ADULT INTERRUPT SEDATION/ANALGESIC INFUSION and
advertisement
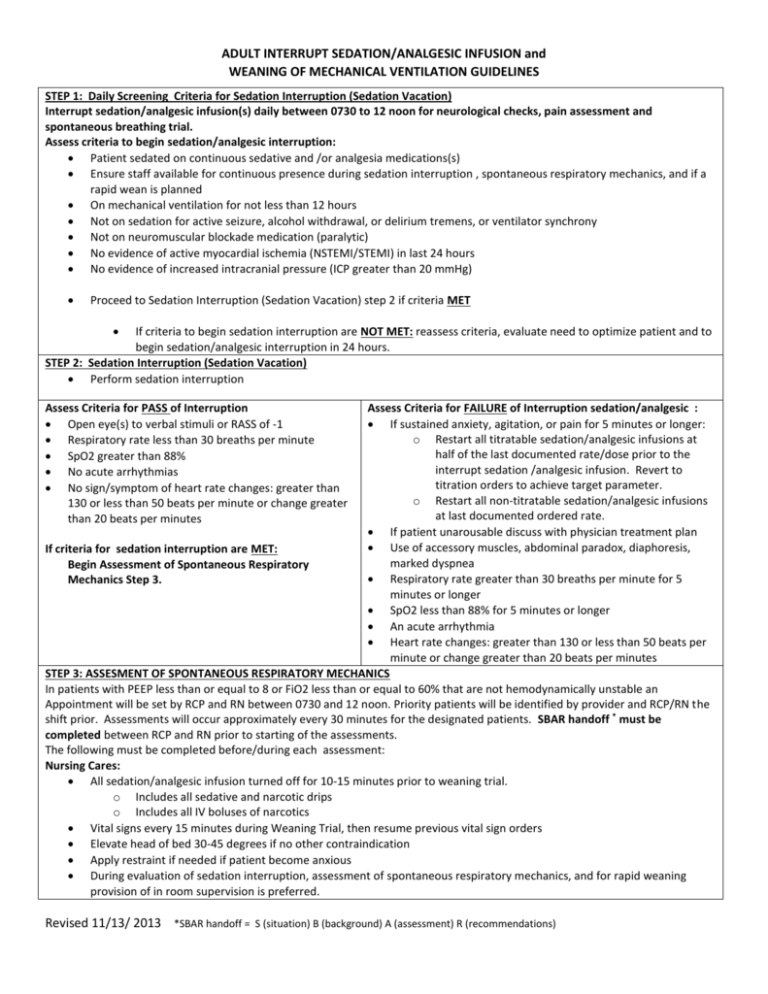
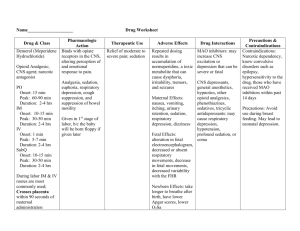
ADULT INTERRUPT SEDATION/ANALGESIC INFUSION and WEANING OF MECHANICAL VENTILATION GUIDELINES STEP 1: Daily Screening Criteria for Sedation Interruption (Sedation Vacation) Interrupt sedation/analgesic infusion(s) daily between 0730 to 12 noon for neurological checks, pain assessment and spontaneous breathing trial. Assess criteria to begin sedation/analgesic interruption: Patient sedated on continuous sedative and /or analgesia medications(s) Ensure staff available for continuous presence during sedation interruption , spontaneous respiratory mechanics, and if a rapid wean is planned On mechanical ventilation for not less than 12 hours Not on sedation for active seizure, alcohol withdrawal, or delirium tremens, or ventilator synchrony Not on neuromuscular blockade medication (paralytic) No evidence of active myocardial ischemia (NSTEMI/STEMI) in last 24 hours No evidence of increased intracranial pressure (ICP greater than 20 mmHg) Proceed to Sedation Interruption (Sedation Vacation) step 2 if criteria MET If criteria to begin sedation interruption are NOT MET: reassess criteria, evaluate need to optimize patient and to begin sedation/analgesic interruption in 24 hours. STEP 2: Sedation Interruption (Sedation Vacation) Perform sedation interruption Assess Criteria for PASS of Interruption Open eye(s) to verbal stimuli or RASS of -1 Respiratory rate less than 30 breaths per minute SpO2 greater than 88% No acute arrhythmias No sign/symptom of heart rate changes: greater than 130 or less than 50 beats per minute or change greater than 20 beats per minutes Assess Criteria for FAILURE of Interruption sedation/analgesic : If sustained anxiety, agitation, or pain for 5 minutes or longer: o Restart all titratable sedation/analgesic infusions at half of the last documented rate/dose prior to the interrupt sedation /analgesic infusion. Revert to titration orders to achieve target parameter. o Restart all non-titratable sedation/analgesic infusions at last documented ordered rate. If patient unarousable discuss with physician treatment plan Use of accessory muscles, abdominal paradox, diaphoresis, If criteria for sedation interruption are MET: marked dyspnea Begin Assessment of Spontaneous Respiratory Respiratory rate greater than 30 breaths per minute for 5 Mechanics Step 3. minutes or longer SpO2 less than 88% for 5 minutes or longer An acute arrhythmia Heart rate changes: greater than 130 or less than 50 beats per minute or change greater than 20 beats per minutes STEP 3: ASSESMENT OF SPONTANEOUS RESPIRATORY MECHANICS In patients with PEEP less than or equal to 8 or FiO2 less than or equal to 60% that are not hemodynamically unstable an Appointment will be set by RCP and RN between 0730 and 12 noon. Priority patients will be identified by provider and RCP/RN the shift prior. Assessments will occur approximately every 30 minutes for the designated patients. SBAR handoff * must be completed between RCP and RN prior to starting of the assessments. The following must be completed before/during each assessment: Nursing Cares: All sedation/analgesic infusion turned off for 10-15 minutes prior to weaning trial. o Includes all sedative and narcotic drips o Includes all IV boluses of narcotics Vital signs every 15 minutes during Weaning Trial, then resume previous vital sign orders Elevate head of bed 30-45 degrees if no other contraindication Apply restraint if needed if patient become anxious During evaluation of sedation interruption, assessment of spontaneous respiratory mechanics, and for rapid weaning provision of in room supervision is preferred. Revised 11/13/ 2013 *SBAR handoff = S (situation) B (background) A (assessment) R (recommendations) ADULT INTERRUPT SEDATION/ANALGESIC INFUSION and WEANING OF MECHANICAL VENTILATION GUIDELINES Respiratory Care Provider (RCP) Cares: If nebulized medication is ordered, administer prior to starting assessment Ventilator Settings: Wean patient to CPAP or PS setting. Document spontaneous respiratory mechanics Arterial blood gases: o Before start of Weaning Trial (unless results from today are available on the same settings) o If patient progresses to weaning trial after assessment of spontaneous respiratory mechanics o Provider may elect not to obtain post weaning trial ABG Spontaneous Respiratory Mechanics PASS Criteria: o SpO2 is greater than 88% on FiO2 of less than 60% o Minute ventilation 5 to 15 L/min o Spontaneous respiratory rate less than 30 breaths/min o Spontaneous VT greater than 300 mL or greater than 5 mL/kg o Rapid shallow breathing index (RSBI) 105 or less (RSBI = frequency/VT) o PEEP equal to or less than 8 cmH2O o Absence of : sustained anxiety or agitation accessory muscles usage, abdominal paradox, diaphoresis, and marked dyspnea sign/symptom of heart rate changes: greater than 130 or less than 50 beats per minute or change greater than 20 beats per minutes acute MAP changes greater than 20mmHg RCP Cares: Initiate Weaning Trial: If criteria met, wean patient to CPAP or Pressure Support (PS) ventilator setting If Criteria Not Met : Notify prescriber of failed spontaneous respiratory mechanics and confirm return to patient’s previous ventilator order settings. STEP 4: Weaning Trial Weaning Trial PASS Criteria: When patient’s results post Weaning Trial are NOT within the Cough or gag reflex present with deflated cuff “Weaning Trial PASS Criteria”: Audible air leak around ETT Nursing Cares: Arterial blood gas results (as indicated): o Restart all titratable sedation/analgesic infusions at pH 7.30 or greater PCO2 rise of no more than 10 or more half of the last documented rate/dose prior to the from baseline interrupt sedation /analgesic infusion. Revert to PaO2 greater than 60 torr on 60% of FiO2 titration orders to achieve target parameter. or less o Restart all non-titratable sedation/analgesic infusions at last documented ordered rate. Notify prescriber for extubation order when the patient’s results after Weaning Trial are RCP Cares: met. o Notify prescriber when weaning criteria are not met. o Assess opportunity to optimize patient for next If weaning trial criteria MET Proceed to weaning trial Extubation Step 5 o Document time of failure, what criteria were not met and any complication in nursing and RCP electronic record o RCP to place patient to previous ventilator order setting STEP 5: Extubation Nursing preparation for extubation: Mouth Care with Chlorohexidine 0.12% 15 mL scrub the oral cavity prior to deflating cuff for extubation Revised 11/13/ 2013 *SBAR handoff = S (situation) B (background) A (assessment) R (recommendations)