children. Radiology 1997;204:622-6.[Abstract/Free Full Text] 15. Shulman RJ, Pokorny WJ, Martin CG, et al. Comparison of percutaneous and surgical placement of central venous catheters in neonates. J Pediatr Surg 1986;21:348-50.[Medline] 16. Dolcourt JL, Bose CL. Percutaneous insertion of silastic central venous catheters in newborn infants. Pediatrics 1982;70:484-6.[Abstract/Free Full Text] 17. Loughran SC, Borzatta M. Peripherally inserted central catheters: a report of 2506 catheter days. JPEN J Parenter Enteral Nutr 1995;19:133-6.[Abstract/Free Full Text] 18. Smith JR, Friedell ML, Cheatham ML, et al. Peripherally inserted central catheters revisited. Am J Surg 1998;176:208-11.[CrossRef][Medline] 19. Crowley JJ, Pereira JK, Harris LS, et al. Peripherally inserted central catheters: experience in 523 children. Radiology 1997;204:617-21.[Abstract/Free Full Text] 20. Chait PG, Ingram J, Phillips-Gordon C, et al. Peripherally inserted central catheters in children. Radiology 1995;197:775-8.[Abstract/Free Full Text] 21. Matsuzaki A, Suminoe A, Koga Y, et al. Long-term use of peripherally inserted central venous catheters for cancer chemotherapy in children. Support Care Cancer 2006;14:15360.[CrossRef][Medline] 22. Ryder MA. Peripheral access options. Surg Oncol Clin N Am 1995;4:395-427.[Medline] 23. Male C, Chait P, Ginsberg JS, et al. Comparison of venography and ultrasound for the diagnosis of asymptomatic deep vein thrombosis in the upper body in children: results of the PARKAA study. Prophylactic Antithrombin Replacement in Kids with ALL treated with Asparaginase. Thromb Haemost 2002;87:593-8.[Medline] 24. Mustafa BO, Rathbun SW, Whitsett TL, et al. Sensitivity and specificity of ultrasonography in the diagnosis of upper extremity deep vein thrombosis: a systematic review. Arch Intern Med 2002;162:401-4.[Abstract/Free Full Text] 25. Wechsler RJ, Spirn PW, Conant EF, et al. Thrombosis and infection caused by thoracic venous catheters: pathogenesis and imaging findings. AJR Am J Roentgenol 1993;160:46771.[Free Full Text] 26. Prandoni P, Polistena P, Bernardi E, et al. Upper-extremity deep vein thrombosis. Risk factors, diagnosis, and complications. Arch Intern Med 1997;157:5762.[Abstract/Free Full Text] 27. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74.[CrossRef][Medline] 28. Bertina RM, Koeleman BP, Koster T, et al. Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature 1994;369:647.[CrossRef][Medline] 29. Schobess R, Junker R, Auberger K, et al. Factor V G1691A and prothrombin G20210A in childhood spontaneous venous thrombosis–evidence of an age-dependent thrombotic onset in carriers of factor V G1691A and prothrombin G20210A mutation. Eur J Pediatr 1999;158(Suppl 3):S105-8. 30. Junker R, Koch HG, Auberger K, et al. Prothrombin G20210A gene mutation and further prothrombotic risk factors in childhood thrombophilia. Arterioscler Thromb Vasc Biol 1999;19:2568-72.[Abstract/Free Full Text] 31. Poort SR, Rosendaal FR, Reitsma PH, et al. A common genetic variation in the 3'untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood 1996;88:3698703.[Abstract/Free Full Text] 32. Infante-Rivard C, Rivard GE, Yotov WV, et al. Absence of association of thrombophilia polymorphisms with intrauterine growth restriction. N Engl J Med 2002;347:1925.[Abstract/Free Full Text] 33. Walshe LJ, Malak SF, Eagan J, et al. Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol 2002;20:327681.[Abstract/Free Full Text] 34. Desmet L, Lacroix J. Transfusion in pediatrics. Crit Care Clin 2004;20:299311.[CrossRef][Medline] 35. Lacroix J, Pineault M, Rozé J. Alimentation entérale et parentérale. In: Lacroix J, Gauthier M, Beaufils F, editors. Urgences et soins intensifs pédiatriques: une approche clinique multidisciplinaire. Montréal: Presses de l'Université de Montréal; 1994. p. 103-4. 36. Allen AW, Megargell JL, Brown DB, et al. Venous thrombosis associated with the placement of peripherally inserted central catheters. J Vasc Interv Radiol 2000;11:130914.[Medline]