My thoughts re rehab programme pilot
advertisement
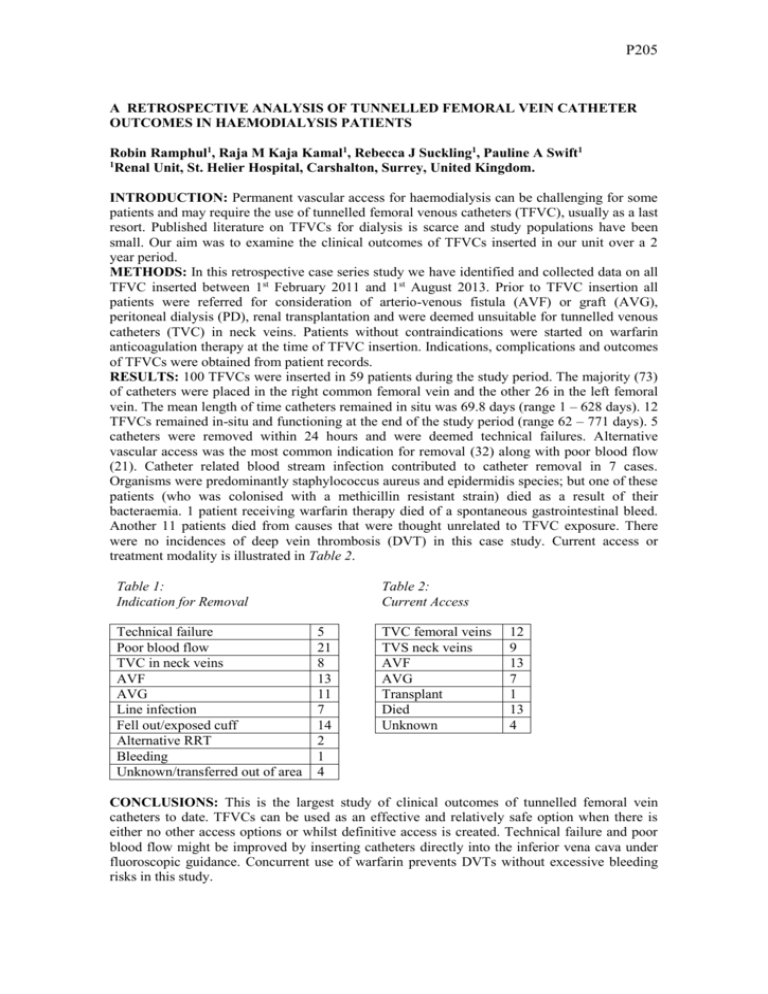
P205 A RETROSPECTIVE ANALYSIS OF TUNNELLED FEMORAL VEIN CATHETER OUTCOMES IN HAEMODIALYSIS PATIENTS Robin Ramphul1, Raja M Kaja Kamal1, Rebecca J Suckling1, Pauline A Swift1 1 Renal Unit, St. Helier Hospital, Carshalton, Surrey, United Kingdom. INTRODUCTION: Permanent vascular access for haemodialysis can be challenging for some patients and may require the use of tunnelled femoral venous catheters (TFVC), usually as a last resort. Published literature on TFVCs for dialysis is scarce and study populations have been small. Our aim was to examine the clinical outcomes of TFVCs inserted in our unit over a 2 year period. METHODS: In this retrospective case series study we have identified and collected data on all TFVC inserted between 1st February 2011 and 1st August 2013. Prior to TFVC insertion all patients were referred for consideration of arterio-venous fistula (AVF) or graft (AVG), peritoneal dialysis (PD), renal transplantation and were deemed unsuitable for tunnelled venous catheters (TVC) in neck veins. Patients without contraindications were started on warfarin anticoagulation therapy at the time of TFVC insertion. Indications, complications and outcomes of TFVCs were obtained from patient records. RESULTS: 100 TFVCs were inserted in 59 patients during the study period. The majority (73) of catheters were placed in the right common femoral vein and the other 26 in the left femoral vein. The mean length of time catheters remained in situ was 69.8 days (range 1 – 628 days). 12 TFVCs remained in-situ and functioning at the end of the study period (range 62 – 771 days). 5 catheters were removed within 24 hours and were deemed technical failures. Alternative vascular access was the most common indication for removal (32) along with poor blood flow (21). Catheter related blood stream infection contributed to catheter removal in 7 cases. Organisms were predominantly staphylococcus aureus and epidermidis species; but one of these patients (who was colonised with a methicillin resistant strain) died as a result of their bacteraemia. 1 patient receiving warfarin therapy died of a spontaneous gastrointestinal bleed. Another 11 patients died from causes that were thought unrelated to TFVC exposure. There were no incidences of deep vein thrombosis (DVT) in this case study. Current access or treatment modality is illustrated in Table 2. Table 1: Indication for Removal Technical failure Poor blood flow TVC in neck veins AVF AVG Line infection Fell out/exposed cuff Alternative RRT Bleeding Unknown/transferred out of area Table 2: Current Access 5 21 8 13 11 7 14 2 1 4 TVC femoral veins TVS neck veins AVF AVG Transplant Died Unknown 12 9 13 7 1 13 4 CONCLUSIONS: This is the largest study of clinical outcomes of tunnelled femoral vein catheters to date. TFVCs can be used as an effective and relatively safe option when there is either no other access options or whilst definitive access is created. Technical failure and poor blood flow might be improved by inserting catheters directly into the inferior vena cava under fluoroscopic guidance. Concurrent use of warfarin prevents DVTs without excessive bleeding risks in this study.