Port-A-Cath - An-Najah National University
advertisement

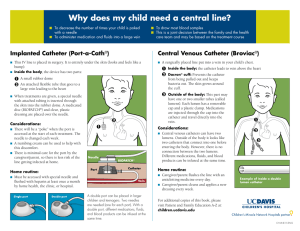
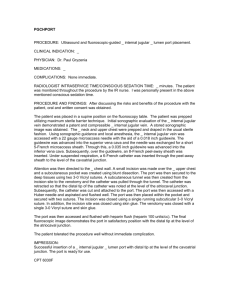
Port-A-Cath Dr. Aidah Alkaissi An-Najah National University College of Nursing Port-a-Cath with needle assembly inserted Chest X-ray showing an implanted port. Port-A-Cath • is a device that is used to make administration of chemotherapy easier. • It can also reduce the risk of certain chemotherapy related complications. • This device is placed under the skin, in upper part of the chest. • It has a small reservoir that is connected to a major vein inside the chest. • This device facilitates administration of chemotherapy into the venous system. • Some of chemotherapy drugs can cause major problems if they leak from the veins in to the surrounding tissues. • Such damage could be very dangerous and difficult to treat. • This may happen if certain drugs are administered into a vein in the arm. • In addition, since patients will need frequent injections and intra venous treatments, very soon may run out of usable veins. • The term portacath is a portmanteau of "portal" and "catheter". • The term totally implantable venous access system (TIVAS) is also used. • Additionally, a portacath is the main form of a central venous access device, and is frequently referred to as such in the medical field. • A port consists of a reservoir compartment (the portal) that has a silicone bubble for needle insertion (the septum), with an attached plastic tube (the catheter). • The device is surgically inserted under the skin in the upper chest or in the arm and appears as a bump under the skin. • It requires no special maintenance and is completely internal so swimming and bathing are not a problem. • The catheter runs from the portal and is surgically inserted into a vein (usually the jugular vein, subclavian vein, or superior vena cava). Ideally, the catheter terminates in the superior vena cava, just upstream of the right atrium. This position allows infused agents to be spread throughout the body quickly and efficiently. • The septum is made of a special self-sealing silicone rubber; it can be punctured hundreds of times before it weakens significantly. • To administer treatment or to withdraw blood, a health professional will first locate the port and disinfect the area. • Then he or she will access the port by puncturing the overlying skin with a 90° Huber point needle although a winged needle may also be used. • (Due to its design, there is a very low infection risk, as the breach of skin integrity is never larger than the caliber of the needle. • Negative pressure is created to withdraw blood into the vacuumized needle, to check for blood return and see if the port is functioning normally. • Next, the port will be flushed with a saline solution. • Then, treatment will begin. • After each use, a heparin lock is made by injecting a small amount of heparinized saline (an anticoagulant) into the device. • This prevents development of clots within the port or catheter. • In some catheter designs where there is a self-sealing valve at the far end, the system is locked with just saline. • The port can be left accessed for as long as required. The port is covered in a dressing to protect the site from infection and to secure the needle in position. Uses • • • • • • • • • To deliver total parenteral nutrition in those unable to take (adequate) food orally for a long period of time. To deliver chemotherapy to cancer patients who must undergo treatment frequently. Chemotherapy is often toxic, and can damage skin and muscle tissue, and therefore should not be delivered through these tissues. Portacaths provide a solution, delivering drugs quickly and efficiently through the entire body via the circulatory system. To deliver coagulation factors in patients with severe hemophilia. To withdraw (and/or return) blood to the body in patients who require frequent blood tests, and in hemodialysis patients. To deliver antibiotics to patients requiring them for a long time or frequently, such as those with cystic fibrosis and bronchiectasis. Delivering medications to patients with immune disorders. For treating alpha 1-antitrypsin deficiency with replacement therapy For delivering radiopaque contrast agents, which enhance contrast in CT imaging. To fill or withdraw fluid from the Lap-Band or Realize gastric bands used in Bariatric surgeries Risks • Infection - a severe bacterial infection can compromise the device, require its surgical removal, and seriously jeopardize the health of the already weak patient. • Thrombosis - formation of a blood clot in the catheter may block the device irrevocably. To prevent clotting the portacath is flushed with saline and heparin, usually by a nurse or other medical professional, or someone properly trained that is a family member or the patient, at least once every four weeks, or more often in conjunction with administering medication. • Pneumothorax - Attempts to gain access to the subclavian vein or jugular vein can injure the lung, possibly leading to this complication. If the pneumothorax is large enough, a chest tube might need to be placed. In experienced hands, the incidence of this complication is about 1%. Arterial injury - The subclavian artery can be inadvertently punctured. This usually leads to a subcutaneous hematoma and occasionally a pseudoaneurysm. • Films • http://www.youtube.com/watch?v=5k1rcc5MZo • http://www.youtube.com/watch?v=esG42dC4q4&feature=related