Tribal Rural Behavioral Health Clinical Handbook
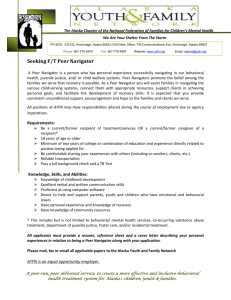
advertisement

Tribal Rural Behavioral Health Clinical Handbook Desk Guide S BHC o Developed by: Behavioral Health Compliance Solutions, LLC TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (To move to a specific page from the Table of Contents, place your cursor on the page number and press control+click on your keyboard. To return to the Table of Contents, place your cursor on the arrow at the bottom of the page and press control+click on your keyboard...) TABLE OF CONTENTS TABLE OF CONTENTS .................................................................................................................................. 1 1.0 SCOPE .............................................................................................................................................. 7 2.0 INTRODUCTION............................................................................................................................ 8 3.0 RECIPIENT ELIGIBILITY ........................................................................................................... 8 3.1 Recipient Eligibility for Medicaid Behavioral Health Services 7 AAC 135.020 ........................ 8 3.1.1 Recipient Eligibility Clinic Services ............................................................................................... 8 3.1.2 Recipient Eligibility Rehabilitation Services ................................................................................. 8 3.2. Recipient Eligibility Definitions ...................................................................................................... 9 3.2.1 Child Experiencing an Emotional Disturbance 7 AAC 70.990. (9) Definitions ....................... 9 3.2.2 Adult Experiencing an Emotional Disturbance 7 AAC 70.990. (3) Definitions ......................... 9 3.2.3 Child or Adult with a Substance Use Disorder 7 AAC 70.990. (31) Definitions ....................... 9 3.2.4 Child Experiencing a Severe Emotional Disturbance (SED) 7 AAC 70.990. (9) Definitions .... 9 3.2.5 Adult Experiencing a Serious Mental Illness (SMI) 7 AAC 70.990. (2) .................................. 10 4.0 STAFF QUALIFICATIONS ........................................................................................................ 10 4.1 Staff ................................................................................................................................................. 10 4.1.1 Behavioral Health Clinical Associate 7 AAC 70.990. (3) Definitions .................................... 10 4.1.2 Directing Clinician 7 AAC 70.990. (13) Definitions .................................................................. 10 4.1.3 Mental Health Professional Clinician 7 AAC 70.990. (28) Definitions ................................... 10 4.1.4 Peer Support Specialist 7 AAC 135.210 ..................................................................................... 11 4.1.5 Substance Use Disorder Counselor 7 AAC 70.990. (32) Definitions ....................................... 12 1 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 5.0 Clinical Record Requirements ...................................................................................................... 12 5.1 6.0 7 AAC 105.230. Requirements for provider records .................................................................. 12 SERVICE REQUIREMENTS ...................................................................................................... 14 6.1 Initial Services ................................................................................................................................ 14 6.1.1 Behavioral Health Screening Alaska Screening Tool (AST) 7 AAC 135.100 ......................... 14 6.1.2 Client Status Review (CSR) Initial 6.1.3 Screening, Brief Intervention, and Referral to Treatment (SBIRT) 7 AAC 135.240 ............. 14 6.2 Professional Behavioral Health Assessments 6.2.2 Substance Abuse Assessment 6.2.3 Integrated Mental Health and Substance Abuse Assessment 7 AAC 135.110 (d) ................. 16 6.2.5 Interactive Psychiatric Assessment (Use of Equipment) 7 AAC 135.110 (f) .......................... 18 6.3 Clinic Services 6.3.1 Pharmacologic Management 6.3.2 Psychological Testing 7 AAC 135.110 (g) .................................................................................... 18 7 AAC135.100 (b) .......................................................... 14 7 AAC 135.110 .............................................. 15 7 AAC 135.110 (c) ................................................................... 16 7 AAC 135.010. (b) ........................................................................................ 18 6.3.2b Psychologist Services 7 AAC 135.140 .......................................................................... 18 7 AAC 110.550. (b) (5) .................................................................... 19 6.3.3 Psychotherapy ______________________________ 7 AAC 135.150........................................ 19 6.3.4 Short-Term Crisis Intervention 7AAC 135.160 ......................................................................... 20 6.4 Rehabilitation Services .................................................................................................................. 21 6.4.1 Behavioral Health Screening Alaska Screening Tool (AST) 6.4.2 Case Management 6.4.3 Initial Client Status Review (CSR) 7 AAC135.100 (b) ............................................................ 23 6.4.4 Comprehensive Community Support Services for Adults 6.4.5 Daily Behavioral Rehabilitation Services 7 AAC 135.270 ......................................................... 24 7 AAC135.100 (a) ................. 22 7 AAC 135.180, 7 AAC 70.990. (9) Definitions ........................................ 22 7 AAC 135.200 ........................... 23 2 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 6.4.6 Day Treatment Services for Children 7 AAC 135.250 .................................................... 25 6.4.7 Detoxification Services 7 AAC 135.190 ...................................................................................... 25 6.4.8 Requirements for Providing Detoxification Services 7 AAC 70.110 ....................................... 26 6.4.9 Facilitation of a Telemedicine Session 7 AAC 135.290 ............................................................... 29 6.4.10 Medication Administration Services 7 AAC 135.260, 7 AAC 70.990. Definitions. (26) ........ 30 6.4.11 Peer Support Services 7 AAC 135.210 ................................................................. 30 6.4.12 Recipient Support Services 7 AAC 135.230............................................. 31 6.4.13 Residential Substance Use Treatment Services 7 AAC 135.280 ........................ 32 6.4.13b Additional Requirements for Residential Substance Use Services 7 AAC 70.120 ................. 33 6.4.14 Screening, Brief Intervention, and Referral to Treatment (SBIRT) 7 AAC 135.240 .............. 36 6.4.15 Therapeutic Behavioral Health Services for Children 7 AAC 135.220 .................................. 36 6.4.16 Short-Term Crisis Stabilization 7.0 7AAC 135.160 ............................ 37 SERVICE AUTHORIZATION AND LIMITATION 7 AAC 135.040 ..................................... 38 7.1 Service Authorizations................................................................................................................... 38 7.1.1 Service Authorizations for Clinic Services 7 AAC 135.040....................................................... 38 7.1.2 Service Authorization for Rehabilitation Services 7 AAC 135.040 ........................................... 39 7.1.3 Service Authorization Procedures 7.1.4 Out of State Placement Non-State Custody Children (Inpatient Psychiatric) ......................... 40 8.0 7 AAC 135.040 ............................................................ 40 DOCUMENTATION PROCESS STEPS .................................................................................... 41 8.1. Request (Referral) for Services..................................................................................................... 41 8.2 Documentation Process with Alaska Automated Information System (AKAIMS) ................. 41 8.2.1 Admission Including Minimal Data Set Requirements (AKAIMS) .......................................... 41 3 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 8.3 Medicaid and Best Practice Service Documentation Requirements ......................................... 42 8.3.1 Medical Necessity 7 AAC 105 - 7AAC 160 .................................................................................. 42 8.3.2 Assessment ...................................................................................................................................... 42 8.3.3 Treatment Plan............................................................................................................................... 47 8.3.4 Progress Notes (encounter notes, miscellaneous notes, non-episode notes) .............................. 50 8.3.5 Client Status Review (CSR) Process – Treatment Reviews ....................................................... 51 9.0 CIVIL COMMITMENT ............................................................................................................... 54 9.1 Requirements for Civil Commitment........................................................................................... 54 9.1.2 Mental Health Evaluations ........................................................................................................... 54 9.1.3 Definitions ....................................................................................................................................... 55 10.0 INFORMATION RESOURCES ............................................................................................................ 56 10.1 State of Alaska Division of Behavioral Health ............................................................................ 56 10.1.1. New Integrated Behavioral Health Regulations.......................................................................... 56 10.1.2 Division Grantee Providers ........................................................................................................... 56 10.1.3 Review On-Site Provider Training ............................................................................................... 56 10.1.4 Regulation Clarification Process .................................................................................................. 56 10.1.5 Standardized Instrument Resources ............................................................................................ 56 10.1.6 Provider Communications ............................................................................................................ 57 10.1.7 Medical Assistance Billing & Payment ......................................................................................... 57 10.1.8 Alaska Department of Health and Social Services Frequently Asked Questions (FAQs) ...... 57 10.1.10 Regional Providers ..................................................................................................................... 57 10.1.11 Programs ..................................................................................................................................... 58 10.1.12 Statewide Resources (including Statewide Directory for All State Programs) .................. 58 4 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 10.2 Alaska Automated Information System (AKAIMS) .................................................................. 58 10.2.1 https://akaims-support.dhss.alaska.gov/training.htm ................................................................ 58 10.3 All Statutes and Regulations www.legis.state.ak.us/folhome.htm ............................................. 59 10.4 Medicaid Related ........................................................................................................................... 59 10.4.1 XEROX (Affiliated Computer Services, Inc.) ............................................................................. 59 10.4.2 “Forms" Provider Enrollment Application forms...................................................................... 59 10.4.3 “Updates” for Behavioral Health Billing Manual - .................................................................... 59 10.4.4 “Training" View the Training Schedule ...................................................................................... 59 10.4.5 “Contact Us” For Designated Work Units, Staff, Mailing Addresses, etc.- ............................. 59 10.4.6 Keys for Achieving Success in Billing/Payment .......................................................................... 59 11.0 POLICIES AND PROCEDURES .......................................................................................................... 60 11.1 Rural Tribal Providers Boiler Plate Policies and Procedures ................................................... 60 11.1.1 Policies and Procedures List ......................................................................................................... 60 12.0 MEDICAID ENROLLMENT................................................................................................................. 61 12.1 Medicaid Description http://dhss.alaska.gov/dhcs/Pages/medicaid_medicare/default.aspx.... 61 12.2 How to Apply for Medicaid ........................................................................................................... 62 12.2.1 Offices for getting help with Medicaid .......................................................................................... 62 12.2.2 Electronic tracking system ............................................................................................................. 62 13.0 BILLING .................................................................................................................................................. 62 13.1 General Information for Billing ....................................................................................................... 62 13.1.1 Tracking Billing Information Suggestions ................................................................................... 62 5 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 14.0 QUALITY ASSURANCE ....................................................................................................................... 66 14.1 Evaluation Tool .............................................................................................................................. 66 14.2 AKAIMS Reports for Tracking Compliance ............................................................................... 74 14.3 Internal Quality Assurance Process .............................................................................................. 75 14.4 Policy & Procedures Required by Regulation for Quality Assurance ...................................... 75 6 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 1.0 SCOPE The Tribal Health Care Delivery System There are 229 federally recognized tribes in Alaska. The state is divided into 9 health care delivery areas (or service units) – each area is as large as a state in the lower 48 with a low population density, no road systems, extreme weather conditions, and a very high cost of living. In each service unit, the tribes have selected an entity to provide the health care services for the region, although some tribes have chosen to retain provision of local health care services. The tribal health care delivery system is operated under a statewide compact with the federal government authorized under PL 93-638. There are six rural hospitals operated by the tribes, with tertiary care services provided at the Alaska Native Medical Center in Anchorage, which is operated by the Alaska Native Tribal Health Consortium www.anthc.org representing all the tribes. This handbook pertains to all Tribal Rural Behavioral Health Centers in the State of Alaska. In order to become a Tribal Rural Behavioral Health Center (TRBHC) a provider must meet the requirements outlined in 7AAC 70.100. and must remain in compliance with all State of Alaska Division of Behavioral Health Grant requirements and Medicaid regulations. As grantees of the Division of Behavioral Health, all TRBHCs are required to provide services that comply with Medicaid regulations for all clients whether they are Medicaid reimbursable or other type of pay. TRBHC service staff must respond to all persons in apparent need of behavioral health services until the situation is resolved. If it is determined that community-based behavioral health services are not necessary, the behavioral health provider may refer the person to appropriate community resources or to a provider outside of the TRBHCs network for services, if the necessary community services are not available. By July 1, 2015 all TRBHCs must be nationally accredited. You may obtain the general criteria from the matrix provided by the Division of Behavioral Health by using the following Hyperlink to view the provider letter and matrix National Accreditation. You may also view the Division of Behavioral Health training video at National Accreditation & Interim Standards. (The provider information letter referenced in the training video may now be accessed at http://dhss.alaska.gov/dbh/Documents/PDF/Prvdr%20Lttr.(4.29.11)%20N.A.%20and%20Matrix.pdf ) 7 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 2.0 INTRODUCTION This Tribal Rural Provider’s Clinical Handbook is a DRAFT Edition and will be updated with current information on an ongoing basis. Additional Sections added will be based on information provided by the Tribal Rural Providers and the Division of Behavioral Health. This Clinical Handbook is a desk guide provided by the State of Alaska Division of Behavioral Health and is based on the State of Alaska Division of Behavioral Health grant requirements and Medicaid regulations. This document is developed to assist in ensuring consistent, quality behavioral health services delivery and documentation that facilitates compliance with regulations, and maximizes Medicaid billing. This handbook includes Policies and Procedures required by all Tribal Rural Community Behavioral Health Providers and are referred to as “Boilerplate Policies and Procedures (P&Ps)”. Each Provider should include these Boilerplate P&Ps as part of their internally developed Policies and Procedures. This handbook also includes hyperlinks that support the content. For users without access to the internet, additional information required may be obtained from the Division of Behavioral Health upon request. You are encouraged to use the hyperlinks found in the electronic version of this document. The links provide detail and clarification. In order to access a hyperlink, place your cursor over the heading and follow the instructions. Check the “Resources” section of the handbook if the area you are attempting to access does not display a hyperlink. If there is no hyperlink available, you may request the information directly from the Division of Behavioral Health. 3.0 RECIPIENT ELIGIBILITY 3.1 Recipient Eligibility for Medicaid Behavioral Health Services 7 AAC 135.020 3.1.1 Recipient Eligibility Clinic Services The department will pay for behavioral health clinic services for the following individuals only: a child experiencing an emotional disturbance; a child experiencing a severe emotional disturbance; an adult experiencing an emotional disturbance; an adult experiencing a serious mental illness. 3.1.2 Recipient Eligibility Rehabilitation Services The department will pay for behavioral health rehabilitation services for the following individuals only: an individual experiencing a substance use disorder characterized by – a maladaptive pattern of substance use; or – cognitive, behavioral, or physiological symptoms indicating that the individual will continue to use a substance despite significant substance-related problems associated with its use; a child experiencing a severe emotional disturbance; an adult experiencing a serious mental illness. 8 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 3.2. Recipient Eligibility Definitions 3.2.1 Child Experiencing an Emotional Disturbance 7 AAC 70.990. (9) Definitions A recipient is under the age of 21who is experiencing a non-persistent mental, emotional, or behavioral disorder that: is identified and diagnosed during a professional behavioral health assessment; and is not the result of intellectual, physical, or sensory deficits 3.2.2 Adult Experiencing an Emotional Disturbance 7 AAC 70.990. (3) Definitions A recipient is 21 years of age or older who is experiencing a non-persistent mental, emotional, or behavioral disorder that: is identified and diagnosed during a professional behavioral health assessment; and is not the result of intellectual, physical, or sensory deficits 3.2.3 Child or Adult with a Substance Use Disorder 7 AAC 70.990. (31) Definitions A recipient of any age experiencing a diagnosed substance abuse disorder related to: alcohol, amphetamine, or similar acting sympathomimetics; cannabis, cocaine, hallucinogens, inhalants, nicotine, or opioids analogs of phencyclidine (PCP) or similar arylcyclohexylamines; or sedatives, hypnotics, or anxiolytics. 3.2.4 Child Experiencing a Severe Emotional Disturbance (SED) 7 AAC 70.990. (9) Definitions A recipient is under the age of 21who has or at any time in the past year had a diagnosable mental, emotional, or behavioral disorder of sufficient duration to meet diagnostic criteria specified within the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders that has resulted in a functional impairment (a disorder that substantially interferes with or prevents functioning of episodic, recurrent, or continuous duration and not as a result of temporary, expected responses to stressful events in the recipient’s environment) which substantially interferes with or limits the child’s role or functioning (achieving or maintaining the developmentally appropriate social, behavioral, cognitive, communicative or adaptive skills) in family, school, or community activities as indicated by a global assessment of functioning score of 50 or less; Exhibits specific mental, emotional, or behavioral disorders that place the individual at imminent risk for out-of-home placement; place the individual at imminent risk for being placed in the custody of the Division of Juvenile Justice [AS 47.14] have resulted in the individual being placed in the protective custody of Office of Children’s Services [AS 47.10] 9 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 3.2.5 Adult Experiencing a Serious Mental Illness (SMI) 7 AAC 70.990. (2) A recipient is 21 years of age or older who has or at any time in the past year had a diagnosable mental, emotional, or behavioral disorder of sufficient duration to meet diagnostic criteria specified within the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders that has resulted in a functional impairment (a disorder that substantially interferes with or prevents functioning of episodic, recurrent, or continuous duration and not as a result of temporary, expected responses to stressful events in the recipient’s environment) which substantially interferes with or limits one or more life activities, including basic daily living skills, such as personal safety, eating, and personal hygiene; instrumental living skills, such as managing money and negotiating transportation; functioning in social, family, or vocational/educational contexts 4.0 STAFF QUALIFICATIONS 4.1 Staff Behavioral Health Clinical Associate 7 AAC 70.990. (3) Definitions Directing Clinician 7 AAC 70.990. (13) Definitions Mental Health Professional Clinician 7 AAC 70.990. (28) Definitions Peer Support Specialist 7 AAC 135.210 Substance Use Disorder Counselor 7 AAC 70.990. (32) Definitions 4.1.1 Behavioral Health Clinical Associate 7 AAC 70.990. (3) Definitions Behavioral Health Clinical Associate means an individual who may have less than a master's degree in psychology, social work, counseling, or a related field with specialization or experience in providing rehabilitation services to recipients with severe behavioral health conditions; whose responsibilities may include provision of psychosocial evaluation, education related to a recipient's behavioral health condition, encouraging and coaching, counseling, and teaching of needed life skills; and who works within the scope of the individual's training, experience, and education; 4.1.2 Directing Clinician 7 AAC 70.990. (13) Definitions Directing Clinician means a substance use disorder counselor or a mental health professional clinician who, by virtue of that individual's education, training, and experience, and with respect to the recipient's behavioral health treatment plan, develops or oversees the development of the plan; periodically reviews and revises the plan as needed; signs the plan each time a change is made to the plan; and monitors and directs the delivery of all services identified in the plan; NOTE: 4.1.3 By signing a treatment plan, a directing clinician attests that in their professional judgment the services prescribed in the plan are appropriate to the recipient’s needs, delivered at an adequate skill level, and are achieving the treatment goals. Mental Health Professional Clinician 7 AAC 70.990. (28) Definitions 10 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Mental Health Professional Clinician means an individual who is working for a community behavioral health services provider; is performing limited behavioral health services that are within that individual's field of expertise; is not working in a capacity that requires the individual to be licensed under AS 08; and has a master's degree or more advanced degree in psychology, counseling, child guidance, community mental health, marriage and family therapy, social work, or nursing; – a nurse who has a master's degree in nursing; has received special training or experience in mental health; has an active license to practice nursing under AS 08.68; and is working in the individual’s field of expertise; – a marital and family therapist who has an active license to practice marital and family therapy under AS 08.63; and is working in the individual's field of expertise; – a professional counselor who has an active license to practice as a professional counselor under AS 08.29; and is working in the individual's field of expertise; – a social worker who has a master's degree in social work; has an active license to practice as a social worker under AS 08.95; and is working in the individual's field of expertise; or – a psychologist or psychological associate who has an active license to practice as a psychologist or psychological associate under AS 08.86; and is working in the individual's field of expertise; 4.1.4 Peer Support Specialist 7 AAC 135.210 A peer support specialist is a person who: meets all the qualifications of a behavioral health clinical associate (above) is competent to provide peer support services by virtue of having experienced behavioral health issues in self or family is supervised by a mental health professional clinician who the behavioral health services provider has determined is competent to supervise peer support services. Peer support services must be provided by a behavioral health clinical associate who – maintains frequent in-person or telephonic contact with the recipient in order to support the recipient and participate in group activities; – is competent to provide peer support services by virtue of having experienced – behavioral health issues in self or family; and – is supervised by a mental health professional clinician who the community – behavioral health services provider has determined is competent to supervise peer support services by a behavioral health clinical associate. Subject to the limitation in 7 AAC 135.040, peer support services may only be offered in combination with 11 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – individual therapeutic behavioral health services for children under 7 AAC 135.220; – family therapeutic behavioral health services for children under 7 AAC 135.220; or – individual comprehensive community support services under 7 AAC 135.200. 4.1.5 Substance Use Disorder Counselor 7 AAC 70.990. (32) Definitions Substance Use Disorder Counselor means an individual who, subject to the limits of the individual's education, training and experience, provides behavioral health rehabilitation services with a focus on the treatment of substance use disorders, while working for a community behavioral health services provider; 5.0 Clinical Record Requirements 5.1 7 AAC 105.230. Requirements for provider records (a) A provider shall maintain accurate financial, clinical, and other records necessary to support the services for which the provider requests payment. The provider shall ensure that the provider's staff, billing agent, or other entity responsible for the maintenance of the provider's financial, clinical, and other records meets the requirements of this section. (b) A provider's record must identify recipient information for each recipient including the name of the recipient receiving treatment; specific services provided; extent of each service provided; date on which each service was provided; and individual who provided each service. (c) A provider's record must identify financial information for each recipient including the charge for each service provided; each payment source pursued; the date and amount of all debit and credit billing actions for each date of service provided; and (the amounts billed and paid. (d) A provider shall maintain a clinical record, including a record of therapeutic services, in accordance with professional standards applicable to the provider, for each recipient. The clinical record must include information that identifies the recipient's diagnosis; information that identifies the medical need for each service; identification of each service, prescription, supply, or plan of care prescribed by the provider; identification of prescription drugs dispensed in accordance with 7 AAC 120.100 - 7 AAC 120.140; stop and start times for time-based billing codes; and annotated case notes identifying each service or supply delivered; the case notes must be dated and either signed or initialed by the individual who provided each service. 12 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (e) A provider shall retain a recipient's records described in (b) - (d) of this section for which services have been billed to the department for at least seven years from the date the service is provided. The duty of the provider set out in this subsection applies to a provider even if the provider's business is sold or transferred, or is no longer operating. If a provider ceases business, the provider shall notify the department how the department can access Medicaid recipient records in the future. (f) A provider who maintains all or part of the provider's records in an electronic format shall ensure that the data required to be maintained by this section is readily accessible as required under 7 AAC 105.240(a) 5.2 7 AAC 135.130. Clinical record (a) To be eligible for payment under this chapter, a community behavioral health services provider, mental health physician clinic, or psychologist enrolled under 7 AAC 135.030(a) (3), must maintain, for each recipient served, a clinical record that includes the following: if the provider is a community behavioral health services provider, a completed behavioral health screening that meets the requirements of 7 AAC 135.100 using the Alaska Screening Tool, adopted by reference under 7 AAC 160.900; if the provider is a community behavioral health services provider, a client status review that meets the requirements of 7 AAC 135.100, unless the services provided to the recipient are limited to – (A) detoxification services under 7 AAC 70.110 and 7 AAC 135.190; – (B) short-term crisis intervention services under 7 AAC 135.160; or – (C) short-term crisis stabilization services under 7 AAC 135.170; (3) if a mental health intake assessment is provided under 7 AAC 135.110, a written report that documents – (A) a complete diagnosis consistent with the multi-axial classification system used in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, adopted by reference in 7 AAC 160.900, if a diagnosis exists; – (B) the problems identified during the professional behavioral health assessment and client status review processes, including functional deficits that require mental health treatment; and – (C) treatment recommendations; (4) if a substance use intake assessment is provided under 7 AAC 135.110, a written report that documents – (A) a diagnosis of the substance use disorder, if a diagnosis exists; – (B) the problems identified during the professional behavioral health assessment and client status review processes; and – (C) treatment recommendations; (5) if an integrated mental health and substance use intake assessment is provided under 7 AAC 135.110, a written report with the information required under (3) and (4) of this subsection; 13 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 6.0 SERVICE REQUIREMENTS 6.1 Initial Services Initial services are those that may be provided to any Medicaid-eligible recipient and include the following services. Behavioral Health Screening 7 AAC 135.100 Initial Client Status Review (CSR) 7 AAC 135.100 Screening and Brief Intervention Services 7 AAC 135.240 6.1.1 Behavioral Health Screening Alaska Screening Tool (AST) 7 AAC 135.100 The AST is the tool authorized and produced by the Department of Health & Social Services to be used to initially screen potential recipients to determine the likelihood that a mental health condition, substance use disorder, or brain injury is present. The AST is the point of entry to a community behavioral health program and assists with determining the appropriate assessments needed to identify the recipient’s treatment needs. This service is administered using the AST form adopted by reference. Alaska Screening Tool (AST) which is a required service for all new and returning recipients. These services may be rendered by a member of the provider’s staff who is performing the service as a regular duty within the scope of that staff member’s knowledge, experience, and education. 6.1.2 Client Status Review (CSR) Initial 7 AAC135.100 (b) This service is rendered by a member of the provider’s staff who is performing this service as a regular duty within the scope of that staff member’s knowledge, experience, and education. The client status review means an evaluation to measure a recipient’s quality of life at the time of intake and at subsequent intervals during treatment or recovery, and at discharge. The service is administered using the Client Status Review form (CSR) adopted by reference. Must be completed for any new or returning recipient and used as relevant clinical information concurrent with an initial professional behavioral health assessment. A client status review must be completed with the recipient present and is required to be: – administered using the CSR or an electronic version of that form by means of the Alaska Automated Information Management System (AKAIMS); – used to assist in determining a recipient’s functioning in the life areas identified on the form; – used by the directing clinician to assist in measuring the outcomes of behavioral health treatment provided; – used by the directing clinician in making treatment decisions; and – used by the directing clinician to revise the recipient’s behavioral health treatment plan. – administered and reviewed every 90 to 135 days while the recipient is in treatment or from the date the treatment plan was last reviewed, and again at discharge from treatment. 6.1.3 Screening, Brief Intervention, and Referral to Treatment (SBIRT) 7 AAC 135.240 SBIRT is a comprehensive, integrated, public health approach to the delivery of early intervention and treatment services for persons with substance use disorders as well as those who are at risk of developing these disorders. Primary care centers, hospital emergency rooms, trauma centers, and 14 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 other community settings provide opportunities for emergency intervention with at-risk substance users before more severe consequences occur. The service includes: Screening - use of self-report questionnaires or structured interviews or similar screening techniques to detect substance use problems; identify the degree to which a person is at risk, and to identify the appropriate level of intervention as results indicate. Brief Intervention - based on results of screening, if necessary, use of motivational discussion focused on raising a person’s awareness of their substance use, the potential harmful effects of that use, and encouraging positive change. Brief Intervention services may include: – feedback – goal setting – coping strategies – identification of risk factors – information – advice Referral to Treatment – if the screening reveals that the recipient meets any of the circumstances identified below, the community behavioral health services provider will refer the recipient to a behavioral health treatment program that will meet their needs – is at severe risk of substance use problems – is already substance dependent – has already received brief intervention or treatment for substance abuse and was nonresponsive – exhibits symptoms of an emotional disorder (Based on SBIRT screening tool) Delivery of screening and brief intervention services does not require an intake assessment or behavioral health treatment plan. 6.2 Professional Behavioral Health Assessments 7 AAC 135.110 If a behavioral health screening conducted under 7 AAC 135.100, or a referral by a court or other agency, has identified an individual who is suspected of having a behavioral health disorder that could require behavioral health services, the department will pay a community behavioral health services provider for the following assessment services: a mental health intake assessment 7 AAC 135.110(b) a substance use intake assessment 7 AAC 135.110 (c) an integrated mental health and substance use intake assessment 7 AAC 135.110 (d) a psychiatric assessment 7 AAC 135.110(e) interactive psychiatric assessment 7 AAC 135.110 (f) The first behavioral health service following the initial assessment may be another assessment service, if determined by the clinician/counselor to be the most appropriate service. I.e. persons being treated or determined to be in need of psychotropic medications may need an appointment with an individual qualified to prescribe psychotropic medications. 6.2.1 Mental Health Assessment 7 AAC 135.110 (b) To qualify for payment, a mental health intake assessment must be documented in the recipient's clinical record in accordance with 7 AAC 105.230 and 7 AAC 135.130; 15 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 conducted in accordance with the requirements of 7 AAC 135.010(b)(1), if the provider is a community behavioral health services provider; conducted by a qualified staff (mental health professional clinician at a minimum) upon admission to services and during the course of active treatment as necessary, for the purpose of determining and documenting – the recipient's mental status and social and medical history; – the nature and severity of any identified mental health disorder; – contain a complete diagnosis consistent with the multi-axial classification system used in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, adopted by reference in 7 AAC 160.900; – treatment recommendations that form the basis of a subsequent behavioral health treatment plan; and – functional impairment; and updated as new information becomes available. NOTE: 7 AAC 135.130. The clinical record must document the problems identified during the professional behavioral health assessment and client status review processes, including functional deficits that require mental health treatment. 6.2.2 Substance Abuse Assessment 7 AAC 135.110 (c) To qualify for payment, a substance use intake assessment must be documented in the recipient's clinical record in accordance with 7 AAC 105.230 and 7 AAC 135.130; conducted by a substance use disorder counselor, social worker, or other qualified program staff member performing duties regularly within the scope of the individual's authority, training, and job description; however, if the substance use intake assessment is conducted as part of detoxification services subject to 7 AAC 70.110 and 7 AAC 135.190, the assessment must be conducted by an individual identified in 7 AAC 70.110 for the type of detoxification service provided; conducted upon admission to services and during the course of active treatment as necessary, for the purpose of determining and documenting – if the recipient has a substance use disorder; – the nature and severity of any identified substance use disorder; – the correct diagnosis; – treatment recommendations that form the basis of a subsequent behavioral health treatment plan; and – functional impairment; and updated as new information becomes available. 6.2.3 Integrated Mental Health and Substance Abuse Assessment 7 AAC 135.110 (d) To qualify for payment, a mental health intake assessment must be documented in the recipient's clinical record in accordance with 7 AAC 105.230 and 7 AAC 135.130; conducted by qualified staff in accordance with the requirements of 7 AAC 135.010(b)(1), if the provider is a community behavioral health services provider; 16 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 NOTE: 6.2.4 conducted upon admission to services and during the course of active treatment as necessary, for the purpose of determining and documenting – the recipient's mental status and social and medical history; – the nature and severity of any identified mental health disorder; – if the recipient has a substance use disorder; – the nature and severity of any identified substance use disorder; – the correct diagnosis; – a complete diagnosis consistent with the multi-axial classification system used in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, adopted by reference in 7 AAC 160.900; – functional impairment; – and treatment recommendations that form the basis of a subsequent behavioral health treatment plan; and updated as new information becomes available. 7 AAC 135.130. The clinical record must document the problems identified during the professional behavioral health assessment and client status review processes, including functional deficits that require behavioral health treatment. Psychiatric Assessment 7 AAC 135.110 (e) The department will pay a community behavioral health services provider or mental health physician clinic for a psychiatric assessment interview that is to serve as the professional behavioral health assessment, if the recipient's condition indicates the need for a more intensive assessment, including an assessment to evaluate the need for medication. A psychiatric assessment interview must be conducted by a professional described in 7 AAC 135.010(b) (2); include a review of any general medical and psychiatric history or problem the recipient is presenting; include a relevant recipient history; include a mental status examination; result in a complete diagnosis consistent with the multi-axial classification system used in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, adopted by reference in 7 AAC 160.900; and include a listing of any identified psychiatric problems, including functional impairments, with treatment recommendations. 17 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 6.2.5 Interactive Psychiatric Assessment (Use of Equipment) 7 AAC 135.110 (f) The department will pay a community behavioral health services provider or mental health physician clinic for an interactive psychiatric assessment using equipment and devices that is to serve as the professional behavioral health assessment, if the recipient’s condition indicates the need for a more intensive assessment including an assessment to evaluate the need for medication. An interactive psychiatric assessment using equipment and devices must be conducted by a professional described in 7 AAC 135.010(b)(2); include a review of any general medical and psychiatric history or problem the recipient is presenting; include a relevant recipient history; include a mental status examination; result in a complete diagnosis consistent with the multi-axial classification system used in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, adopted by reference in 7 AAC 160.900; and include a listing of any identified psychiatric problems, including functional impairments, with treatment recommendations. 6.3 Clinic Services 7 AAC 135.010. (b) Clinic services must be performed by a staff who is a physician, physician assistant, advanced nurse practitioner, or mental health professional clinician and who is performing the service within the scope of their knowledge, experience, and education: Pharmacologic Management Services 7 AAC 135.14 Psychological Testing 7 AAC 135.110 (g) Psychotherapy 7 AAC 135.150 Short-Term Crisis Intervention Services 7 AAC 135.160 6.3.1 Pharmacologic Management 7 AAC 135.140 The department will pay a community behavioral health services provider or mental health physician clinic for a pharmacologic management service if that service is provided directly by a professional described in 7 AAC 135.010(b) (2). To qualify for payment under this section, a provider must monitor a recipient for the purposes of assessing a recipient's need for pharmacotherapy; prescribing appropriate medications to meet the recipient's need; and monitoring the recipient's response to medication, including – documenting medication compliance; – assessing and documenting side effects; and – evaluating and documenting the effectiveness of the medication. 6.3.2 Psychological Testing 7 AAC 135.110 (g) The department will pay a community behavioral health services provider, mental health physician clinic, or psychologist for psychological testing and evaluation to assist in the diagnosis and treatment of mental and emotional disorders. Psychological testing and evaluation includes the assessment of functional capabilities, the administration of standardized psychological tests, and the interpretation of findings, and must be conducted in accordance with 18 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 the requirements of 7 AAC 135.010(b)(1), if the provider is a community behavioral health services provider; the requirements of 7 AAC 135.030(d) and (e), if the provider is a mental health physician clinic; the requirements of 7 AAC 135.030(a), if the provider is a psychologist. If the provider is a community behavioral health services provider, the individual who conducts a professional behavioral health assessment under this section shall document in the written assessment that the results of the behavioral health screening, conducted under 7 AAC 135.100 using the Alaska Screening Tool, adopted by reference under 7 AAC 160.900, were reviewed and considered during the assessment. 6.3.2b Psychologist Services 7 AAC 110.550. (b) (5) To be eligible for payment under 7 AAC 105 - 7 AAC 160 for providing psychologist services, a provider must be an independently practicing psychologist who – is enrolled as a psychologist in accordance with 7 AAC 105.210; – has an active license to practice psychology issued by the jurisdiction in which the psychologist provides services; if services are provided in this state, the psychologist must hold an active license under AS 08.86.130 or 08.86.135; and – maintains records in accordance with (e) of this section. Covered psychologist services are limited to medically necessary psychological testing to determine the status of the patient's mental, intellectual, and emotional functioning. Testing services must include administration of psych diagnostic tests, the interpretation of the results of the tests, and a written report. Testing services must be provided directly by the psychologist. Payment is limited to the following services: – psychological testing; – assessment of aphasia; – developmental testing, limited or extended; – neurobehavioral status examination, including assessment of thinking, reasoning, and judgment; – neuropsychological testing. Psychologist services may be provided to a recipient who has received a referral from the recipient's treating physician, a physician assistant, an advanced nurse practitioner, a community mental health clinic, a tribal health program, or an appropriate school official, if the referral documents the purpose for the testing, including the need to determine acuity of need, severity of symptoms, or level of impairment. 6.3.3 Psychotherapy ______________________________ 7 AAC 135.150 The department will pay a community behavioral health services provider or mental health physician clinic for one or more of the following forms of psychotherapy, as coded in Current Procedural Terminology (CPT), adopted by reference in 7 AAC 160.900: insight-oriented individual psychotherapy; interactive individual psychotherapy (i.e. play therapy); group psychotherapy; family psychotherapy - without recipient;** 19 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 family psychotherapy - with recipient;** multi-family group psychotherapy Biofeedback or relaxation therapy may be provided as an element of insight-oriented individual psychotherapy and interactive individual psychotherapy if that biofeedback or relaxation therapy is prescribed by a psychiatrist, if provided in a mental health physician clinic; prescribed by a physician or ordered by a mental health professional clinician, if provided at a community behavioral health services provider; and included in the behavioral health treatment plan as a recognized treatment or adjunct to a treatment only for the following conditions or substantially similar conditions: – chronic pain syndrome; – panic disorders; – phobias ** Family psychotherapy, with or without recipient involvement, may be provided telephonically if the service could not otherwise be provided; and the provider documents, in the recipient's treatment note for each session, the reason that family psychotherapy was provided telephonically 6.3.4 Short-Term Crisis Intervention 7AAC 135.160 The department will pay a community behavioral health services provider for short-term crisis intervention services, provided by a mental health professional clinician to a recipient, if that mental health professional clinician provides an initial assessment of the nature of the short-term crisis; recipient's mental, emotional, and behavioral status; and recipient's overall functioning in relation to the short-term crisis. The mental health professional clinician may order and deliver, as a crisis intervention service, any medically necessary and clinically appropriate behavioral health clinic or rehabilitation service or intervention in accordance with 7 AAC 135.010 that is included in the crisis plan to reduce the symptoms of the acute mental, emotional, or behavioral disorder; prevent harm to the recipient or others; prevent further relapse or deterioration of the recipient's condition; or stabilize the recipient within the family system, if one exists. Short-term crisis intervention includes the following treatment and supports: individual or family psychotherapy needed in response to the short-term crisis; individual or family training and education related to resolving the existing short-term crisis and preventing a future crisis; monitoring the recipient for safety purposes. The mental health professional clinician is responsible for planning all behavioral health services needed to respond to the short-term crisis; writing the short-term crisis intervention plan that contains – treatment goals derived from the crisis assessment; and 20 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – a description of the medically necessary and clinically appropriate services provided under this chapter that the recipient requires to resolve the existing short-term crisis; and – directing all services that are ordered in the short-term crisis intervention plan except for pharmacologic management services. The department will separately pay a community behavioral health services provider for pharmacologic management services provided in accordance with 7 AAC 135.010(b)(2) and for the behavioral health clinic and rehabilitation services and interventions ordered and delivered under a short-term crisis intervention plan developed if the bill for each service is separately submitted to the department. Notwithstanding any behavioral health treatment plan in effect for the recipient at the onset of a short-term crisis, if a recipient is receiving short-term crisis intervention services, the department will only pay for the behavioral health services identified in the short-term crisis intervention plan for the duration of the short-term crisis intervention service. short-term crisis intervention must be documented on a contact form provided by the department. The services that are ordered by the mental health professional clinician in the short-term crisis intervention plan, but provided by others, must be documented by the individual who provides the service. All documentation under this subsection must be filed in the recipient's clinical record. Short-term crisis intervention may be provided in any appropriate outpatient or community setting, including a hospital emergency room, if the recipient has not been admitted to the hospital; a facility designated for crisis respite purposes; and the recipient's place of residence, workplace, or school. NOTE: 6.4 The crisis intervention/stabilization form can be obtained at the following website: Alaska Department of Health & Social Services, Division of Behavioral Health. Provider Information can be located at: http://hss.alaska.gov/dbh/. From the website, select “Use this link for New Integrated Behavioral Health Regulations Implementation”. The Crisis Intervention/Stabilization Form (Word) and (PDF) is found under “Resources”. Rehabilitation Services Rehabilitation services are provided reduce the effects of behavioral health disorders and to increase the recipient’s ability to function within their home, school and community. Services may be provided on the premises of a CBHS provider, in the recipient’s home, or any community setting appropriate for providing the services as specified in the recipient’s behavioral health treatment plan. The clinical record must document the problems identified during the professional behavioral health assessment and client status review processes, including functional deficits that require mental health rehabilitation services At a minimum you must be a Behavioral Health Clinical Associate or Substance Use Disorder Counselor. 21 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 The department will pay for the following behavioral health rehabilitation services if the service is provided by a member of the provider's staff who is performing that service as a regular duty within the scope of that staff member's knowledge, experience, and education: Behavioral health screening; client status review. 7 AAC 135.100 Case management 7 AAC 135.180 Client Status Review 7 AAC135.100 (b) Comprehensive community support services for adults 7 AAC 135.200 Daily behavioral rehabilitation services. 7 AAC 135.270 Day treatment services for children. 7 AAC 135.250 Detoxification services. 7 AAC 135.190 Facilitation of a telemedicine session. 7 AAC 135.290 Medication administration services 7 AAC 135.260. Peer support services. 7 AAC 135.210 Recipient support services 7 AAC 135.230 Residential substance use treatment services. 7 AAC 135.280 Screening and brief intervention services. 7 AAC 135.240 Therapeutic behavioral health services for children. 7 AAC 135.220 Short-term crisis stabilization services. 7 AAC 135.170 6.4.1 Behavioral Health Screening Alaska Screening Tool (AST) 7 AAC135.100 (a) The AST is the tool authorized and produced by the Department of Health & Social Services to be used at the initial screening of potential recipients to determine the likelihood that a mental health condition, substance use disorder, or brain injury is present. The AST is the point of entry to a community behavioral health program and assists with determining the appropriate assessments needed to identify the recipient’s treatment needs. This service is administered using the AST form adopted by reference. Alaska Screening Tool (AST) is a required service for all new and returning recipients. These services may be rendered by a member of the provider’s staff who is performing the service as a regular duty within the scope of that staff member’s knowledge, experience, and education. 6.4.2 Case Management 7 AAC 135.180, 7 AAC 70.990. (9) Definitions The department will pay a community behavioral health services provider for case management provided to a recipient or recipient's family for one or more of the following purposes only: coordinating assessments, treatment planning, and service delivery; providing linkage between the recipient and other needed services; monitoring, by direct observation by the directing clinician, the delivery of behavioral health services other than case management as those services are provided to the recipient to ensure that interventions and techniques are – appropriate to the recipient's needs; – delivered at an adequate skill level; and – achieving the treatment goals; providing advocacy and support to the parents and the foster parents of a child in foster care to preserve the placement; providing overall advocacy and support for the recipient's social, educational, legal, and treatment needs. 22 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 The department will pay only one case manager of a child experiencing a severe emotional disturbance for time setting up, traveling to or from, and attending a treatment team meeting conducted under 7 AAC 135.120 for that recipient. – Except as provided in (b) of this section, the department will not pay a member of a treatment team for – travel to or from a meeting; – time spent in or preparing for a meeting; – serving as a member of a treatment team; or – writing or monitoring a behavioral health treatment plan. The department will not pay for case management if it is provided by a family member or foster parent of the recipient. Case management may be provided within the home, workplace, school, or any other appropriate community setting. Case management does not require the recipient to be present and may be provided at the same time the recipient is being provided another service. – "Case management" means assistance to the recipient and the recipient's family in accessing and coordinating high-quality needed services, including – medical, psychiatric, and mental health services; – substance use treatment; – educational, vocational, and social supports; and – community-based services, related assessments, and post-discharge follow-up activities; 6.4.3 Initial Client Status Review (CSR) 7 AAC135.100 (b) This service is rendered by a member of the provider’s staff who is performing this service as a regular duty within the scope of that staff member’s knowledge, experience, and education. The client status review means an evaluation to measure a recipient’s quality of life at the time of intake and at subsequent intervals during treatment or recovery, and at discharge. The service is administered using the Client Status Review form (CSR) adopted by reference. Must be completed for any new or returning recipient and used as relevant clinical information concurrent with an initial professional behavioral health assessment. A client status review must be completed with the recipient present and is required to be: – administered using the CSR or an electronic version of that form by means of the Alaska Automated Information Management System (AKAIMS); – used to assist in determining a recipient’s functioning in the life areas identified on the form; – used by the directing clinician to assist in measuring the outcomes of behavioral health treatment provided; – used by the directing clinician in making treatment decisions; and – used by the directing clinician to revise the recipient’s behavioral health treatment plan. – administered and reviewed every 90 to 135 days while the recipient is in treatment or from the date the treatment plan was last reviewed, and again at discharge from treatment. 6.4.4 Comprehensive Community Support Services for Adults 7 AAC 135.200 23 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 The department will pay a community behavioral health services provider for comprehensive community support services, for a recipient 21 years of age or older except as provided in 7 AAC 135.020(d) , if those services promote wellness, recovery, and resiliency; improve the recipient's overall functioning; assist the recipient to be successful with illness self-management; restore the recipient's capacity for more effective daily functioning and reduce the likelihood of institutionalization or institution-based care; help the recipient develop, maintain, or improve specific self-care, self-direction, communication, and social behavior; restore the recipient's ability to engage in normal, age-appropriate daily activities that may include the use of stores, restaurants, churches, recreational facilities, public transportation, and workplaces; or restore the behavioral, emotional, or intellectual skills necessary to live, learn, or work productively in the recipient's environment, including the following activities of daily living: – obtaining and remembering to take prescribed medication; – making appointments for health care or other needs; – arranging for transportation to and from appointments; – budgeting, meal planning, and grocery shopping; – choosing safe friends; – developing appropriate social relationships; – other daily living responsibilities associated with being a fully functioning adult. Comprehensive community support services may be provided – on the premises of the community behavioral health services provider, the recipient's residence, the recipient's workplace, or any other appropriate community setting; – to an individual or a group. Comprehensive community support services are limited to the following: – teaching of life skills designed to restore the recipient's functioning; – counseling focused on functional improvement, recovery, and relapse prevention; – encouraging and coaching. 6.4.5 Daily Behavioral Rehabilitation Services 7 AAC 135.270 The department will pay a community behavioral health services provider for daily behavioral rehabilitation services provided to a recipient who resides in a foster home or residential setting that is licensed under 7 AAC 50.005 - 7 AAC 50.790 or 7 AAC 56 if those services are provided in accordance with 7 AAC 135.020(b) to a recipient who is a child experiencing a severe emotional disturbance, and for the purpose of improving the recipient's overall functioning and reducing the likelihood of – the recipient's failure in a school setting; – longer term separation from the recipient's family; or – referral of the recipient to more restrictive institutional care; promoting the recipient's wellness, recovery, and resiliency; helping the recipient – develop or improve specific age-appropriate social behavior; – develop or improve self-management skills that will support overall success; and 24 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – make better behavioral choices within the recipient's family, school, and community; assisting the recipient in developing strategies for transitioning into adulthood, including planning for continued education or employment. To qualify as a daily behavioral rehabilitation service, the service must provide safety, structure, supervision, and at least two of the following types of active treatment each day: – teaching of life skills designed to restore the recipient's functioning; – counseling focused on functional improvement, recovery, and relapse prevention; – encouraging and coaching. The department will not pay for the daily supervisory activities provided in a licensed foster home or licensed residential setting that a parent or foster parent would normally carry out to assure protection, emotional support, and care of a child who is not a child experiencing a severe emotional disturbance. Except for FASD/SED waiver services provided under 7 AAC 130.100 - 7 AAC 130.199, the department will not pay a community behavioral health services provider for any other behavioral health service provided by the recipient's foster parent on the same day, including residential behavioral rehabilitation services under 7 AAC 135.800. 6.4.6 6.4.7 Day Treatment Services for Children 7 AAC 135.250 The department will pay a community behavioral health services provider for day treatment services for children provided in the school setting if those services are provided to a recipient who is a child experiencing a severe emotional disturbance; promote the recipient's ability to be successful, independent of behavioral health services, in the community-based school environment; and assist the recipient in developing self-management skills consistent with academic progress. Day treatment services for children are provided – on the school premises; – on days that the recipient's school is in session; – as group treatment; and – by an individual who delivers rehabilitation services within the educational setting led by a teacher. Day treatment services for children are limited to the following forms of active treatment: – teaching self-management skills designed to improve the recipient's academic and behavioral functioning; – counseling focused on overall functional improvement in the school setting; – encouraging and coaching to achieve academic and behavioral success in school. The community behavioral health services provider providing day treatment services must establish with the local school district a written agreement that specifies the overall goals of the collaborative effort, guidelines for meeting the criteria for services, roles and responsibilities of the parties to the agreement, and the resources, including personnel, contributed by each of the parties to the agreement. The department will not pay for day treatment services if those services are delivered by the teacher providing the academic program. Detoxification Services 7 AAC 135.190 25 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 The department will pay a community behavioral health services provider for the following alcohol and drug detoxification services delivered face-to-face to the recipient: ambulatory detoxification with extended on-site monitoring provided in accordance with 7 AAC 70.110; clinically managed residential detoxification provided in accordance with 7 AAC 70.110; medically monitored residential detoxification provided in accordance with 7 AAC 70.110. The only behavioral health services that the department will pay for when provided on the same day as alcohol and drug detoxification services are behavioral health screening under 7 AAC 135.100; needed professional behavioral health assessments under 7 AAC 135.110; case management services under 7 AAC 135.180; needed behavioral health clinic services under 7 AAC 135.010; a medical evaluation 6.4.8 Requirements for Providing Detoxification Services 7 AAC 70.110 The department will approve a community behavioral health services provider that meets the requirements of this section to provide one or more of the following alcohol and drug detoxification services: ambulatory detoxification with extended on-site monitoring; clinically managed residential detoxification; medically monitored residential detoxification. Ambulatory detoxification with extended on-site monitoring must – be delivered as an outpatient service on the premises of the community behavioral health services provider; – include 24-hour access to medical consultation and emergency medical care in a general acute care hospital; – include periodic evaluation of the recipient's condition and treatment to confirm that ambulatory detoxification with extended on-site monitoring continues to be safe for the recipient; – be provided directly to a recipient by an individual with an active license under AS 08 to practice as a physician; a physician assistant; an advanced nurse practitioner; a registered nurse supervised by a physician or advanced nurse practitioner; or a licensed practical nurse supervised by a physician or advanced nurse practitioner; and – include, at admission and during the course of active treatment as needed, a substance use intake assessment conducted in accordance with 7 AAC 135.110(c) ; a medical evaluation; of the individuals listed in (4) of this subsection, only a physician, physician assistant, or advanced nurse practitioner may provide a medical evaluation; monitoring, assessment, and management of intoxication; and evaluating a recipient's withdrawal by applying the Revised Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWA-Ar) or Clinical Opiate Withdrawal Scale (COWS), adopted by reference in 7 AAC 70.910; and 26 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – include at least three of the component services listed in this section. Clinically managed residential detoxification must – be delivered as a residential service on the premises of the community behavioral health services provider; – include 24-hour access to medical consultation and care; – be provided directly to a recipient by a substance use disorder counselor; a behavioral health clinical associate; a mental health professional clinician; or an individual with an active license under AS 08 to practice as (i) a physician; (ii) a physician assistant; (iii) an advanced nurse practitioner; (iv) a registered nurse supervised by a physician or advanced nurse practitioner; or (v) a licensed practical nurse supervised by a physician or advanced nurse practitioner; – include at least three of the component services listed in this section; if the component services include medication administration services, and of the medically monitored residential detoxification individuals listed in this subsection, only a physician, a physician assistant, an advanced nurse practitioner, a registered nurse supervised by a physician or advanced nurse practitioner, or a licensed practical nurse supervised by a physician or advanced nurse practitioner may provide medication administration services; – include a substance use intake assessment, at admission and during the course of active treatment as needed, and conducted in accordance with 7 AAC 135.110(c) ; and – include a medical evaluation; of the medically monitored residential detoxification individuals listed in this subsection, only a physician, physician assistant, or advanced nurse practitioner may provide a medical evaluation. Medically monitored residential detoxification must – be delivered as a residential service on the premises of the community behavioral health services provider; – include medical consultation available daily by telephone 24 hours per day; – be provided directly to a recipient by an individual with an active license under AS 08 to practice as a physician; a physician assistant; an advanced nurse practitioner; a registered nurse supervised by a physician or advanced nurse practitioner; or a licensed practical nurse supervised by a physician or advanced nurse practitioner; – include, no later than 24 hours after admission, and during the course of active treatment as needed, a medical evaluation; of the medically monitored residential detoxification individuals listed in this subsection, only a physician, physician assistant, or advanced nurse practitioner may provide a medical evaluation; if methadone is used in treatment, a physician must perform a reevaluation no later than 24 hours after admission; – include daily monitoring of each recipient on the premises; of the medically monitored residential detoxification individuals listed in this subsection, only a physician, physician assistant, or advanced nurse practitioner may perform that daily monitoring; 27 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – include, if medically necessary and clinically appropriate, hourly monitoring 24 hours per day of a recipient's medication administration and progress; – include, at admission and during the course of active treatment as needed, a substance use intake assessment conducted in accordance with 7 AAC 135.110(c) ; the following services performed by a nurse: (i) monitoring, assessment, and management of intoxication; (ii) evaluation of a recipient's withdrawal by applying the Revised Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWA-Ar) or Clinical Opiate Withdrawal Scale (COWS), adopted by reference in 7 AAC 70.910; and medically supervised evaluation and consultation available 24 hours per day; and – include at least three of the component services listed in this section. Ambulatory detoxification with extended on-site monitoring, clinically managed residential detoxification, and medically monitored residential detoxification must include at least three of the following component services: – medication administration services; – referrals to other behavioral, medical, social, or educational agencies, as needed; – discharge or transfer planning; – evaluation and treatment of symptoms of intoxication and withdrawal; – comprehensive community support services; – crisis or relapse prevention planning; – individual daily assessment; – case management; – management of a recipient's chronic disease, if medically necessary and clinically appropriate; – urinalysis and breathalyzer testing, when specifically related to detoxification; – development of coping skills in the recovery environment. Each employee of a community behavioral health services provider who provides detoxification services directly to a recipient must – be currently certified by the American Red Cross, or other certifying organization, in cardiopulmonary resuscitation; basic first aid; and blood-borne and airborne pathogens; – work within the scope of that employee's education, training, license, credentials, and experience; – work under the supervision of a physician, a physician assistant, or an advanced nurse practitioner, if the employee is not a physician, a physician assistant, or an advanced nurse practitioner; – be capable of implementing (i) physician-approved protocols for observation and supervision; and (ii) protocols for medical intervention and crisis management developed by the provider under (g) of this section; assisting in the determination of an appropriate level of care and in transitioning the recipient to that level of care; 28 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 monitoring, identifying, treating, or assisting with the treatment of symptoms of intoxication or withdrawal from alcohol or drugs using the assessment materials listed at the bottom of this section; following provider protocol on when to seek medical care for any symptom or treatment need of a recipient; observing a recipient self-administer medication and verifying that self-administration was done in accordance with the physician's prescription and all other laws, policies, and procedures; and monitoring a recipient's stabilized behavioral health problems and recognizing instability in a recipient with co-occurring disorders. To be approved to provide any service under this section, a community behavioral health services provider must establish a – protocol for determining when and what kind of medical intervention may be needed, including nursing or physician care; emergency procedures; and transferring a recipient to a higher level of care; and – crisis management protocol and train staff in using that protocol. All detoxification services must be medically necessary and clinically appropriate in accordance with the – ASAM Patient Placement Criteria for the Treatment of Substance-Related Disorders, adopted by reference in 7 AAC 70.910; – Diagnostic and Statistical Manual of Mental Disorders, adopted by reference in 7 AAC 70.910; – Revised Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWA-Ar), adopted by reference in 7 AAC 70.910; and – Clinical Opiate Withdrawal Scale (COWS), adopted by reference in 7 AAC 70.910. In this section, "individual daily assessment" means the ongoing daily process of collecting information regarding the recipient's treatment needs, preferences, and desired outcomes. 6.4.9 Facilitation of a Telemedicine Session 7 AAC 135.290 Facilitation of telemedicine is the combination of activities necessary to establish and maintain electronic connectivity via telemedicine communication equipment for the purposes of securing needed treatment for an eligible recipient by a qualified treating provider in another location. The department will pay a community behavioral health services provider for facilitation of a telemedicine session if the facilitating provider ensures all of the following conditions are met: – the telemedicine communication equipment is supplied by the provider – the electronic connection used by the treating provider and the recipient are established and maintained by the provider – the provider remains available during the telemedicine session to reestablish failed connection before the intended end of the telemedicine session – the provider documents the recipient’s clinical record a note summarizing the facilitation of each telemedicine session (although the facilitating provider is not required to document a clinical problem or treatment goal as these are to be documented by the treating provider) This service may be rendered to eligible recipients meeting the following criteria 29 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – child or adult experiencing a substance use disorder – child experiencing a severe emotional disturbance – adult experiencing a serious mental illness This service is rendered by a member of the provider’s staff who is performing this service as a regular duty within the scope of that staff member’s knowledge, experience, and education. 6.4.10 Medication Administration Services 7 AAC 135.260, 7 AAC 70.990. Definitions. (26) The department will pay a community behavioral health services provider for on-premises medication administration services provided to a recipient on the premises of the community behavioral health services provider. The department will pay a community behavioral health services provider for off-premises medication administration services provided to a recipient at home, school, or any other appropriate community setting. (26) "medication administration services" means the administration, by medical personnel, of injectable or oral medications to a recipient, documentation of medication compliance, assessment and documentation of side effects, and evaluation and documentation regarding the effectiveness of the medication; in this paragraph, "medical personnel" means – a physician; – a physician assistant; – an advanced nurse practitioner; – a registered nurse supervised by a physician or advanced nurse practitioner; – a licensed practical nurse supervised by a physician or advanced nurse practitioner; 6.4.11 Peer Support Services 7 AAC 135.210 The department will pay a community behavioral health services provider for peer support services if those services include – one-on-one or family activities designed to facilitate a smooth transition from an institutional setting to the community; – assisting the recipient or recipient's family in regaining balance and control of their lives; – enhancing the recipient's community living skills; and – supporting a self-directed recovery and independence; – are based on the unique therapeutic relationship between the provider, the recipient, and the recipient's family; – are coordinated in the recipient's behavioral health treatment plan; and – are focused on specific goals and objectives including identified benchmarks or other measurable outcomes. Peer support services must be provided by a behavioral health clinical associate who – maintains frequent in-person or telephonic contact with the recipient in order to support the recipient and participate in group activities; – is competent to provide peer support services by virtue of having experienced behavioral health issues in self or family; and – is supervised by a mental health professional clinician who the community behavioral health services provider has determined is competent to supervise peer support services by a behavioral health clinical associate. 30 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Subject to the limitation in 7 AAC 135.040, peer support services may only be offered in combination with – individual therapeutic behavioral health services for children under 7 AAC 135.220; – family therapeutic behavioral health services for children under 7 AAC 135.220; or – individual comprehensive community support services under 7 AAC 135.200. 6.4.12 Recipient Support Services 7 AAC 135.230 The department will pay a community behavioral health services provider for a recipient support service if that service – is medically necessary; – if provided during sleep hours, meets the requirements of this section; and – if provided during waking hours, meets the requirements of this section. The department will consider a recipient support service to be medically necessary only if the current need for that service is identified through a professional behavioral health assessment under 7 AAC 135.110 that – documents the recipient's history of high-risk behavior or the rationale for heightened vigilance; and – recommends the frequency and location where the service should be provided; and the recipient's behavioral health treatment plan clearly identifies – the recipient's target symptoms; and – how the staff of the community behavioral health services provider is expected to respond to and resolve a recipient's high-risk behavior. When recipient support services are provided to a recipient during the recipient's sleep hours, the individual rendering the service must be awake and able to hear or observe the recipient's behavior and, if that behavior puts the recipient or others at risk, respond to prevent harm to the recipient or others. If recipient support services are provided to a recipient during the recipient's waking hours, the individual rendering the service must be present and able to observe the recipient's behavior and, if that behavior puts the recipient or others at risk, respond to prevent harm to the recipient or others. The following elements of recipient support services are considered active treatment: – structure; – support; – sight or sound supervision. Recipient support services may be provided at – the recipient's residence; – the recipient's workplace; – the recipient's school; or – any other appropriate community setting specified in the behavioral health treatment plan. The department will pay a community behavioral health services provider for recipient support services provided to more than one recipient by the same staff during the same session if – each recipient lives in the same household; and – the service is provided to each recipient in accordance with this section. Recipient support services do not include the daily supervisory activities that 31 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – a parent or foster parent would normally carry out to assure protection, emotional support, and care of a child who is not a child experiencing a severe emotional disturbance; or – are normally provided by or within an assisted living facility, congregate housing facility, or group home for an adult who is not an adult experiencing an emotional disturbance; or an adult experiencing a serious mental illness. The department may pay for recipient support services while the recipient is concurrently receiving other behavioral health services if a recipient is at high risk of committing violence to self or others. For purposes of this subsection, a recipient is considered at high risk of committing violence to self or others if the recipient – has received a diagnosis with Axis I or Axis II disorders, according to the standards of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, adopted by reference in 7 AAC 160.900; the diagnosis may include a substance use disorder; – has a history of violence; the department will consider the frequency and circumstances in which the violence occurred; and – currently presents assaultive or threatening behavior; or delusions or command hallucinations of violent content. With prior authorization from the department, a recipient identified above may receive recipient support services provided concurrently from more than one individual during the same period. 6.4.13 Residential Substance Use Treatment Services 7 AAC 135.280 The department will pay a community behavioral health services provider for residential substance use treatment services if the provider is operating a structured residential program to treat substance use disorders in accordance with 7 AAC 70.120. To qualify for payment for providing residential substance use treatment services, a community behavioral health services provider must provide the following active treatment each day the recipient is in treatment: – teaching of life skills designed to restore or improve the recipient's overall functioning relative to their substance use disorder; – counseling focused on functional improvement, recovery, and relapse prevention; – encouraging and coaching. Residential substance use treatment services may be provided within the structured residential program as individual, group, or family services. The only behavioral health services that the department will pay for on the same day as residential substance use treatment services are – behavioral health screening under 7 AAC 135.100; – completing a client status review under 7 AAC 135.100; – needed professional behavioral health assessments under 7 AAC 135.110; – case management services under 7 AAC 135.180; – needed behavioral health clinic services under 7 AAC 135.010; – a medical evaluation. 32 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 6.4.13b Additional Requirements for Residential Substance Use Services 7 AAC 70.120 The department will approve a community behavioral health services provider that meets the requirements of this section to provide clinically managed low-intensity, medium-intensity, or high-intensity residential substance use treatment services. All residential substance use treatment services must include, at admission and during the course of active treatment as needed, – a substance use intake assessment conducted in accordance with 7 AAC 135.110(c) , or an integrated mental health and substance use intake assessment conducted in accordance with 7 AAC 135.110(d) ; if the assessment conducted under this paragraph is an integrated mental health and substance use intake assessment, only a physician, a physician assistant, an advanced nurse practitioner, or a mental health professional clinician may provide that assessment; and – development and maintenance of an individualized treatment plan that includes measurable short-term goals and objectives as needed in the areas of case management; addiction treatment; health care; mental health; social services; vocational services; and housing services. Residential substance use treatment services may be administered to an individual or a group, or on a family basis, but must include the following component services: – life skills development designed to restore or improve the recipient's overall functioning relative to the recipient's substance use disorder; – counseling to promote successful initial involvement in regular productive daily activity, including going to work or school, and successful reintegration into family living; – motivational and engagement strategies appropriate to the recipient's treatment plan; – medication administration services; only a physician, a physician assistant, an advanced nurse practitioner, a registered nurse supervised by a physician or advanced nurse practitioner, or a licensed practical nurse supervised by a physician or advanced nurse practitioner may provide medication administration services; – referrals to other agencies, as needed; – discharge or transfer planning; – comprehensive community support services; – crisis or relapse prevention planning; – management of a recipient's chronic disease, if medically necessary and clinically appropriate; – urinalysis and breathalyzer testing to reinforce treatment gains as appropriate to the treatment plan; – development of a social network that is supportive to recovery; – services provided to the recipient's family and significant other to support recovery and prevention; – didactic motivational interventions to assist the recipient in understanding the relationship between substance use disorder and attendant life issues; 33 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – development of coping skills in the recovery environment. All residential substance use treatment services must be medically necessary, clinically appropriate, and provided in accordance with the – ASAM Patient Placement Criteria for the Treatment of Substance-Related Disorders, adopted by reference in 7 AAC 70.910; and – Diagnostic and Statistical Manual of Mental Disorders, adopted by reference in 7 AAC 70.910. In addition to being delivered during regular business hours, all residential substance use treatment services must be delivered as needed during evening hours and on weekends. Clinically managed low-intensity residential substance use treatment services must – be delivered as a residential service on the premises of a community behavioral health services provider; – include five or more hours of clinical and therapeutic rehabilitative services per week; – be delivered in a structured recovery environment, staffed 24 hours a day, that provides sufficient stability to prevent or minimize the potential for recipient relapse or level of substance use that creates problems for the recipient; – include the availability of telephonic or in-person consultation with a physician, a physician assistant, an advanced nurse practitioner, or the emergency medical staff of a general acute care hospital 24 hours a day, seven days per week; – be provided with the appropriate medical, psychiatric, and psychological services on-site or closely coordinated off-site as determined by the severity and urgency of the recipient's condition; – be provided directly to a recipient by any of the following individuals, working within the scope of the individual's practice: a substance use disorder counselor; a behavioral health clinical associate; a mental health professional clinician; an individual with an active license under AS 08 to practice as (i) a physician; (ii) a physician assistant; (iii) an advanced nurse practitioner; (iv) a registered nurse supervised by a physician or advanced nurse practitioner; or (v) a licensed practical nurse supervised by a physician or advanced nurse practitioner; and – include access to nursing care and observation of the recipient as needed. Clinically managed medium-intensity residential substance use treatment services must – be delivered as a residential service on the premises of a community behavioral health services provider; – include 20 or more hours of clinical and therapeutic rehabilitative services per week; – include the availability of consultation with a physician, a physician assistant, an advanced nurse practitioner, or the emergency medical staff of a general acute care hospital 24 hours a day, seven days per week, including telephonic consultation available no later than eight hours after the provider's request for consultation; 34 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 in-person consultation available no later than 24 hours after the provider's request for consultation; – be provided with the appropriate medical, psychiatric, and psychological services on-site or closely coordinated off-site as determined by the severity and urgency of the recipient's condition; – be available 24 hours per day, must be provided on-site, and must be provided directly to a recipient by any of the following individuals, working within the scope of the individual's practice: a substance use disorder counselor; a behavioral health clinical associate; a mental health professional clinician; an individual with an active license under AS 08 to practice as (i) a physician; (ii) a physician assistant; (iii) an advanced nurse practitioner; (iv) a registered nurse supervised by a physician or advanced nurse practitioner; or (v) a licensed practical nurse supervised by a physician or advanced nurse practitioner; and – include access to nursing care and observation of the recipient as needed. Clinically managed high-intensity residential services must – be delivered as a long-term residential inpatient service on the premises of a community behavioral health services provider; – include 20 or more hours of clinical and therapeutic rehabilitative services per week; – include the availability of consultation with a physician, a physician assistant, an advanced nurse practitioner, or the emergency medical staff of a general acute care hospital 24 hours a day, seven days per week, including telephonic consultation available no later than eight hours after the provider's request for consultation; in-person consultation available no later than 24 hours after the provider's request for consultation; – be provided with the appropriate medical, psychiatric, and psychological services on-site or closely coordinated off-site as determined by the severity and urgency of the recipient's condition; – be available 24 hours per day, must be provided on-site, and must be provided directly to a recipient by any of the following individuals, working within the scope of the individual's practice: a substance use disorder counselor; a behavioral health clinical associate; a mental health professional clinician; an individual with an active license under AS 08 to practice as (i) a physician; (ii) a physician assistant; (iii) an advanced nurse practitioner; (iv) a registered nurse supervised by a physician or advanced nurse practitioner; or 35 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (v) a licensed practical nurse supervised by a physician or advanced nurse practitioner; and – include access to nursing care and observation of the recipient as needed. In this section, "telephonic" means two-way vocal communication by telephone or voice over internet protocol technologies. 6.4.14 Screening, Brief Intervention, and Referral to Treatment (SBIRT) 7 AAC 135.240 SBIRT is a comprehensive, integrated, public health approach to the delivery of early intervention and treatment services for persons with substance use disorders as well as those who are at risk of developing these disorders. Primary care centers, hospital emergency rooms, trauma centers, and other community settings provide opportunities for emergency intervention with at-risk substance users before more severe consequences occur. The service includes: – Screening - use of self-report questionnaires or structured interviews or similar screening techniques to detect substance use problems; identify the degree to which a person is at risk, and to identify the appropriate level of intervention as results indicate. – Brief Intervention - based on results of screening, if necessary, use of motivational discussion focused on raising a person’s awareness of their substance use, the potential harmful effects of that use, and encouraging positive change. Brief Intervention services may include: feedback goal setting coping strategies identification of risk factors information advice Referral to Treatment – if the screening reveals that the recipient meets any of the circumstances identified below, the community behavioral health services provider will refer the recipient to a behavioral health treatment program that will meet their needs – is at severe risk of substance use problems – is already substance dependent 6.4.15 Therapeutic Behavioral Health Services for Children 7 AAC 135.220 The department will pay a community behavioral health services provider for therapeutic behavioral health services, for a recipient under 21 years of age with a severe behavioral disorder, if those services – improve the recipient's overall functioning and reduce the likelihood of removal from a school setting; placement out of the family home; or referral to institutional care; – help the recipient's family to develop or improve specific child behavior management skills; – promote wellness, recovery, and resiliency; – help the recipient develop or improve specific age-appropriate social behavior; 36 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 develop or improve self-management skills that will support academic success; and make better behavioral choices within their family, school, and community overall; or assist the recipient in developing more functional coping strategies. Therapeutic behavioral health services for children may be provided – on the premises of the community behavioral health services provider, the recipient's home, the recipient's school, or any other appropriate community setting; – to an individual, family, or group. Therapeutic behavioral health services for children are limited to the following: – teaching of life skills designed to restore the recipient's functioning; – counseling focused on functional improvement, recovery, and relapse prevention; – encouraging and coaching. The department will not pay for therapeutic behavioral health services delivered in a classroom setting if those services are delivered by the teacher providing the academic program. The department will pay for therapeutic behavioral health services for children, when provided in a classroom setting, as a group session only if – all group participants have similar treatment needs; and – the individual rendering the services facilitates a group session outside the regular academic class at least twice per week for the purpose of creating a clear awareness among recipients of the specific in-class behaviors that are the focus of treatment; reviewing by means of the group process each recipient's strategies for success; facilitating the group's assessment of individual progress; and preparing each recipient in the group for the classroom. 6.4.16 Short-Term Crisis Stabilization 7AAC 135.160 The department will pay a community behavioral health services provider for short-term crisis stabilization services, provided by a substance use disorder counselor or a behavioral health clinical associate to a recipient, if that substance use disorder counselor or behavioral health clinical associate – provides an initial assessment of the recipient's overall functioning in relation to the shortterm crisis; – develops a short-term crisis stabilization plan; and – documents, on a form provided by the department, the assessment, a short-term crisis stabilization plan, and the services that are provided. The substance use disorder counselor or behavioral health clinical associate may provide, as part of the short-term crisis stabilization plan, any medically necessary and clinically appropriate behavioral health rehabilitation services necessary to return the recipient to the recipient's mental, emotional, and behavioral level of functioning before the short-term crisis occurred. Short-term crisis stabilization includes the following treatment and supports: – individual or family counseling needed in response to the short-term crisis; – individual or family training and education related to resolving the existing short-term crisis and preventing a future crisis; – monitoring the recipient for safety purposes; – any behavioral health rehabilitation services. 37 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Notwithstanding any behavioral health treatment plan in effect for the recipient at the onset of a short-term crisis, if a recipient is receiving short-term crisis stabilization services, the department will only pay for the behavioral health services identified in the short-term crisis stabilization plan for the duration of the short-term crisis stabilization. Short-term crisis stabilization must be documented on a contact form provided by the department. Documentation under this section must be filed in the recipient's clinical record. If the substance use disorder counselor or behavioral health clinical associate is unable to resolve the short-term crisis, a mental health professional clinician may assume responsibility for the case and begin providing short-term crisis intervention services under 7 AAC 135.160. Short-term crisis stabilization services may be provided in any appropriate outpatient or community setting, including – the premises of the community behavioral health services provider; – a facility designated for crisis respite purposes; and – the recipient's place of residence, workplace, or school NOTE: The crisis intervention/stabilization form can be obtained at the following website: http://dhss.alaska.gov/dbh/ under Resources Crisis Intervention/Stabilization Form (Word) and (PDF) 7.0 SERVICE AUTHORIZATION AND LIMITATION 7 AAC 135.040 7.1 Service Authorizations 7.1.1 Service Authorizations for Clinic Services 7 AAC 135.040 A community behavioral health services provider or mental health physician clinic may provide the following behavioral health clinic services without prior authorization from the department: – any combination of individual, group, and family psychotherapy, not to exceed 10 hours per recipient in a state fiscal year; – psychiatric assessments under 7 AAC 135.110(e) or (f), not to exceed four per recipient in a state fiscal year; – psychological testing and evaluation under 7 AAC 135.110(g) , not to exceed six hours per recipient in a state fiscal year, except that neuropsychological testing and evaluation is limited to 12 hours per recipient in a state fiscal year if the provider has documentation validating the provider's qualifications to provide neuropsychological testing and evaluation services; – pharmacologic management services, not to exceed one visit per recipient per week during the first four weeks after the recipient begins receiving pharmacologic management services, and, thereafter, not to exceed one visit per recipient per month as long as the recipient is receiving a service under this chapter, unless more frequent monitoring is required because of the requirements of the specific medication; or a recipient's unusual clinical reaction to a medication; 38 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 if the individual is not already receiving services under this chapter at the time the assessment is provided under this paragraph, one integrated mental health and substance use intake assessment under 7 AAC 135.110, or a combination of one mental health intake assessment and one substance use intake assessment under 7 AAC 135.110; the assessment or combination of assessments must consist of – one or more face-to-face sessions; and – a review of collaterally connected information; based on a current behavioral health treatment plan, one integrated mental health and substance use intake assessment under 7 AAC 135.110, or a combination of one mental health intake assessment and one substance use intake assessment under 7 AAC 135.110, every six months; short-term crisis intervention services under 7 AAC 135.160 that do not exceed 22 hours of the total short-term crisis intervention services provided to a recipient during a state fiscal year. 7.1.2 Service Authorization for Rehabilitation Services 7 AAC 135.040 A community behavioral health services provider may provide the following behavioral health rehabilitation services without specific authorization by the department: case management, not to exceed 180 hours per recipient per state fiscal year; no more than one hour per week per recipient may be used in monitoring by the directing clinician of the provision of services; individual therapeutic behavioral health services for children under 7 AAC 135.220, or a combination of individual therapeutic behavioral health services for children and peer support services under 7 AAC 135.210 and 7 AAC 135.220; the services or combination of services may not exceed 100 hours per recipient per state fiscal year; group therapeutic behavioral health services for children under 7 AAC 135.220, not to exceed 140 hours per recipient per state fiscal year; family therapeutic behavioral health services for children under 7 AAC 135.220, or a combination of family therapeutic behavioral health services for children and peer support services under 7 AAC 135.210 and 7 AAC 135.220; the services or combination of services may not exceed 180 hours per recipient per state fiscal year; individual comprehensive community support services under 7 AAC 135.200, or a combination of individual comprehensive community support services and peer support services under 7 AAC 135.200 and 7 AAC 135.210; the services or combination of services may not exceed 240 hours per recipient per state fiscal year; group comprehensive community support services under 7 AAC 135.200, not to exceed 140 hours per recipient per state fiscal year; recipient support services, not to exceed four hours per recipient per calendar day; medication administration services as provided in the recipient's behavioral health treatment plan; one medical evaluation of a recipient in a methadone treatment program per admission for that methadone treatment program, including – consultation and referral; – verification of addiction; and – establishing methadone dosage; methadone or antabuse administration as prescribed by a physician; detoxification services, with no limit; 39 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 behavioral health screening using the Alaska Screening Tool, adopted by reference under 7 AAC 160.900, to determine eligibility for admission to a treatment program, limited to one screening per program admission for new or returning recipients; medical evaluation for a recipient not receiving methadone, limited to one medical evaluation per recipient per admission to detoxification treatment; behavioral health treatment plan review for a recipient in a methadone treatment program, limited to one review per admission; day treatment services for children under 7 AAC 135.250, not to exceed 180 hours per state fiscal year; day treatment services may not be provided more than six hours per school day; screening and brief intervention services, with no limit; residential substance use treatment services under 7 AAC 135.280, with no limit; short-term crisis stabilization services under 7 AAC 135.170 that – do not exceed 22 hours of the total short-term crisis stabilization services provided to a recipient during a state fiscal year; and – are provided during a psychiatric emergency that is documented in the recipient's clinical record. 7.1.3 Service Authorization Procedures 7 AAC 135.040 A provider request for prior authorization of an extension of a service beyond service limitations or a provider request for a change in the level of the service that a recipient previously received must be made in writing on a form approved by the department. The request must – be documented in the clinical record prepared under 7 AAC 105.230 and 7 AAC 135.130; – include a listing of all Medicaid reimbursable services and the expected duration of these services as set out in the recipient's behavioral health treatment plan; and – affirm that the recipient's treatment team for a recipient under 18 years of age, in accordance with 7 AAC 135.120, has reviewed the behavioral health treatment plan and recommended the requested services as medically necessary and clinically appropriate. An extension made under this section is valid through the date set by the director of the division responsible within the department for behavioral health services, or the director's designee. The department will not pay for more than one service episode per day of a detoxification service. In this subsection, "service episode" means the completion of all services identified in this section for which a single payment is made in accordance with 7 AAC 145.580. After considering the area of the state where the service is provided, the provider's location, and whether other providers are available to a recipient, the director of the division responsible within the department for behavioral health services, or the director's designee, shall extend a behavioral health clinic service limitation under 7 AAC 135.010 - 7 AAC 135.290 if the director or director's designee determines that – the recipient's circumstances are exceptional; and – the extension is necessary to protect the recipient's health. 7.1.4 Out of State Placement Non-State Custody Children (Inpatient Psychiatric) 40 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 For any child not in state custody the State of Alaska Division of Behavioral Health (DBH) requires providers to complete a mandatory form requesting services as soon as an out-of-state admission may be advised. Providers must complete the form in its entirety prior to arranging for any out of state services. If you are unsure of whether your client will meet the criteria due to unforeseen circumstance discuss your concerns with the DBH staff. The form contains information on the process required to obtain out of state placement for youth The form requires providers to provide assessment and current treatment information on client. Providers may contact the State of Alaska Division of Behavioral Health Policy & Planning (907) 269-3600 or contact any of the following persons to discuss the process and/or obtain copies of the “request for out-of-state-placement” form. Judith (Judy) Helgeson (907) 269-3697 judith.helgeson@alaska.gov Valerie (Val) Kenny (907) 269-3797 valerie.kenny@alaska.gov Maureen McGlone (907) 269-3600 maureen.mcglone@alaska.gov Reta Sullivan (907) 269-8869 reta.sullivan@alaska.gov 8.0 DOCUMENTATION PROCESS STEPS 8.1. Request (Referral) for Services Each agency has a process for determining how a client will request services – Request for Services (form is developed by each agency) 8.2 Documentation Process with Alaska Automated Information System (AKAIMS) 8.2.1 Admission Including Minimal Data Set Requirements (AKAIMS) Admission information must be entered into the State of Alaska Automated Information System (AKAIMS). Training for entry of documentation into AKAIMS is provided by the state of Alaska Division of Behavioral Health upon request by the agency. See AKAIMS section for links to forms. An agency may choose to utilize AKAIM fully or elect to enter only the minimal data set. Following is a summarized list, in order of use, of required fields to meet AKAIMS minimal data set for reporting to the state. It does not explain any of the fields or questions; it simply lists them. See AKAIMS User Manual for a much more complete description of the database, and the Data Dictionary for explanations of fields. – Minimal Data Set Requirements (AKAIMS) Appendix C – Client List -Profile forms – Client Intake Form (To become a client of the agency) – Screening form (Alaska Screening Tool AST- required) – Client Status Review form Note: If client is not admitted after this point, stop here. Save and close this episode via the link at bottom of the Intake screen. Once admission is created in AKAIMS, Discharge becomes required. – Client Admission Form (admission to a specific program) The Client Admission Form is to be completed at first admission into a program at the beginning of a treatment episode. 41 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Entry of this form into AKAIMS establishes that the individual is admitted/enrolled in a program and receiving services. Fill in the blanks or check the boxes for each question. Do not leave anything blank. These are all required fields (“minimal data set”) for the State of Alaska and continued funding is contingent upon compliance with this state requirement. Notes (Encounter Data) Discharge Data 8.3 Medicaid and Best Practice Service Documentation Requirements 8.3.1 Medical Necessity 7 AAC 105 - 7AAC 160 While it is essential to have clinical documentation forms that allow for all necessary information to be captured, it is not enough to just have good forms. There must be clarity of how each document relates to and interfaces with treatment. It is critical to understand some practical and essential components of the assessment process, treatment planning, documentation of service delivery (progress notes), and review of treatment. The following information is based on State of Alaska Health & Social Services Medicaid regulations and Best Practices: The department will pay for a service only if that service is medically necessary as determined by criteria established under 7 AAC 105 - 7 AAC 160 or by the standards of practice applicable to the provider; All Treatment Must be Medically Necessary: – A qualified individual identifies behavioral health problems and treatment needs in an assessment or reassessment that meets industry standards – A qualified individual prescribes treatment objectives, services and active interventions in the behavioral health treatment plan derived from the assessment – Assessments are updated as new information becomes available – Services delivered are those prescribed – Services are delivered by qualified staff – Treatment progress is evaluated – Treatment changes are made accordingly – Discharge criteria identified 8.3.2 Assessment Once the identifying information is complete for administrative intake, it is time for the clinical assessment process to begin. The information listed here is for the most part in the order that it appears on the AKAIMS Behavioral Health Assessment Form. These are some areas of the initial clinical assessment that help focus treatment. Presenting Problem: Client statements of presenting problems/concerns & current status – This area of an assessment contains both the client’s direct statements of their concerns and/or presenting problems and the clinician/counselor understanding of the presenting problems. – Purpose Identify/document behavioral health problems Document client current life situation & historical data Document functional impairment 42 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Document that the Alaska Screening Tool (AST) was considered during the assessment Document that the Client Status Review (CSR) was considered during the assessment Determine proper diagnosis (DSM) Determine level of care (ASAM) for client’s with substance use issues Document treatment recommendations Include quotes from client whenever possible. Although the presenting problem may have been stated on a referral document or as part of the intake process it will need to be fully explored during the clinical assessment process. If you are using AK AIMS you will need to change the Presenting Problem in the Intake paperwork as it populates from there to the assessment The key to writing measurable goals/objectives is to be specific in stating the problem in the assessment. Vague problems result in vague goals that in turn result in vague service delivery. The symptoms of the Presenting Problems become the goals for treatment. The client may have difficulty stating the problem. The symptoms are often confused with the problem. It is up to the clinical staff to assist the client to clarify the problem. Mental Status Exam Clinical Impressions Summary – Include the following in this section a clinical interpretation of information gathered in the assessment process a description of symptoms that support the diagnosis a brief summary of the need for treatment and services Eligibility Summary – Summarize the recipient’s status as ED, SED-Child, SMI-Adult (SMI includes SEDA and CMI), and support for the determination of eligibility for the service categories to be recommended (clinic, rehab, RSS). Problem Summary List – Document each problem. If you choose you may complete AXIS IV before completing this area and transfer your findings to the problem summary area. When you complete the AXIS IV-Psycho Social Stressors, you will identify the problems and if you have specified (used “as evidenced by” statements) you may use this information to develop your Problem Summary List. When you specify or describe the problem with an “as evidenced by” statement you will have identified the symptoms. The symptoms will become the goals for treatment. You can then use the Problem Summary List to assist in developing your goals on your treatment plan. You may also use the information to assist you in completing the Recommendations for Treatment (services to be used). Strengths/Resources – Describe those strengths that are relevant to treatment, and that may assist in determining interventions or developing treatment strategies. For example, someone whose strengths include being very bright, sophisticated, and high functioning may respond to insight therapy or if a client is very motivated to make changes. Include the recipient’s support sources. Prognosis (circle one) Excellent Good Fair Poor – This section contains the clinician/counselor’s best predictions regarding the outcomes of the recommended treatment taking all the above gathered information into consideration. This can be provided on a problem-by-problem basis or as an overall prediction. 43 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Comments (include comments that support the prognosis) Services the Family Wants Recommendations – This area should reflect the services that will be used to address the problems identified in the Problem Summary List. The services should be identified by the Medicaid service name. All services documented in the treatment plan must first be recommended in an assessment. – This area is also where recommendations for additional assessments, medical visits, and services needed from outside of the agency sources are stated. Client Diagnosis – Mental disorders are diagnosed according to a manual published by the American Psychiatric Association called the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Persons using the DSM for diagnosis should be trained in its use Diagnosis should be conducted to identify illness and not label a person Diagnosis should be based on comprehensive information Culture and ethnic considerations are important in making a diagnosis A diagnosis should not lead to the assumption that all individuals having a disorder are alike in all important ways A DSM-IV diagnosis has five parts. Each part, called an axis, gives a different type of information about the diagnosis. – Axis I provides information about clinical disorders. Any mental health conditions, other than personality disorders or mental retardation, would be included here. Clinical Disorders are identified in 14 categories. i. Anxiety Disorders ii. Childhood Disorders iii. Cognitive Disorders iv. Dissociative Disorders v. Eating Disorders vi. Factitious Disorders vii. Impulse Control Disorders viii. Mood Disorders ix. Psychotic Disorders x. Sexual and Gender Identity Disorders xi. Sleep Disorders xii. Somatoform Disorders, xiii. Substance Related Disorders For Substance Related Disorder the following tool must be administered to determine placement needs. American Society of Addiction Medicine (ASAM) Patient Placement Criteria A tool for determining the intensity of care needed by clients with substance use disorders during treatment. Its use helps to place clients in the most appropriate level of care based on need and availability of service. This tool is located on the AKAIMS website. The training video is available at the following link. https://akdhss.adobeconnect.com/_a815866595/admissionasam/ 44 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 xiv. Adjustment Disorders (Other Conditions) These may also be a focus of clinical attention;” Other Conditions” include Medication-Induced Movement Disorders, Relational Problems, Problems Related to Abuse or Neglect, Noncompliance with Treatment, Malingering, Adult Antisocial Behavior, Child or Adolescent Antisocial Behavior, Age-Related Cognitive Decline, Bereavement, Academic Problem, Occupational Problem, Identity Problem, Religious or Spiritual Problem, Acculturation Problem, Phase of Life Problem – Axis II provides information about personality disorders and mental retardation and are recorded so the clinician will give consideration to additional intervention and treatment choices Mental Retardation- problems in brain development have usually occurred and virtually will affect all aspects of the individual's cognitive functioning. Borderline Intellectual Functioning may also be a clinical focus. There are varying degrees: i. Mild Mental Retardation ii. Moderate Mental Retardation iii. Severe Mental Retardation iv. Profound Mental Retardation Personality is the qualities and traits of being a specific and unique individual. - it is how we think, love, feel, make decisions and take actions. Personality is determined, in part, by our genetics and also, by our environment. Individuals with Personality Disorders have more difficulty in every aspect of their lives. Their individual personality traits reflect ingrained, inflexible, and maladaptive patterns of behaviors and impair the individual's ability to function in the daily activities of living. Personality Disorders include: i. Antisocial Personality Disorder ii. Avoidant Personality Disorder iii. Borderline Personality Disorder iv. Dependent Personality Disorder v. Histrionic Personality Disorder vi. Narcissistic Personality Disorder vii. Obsessive-Compulsive Personality Disorder viii. Paranoid Personality Disorder ix. Schizoid Personality Disorder x. Schizotypal Personality Disorder – Axis III: General Medical Conditions for reporting current medical conditions that are potentially relevant to the understanding or management of the individual's mental disorder. The purpose of distinguishing General Medical Conditions is to encourage thoroughness in evaluation/assessment and to enhance communication among health care providers. General Medical Conditions can be related to mental disorders in a variety of ways. It is clear the medical condition is directly related to the development or worsening of the symptoms of the mental disorder. The relationship between the medical condition and mental disorder symptoms is insufficient. 45 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 There are situations in which the medical condition is important to the overall understanding or treatment of the mental disorder. When there is no physician report containing the proper ICD-9- Code you write in what the client reports without providing a code. – Axis IV is used to describe psychosocial and environmental factors affecting the person. Be specific….”Problems with primary support group” would be more informative if it stated detail i.e. lost father age 13, removed from home age 6, victim of neglect first three years of life….. List other stressors even if POSITIVE that might help focus intervention and understanding “….note psychosocial and environmental problems occurring prior years if these clearly contribute to the mental disorder or have become a focus of treatment…..” List of psychosocial stressor categories i. Problems with primary support group Specify ii. Problems related to the social environment Specify ii. Educational problems Specify iii. Occupational problems Specify iv. Housing problems Specify v. Economic problems Specify vi. Problems with access to health care services Specify vii. Legal problems Specify viii. Readiness to change Specify ix. Relapse continued problem potential Specify x. Recovery Living environment Specify i. Other psychosocial stressor Specify – Axis V is a rating scale called the Global Assessment of Functioning; the GAF SCALE goes from 0 to 100 and provides a way to summarize in a single number just how well the person is functioning overall. Global Assessment of Functioning (GAF) Scale Part of DSM-IV Multi-axial System i. Measures "psychological, social, and occupational functioning": ii. 100 for the hypothetical healthiest patient; iii. 1 for the most ill patient A tool that has been widely accepted is the GAFTREE GAF rating represents Symptoms and Functioning - two scales rolled into one. Determine the symptom severity and the level of functioning based on scale criteria and use the results of the WORST effects of either symptoms or functional impairment to determine current GAF. Instructions on how to obtain training on this tool may be obtained from the Division of Behavioral Health. Recipient Support Services need to be identified as medically necessary through a professional behavioral health assessment that documents the recipient's history of high-risk behavior for violence or other rationale for heightened vigilance. The professional behavioral health assessment recommends the frequency and location where RSS services should be provided. – A recipient is considered at high risk of committing violence to self or others if the recipient 46 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 8.3.3 has received an Axis I or Axis II diagnosis (according to current DSM) has a history of violence currently presents i. assaultive or threatening behavior; or ii. delusions or command hallucinations of violent content Treatment Plan Must include: – Comprehensive diagnosis – List of members of interdisciplinary or interagency team when required – Problem statement – Measurable goals/objectives directly related to problems found in assessment – Documentation that the recipient, recipient’s parents, guardian or other legal representative actively participates, approves and signs plan – Specific services, intervention or activities provided by clinician – Frequency duration and target date of treatment Frequency is how often you will deliver services i.e. 1X per week Duration is the extent of each service provided i.e. 1 hour per session Target date for completion (should be completed or reviewed within the required client status review process (90-135 days)). – The target date for completion assists in determining the need for a Service Authorization. – Overseen by a qualified staff – Description of Problems, Goals, Objectives and Interventions Problem: An undesirable psychological state or ineffective or harmful behavioral pattern that is expressed in specific terms in a manner that is individualized and tailored to a unique consumer. Goals: Goals are based on identified problems and are what client wants to achieve. Clearly stated generally statements that the consumer has identified that describe a desired outcome. The symptoms of the problems as identified in an assessment will become the goals for treatment. Objectives: Objectives are what the client will do to achieve their goals. Measurable, observable behaviors, which have been identified as steps toward achieving the goal. Interventions: Activities done by a behavioral health specialist (mental health professional clinician, clinical associate, substance abuse counselor, etc.) aimed at meeting an identified goal/objective. 7 AAC 135.120. Behavioral health treatment plan (a) The department will pay a community behavioral health services provider or a mental health physician clinic for services provided to a recipient only if (1) those services are provided under an individualized behavioral health treatment plan that meets the requirements of 7 AAC 135.130; (2) the plan is based on a professional behavioral health assessment under 7 AAC 135.110; 47 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (3) the plan is signed and supervised by the directing clinician; (4) if the recipient is 18 years of age or older, the plan is (A) developed with the recipient or the recipient's representative; and (B) signed by the recipient or the recipient's representative; (5) if the recipient is under 18 years of age, the plan is (A) based upon the input of a treatment team that meets the requirements of (c) of this section; and (B) signed by the recipient or the recipient's representative; and (6) the plan remains current based upon the periodic client status review conducted under 7 AAC 135.100(c) . (b) By signing a behavioral health treatment plan, a directing clinician attests that in the directing clinician's professional judgment the services called for in the behavioral health treatment plan are (1) appropriate to the recipient's needs; (2) delivered at an adequate skill level; and (3) achieving the treatment goals. (c) A behavioral health treatment team for a recipient under 18 years of age (1) must include (A) the recipient; (B) the recipient's family members, including parents, guardians, and others similarly involved in providing general oversight of the recipient; (C) a staff member of the office in the department responsible for children's services, if the recipient is in the state's protective custody or supervision; (D) a staff member of the division in the department responsible for juvenile justice, if the recipient is in that agency's custody or care; (E) the directing clinician; and 48 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (F) the case manager, if the recipient is a child experiencing a severe emotional disturbance; and (2) may include (A) if the recipient currently resides within an alternative living arrangement, including foster care, residential child care, or an institution, a representative of that facility; (B) if the recipient is currently unable to succeed in a school, a representative from the recipient's public, private, or home educational system, including a teacher, special education consultant, speech therapist, or other representative involved in the recipient's education. (d) All members of the behavioral health treatment team shall attend meetings of the team in person or by telephone and be involved in team decisions unless the clinical record documents that (1) the other team members determine that participation by the recipient or other individual involved with the care of the recipient is detrimental to the recipient's well-being; (2) family members, school district employees, or government agency employees refuse to or are unable to participate after the provider's responsible efforts to encourage participation; or (3) weather, illness, or other circumstances beyond the member's control prohibits that member from participating. (e) If a provision of this chapter requires the approval, concurrence, or recommendation of the treatment team, the treatment team may issue that approval, concurrence, or recommendation only upon the concurrence of (1) the directing clinician; and (2) the recipient or the recipient's representative. AAC 135.130. Clinical record (a) To be eligible for payment under this chapter, a community behavioral health services provider, mental health physician clinic, or psychologist enrolled under 7 AAC 135.030(a) (3), must maintain, for each recipient served, a clinical record that includes the following: (7) a behavioral health treatment plan that meets the requirements of 7 AAC 135.120 and includes (A) the recipient's identifying information; 49 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (B) the date implementation of the behavioral health treatment plan will begin; (C) treatment goals that are directly related to the findings of a professional behavioral health assessment provided under 7 AAC 135.110; (D) the services and interventions that will be employed to address the written goals; (E) the name, signature, and credentials of the directing clinician; and (F) the signature of the recipient or the recipient's representative; (d) The clinical record must reflect all changes made to a recipient's behavioral health treatment plan and professional behavioral health assessment. 8.3.4 Progress Notes (encounter notes, miscellaneous notes, non-episode notes) Medicaid is a medical insurance program that reimburses for the provision of services to eligible recipients. To support the billing for a service, a service note must support that the service that was billed and paid for was actually provided. AAC 135.130. Clinical record (a) (8) a progress note for each service for each day the service is provided, that is signed by the individual provider, and that includes (A) a description or listing of the active treatment provided; (B) the date the service was provided; (C) the duration of the service expressed in the service unit or clock time used to determine the payment rate under 7 AAC 145.580; (D) the treatment goals that the service targeted; (E) a description of the recipient's progress toward those treatment goals; and (F) the name, signature, and credentials of the individual who rendered the service. (b) A provider of Medicaid behavioral health services shall retain a record of any service provided to the recipient in accordance with 7 AAC 105.230 even if the recipient is not currently receiving services. (c) To document active treatment, the provider must set out a description or a listing of the active interventions that the provider provides to, or on behalf of, the recipient. There are three types of notes in the Alaska Information Management System (AK-AIMS) – Encounter Note -This is a progress note describing delivery of a billable service to a client with an open/active chart – Miscellaneous Note - This is a progress note describing delivery of a non- billable service or contact with a client with an open/active chart 50 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – Non-Episode Note - This is a progress note describing contact with a client that does not have an open/active chart with your agency. You must have established a profile for the client and you may link to this encounter type through the profile area. The components of a progress note that meets Medicaid regulations are as follows: – Client identifying information – For each service delivered, there must be one note, per provider, per day – Notes have to be dated – Type of service delivered – Amount of time spent providing the service needs to be documented – Start and stop times are required for time-based services/codes – Goal being addressed – Description of the active treatment/interventions directed toward the goal being addressed – A clinical interpretation of how the consumer responded to the intervention. – Clinically relevant information – Progress toward the identified treatment goal addressed in the session – Plan for ongoing treatment (best practice) – Signed, dated and credentialed by provider. Progress note tips – Progress notes must be based on services as identified in the treatment plan. – Some measurement tools include: Yes / Partial/ No - either met, partially met, or did not meet sessions goal/objective Counting - i.e. 90 days without being hospitalized, No more than 3 temper tantrums per week, will identify at least X# of friends, measurement scales – Notes that do not contain information about what a provider did do not substantiate the billing and may be subject to repayment in the case of an audit. – Progress notes must also contain sufficient information about what a provider did to substantiate the payment for the service provided. – Use words that describe what you actually did. Do not think that you have to use any “special”, “magical” or “code” words to write a clinically relevant note. – The active staff intervention used and documented in the note must be identified in a current treatment plan and must utilize a service that supports the intervention. – Start and stop times are required for the following time-based services/codes Code Code Ending Effective 12/31/2012 1/1/2013 Service Description Units 90804 90832 Psychotherapy, Individual 30 minutes 90806 90837 Psychotherapy, Individual 60 minutes 90810 90832 Psychotherapy, Individual 30 minutes 90812 90837 Psychotherapy, Individual 60 minutes 96101 no change Psychological Testing 1 hour 96118 no change Neuropsychological Testing 1 hour 8.3.5 Client Status Review (CSR) Process – Treatment Reviews The Client Status Review (CSR) form is required and must be completed every 90-135 days while client status is active. If the CSR is not current any service delivered during the time that 51 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 is out of compliance is considered to be not Medically Necessary and therefore is not a billable service. AKAIMS provides instructions for the treatment review in the AKAIMS User Manual https://akaims-support.dhss.alaska.gov/training.htm These instructions include: – Review process of Client Status Review (CSR) 7 AAC 135.100. – ASAM for substance abuse clients The treatment review process evaluates and documents progress toward each goal area from the treatment plan Determines whether there are new behavioral health problems during review period Includes recommended changes to the treatment plan Review process is supervised by the directing clinician (qualified staff includes a mental health professional clinician at a minimum for clients with a mental health diagnosis or a qualified substance use counselor for substance using clients.) AAC 135.100. Behavioral health screening; client status review 7 AAC 135.100. (a) The department will pay a community behavioral health services provider for conducting a behavioral health screening using the Alaska Screening Tool, adopted by reference under 7 AAC 160.900, provided by the department. A community behavioral services health provider must complete a behavioral health screening for each new or returning recipient of behavioral health services before a professional behavioral health assessment is conducted for that recipient under 7 AAC 135.110. (b) The department will pay a community behavioral health services provider for completing, in accordance with (c) of this section, a client status review with the recipient present, if the client status review is completed and used as relevant clinical information concurrent with (1) an initial professional behavioral health assessment under 7 AAC 135.110 for a new or returning recipient; (2) a client status review under (c)(6) of this section; (3) a client status review under 7 AAC 135.120(a) (6); or (4) at discharge from treatment. (c) A client status review completed with the recipient present must be (1) administered using the department's Client Status Review form, adopted by reference under 7 AAC 160.900, or administered using the electronic version of that form, by means of the Alaska Automated Information Management System; (2) used to assist in determining a recipient's functioning in the life areas identified on the form; 52 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (3) used by the directing clinician to assist in measuring the outcomes of behavioral health treatment provided; (4) used by the directing clinician in making treatment decisions; (5) used by the directing clinician to revise the recipient's behavioral health treatment plan; and (6) administered and reviewed every 90 to 135 days (A) while the recipient is in treatment; or (B) from the date the behavioral health treatment plan was last reviewed. (d) Each time a client status review is completed, the community behavioral health services provider shall (1) include a copy of the client status review in the recipient's clinical record; and (2) report the client status review data to the department. (e) In this section, "in treatment" means the recipient is receiving or is ready to begin receiving services from a community behavioral health services provider who is providing or ready to begin providing the services identified in a behavioral health treatment plan approved by the recipient and directing clinician. AAC 135.130. Clinical record (d) The clinical record must reflect all changes made to a recipient's behavioral health treatment plan and professional behavioral health assessment. 8.3.6 Discharge Planning 7 AAC 70.990. (9) Definitions "Discharge or transfer planning" means the planning necessary for a recipient to make a smooth transition away from active involvement with treatment services or from one level of care to another level of care; – Phasing from one level of care to another, possibly between programs – Treatment plan follows client – Changes in service intensity should be a gradual process – Treatment ends when client is ready to self- manage recovery Discharge must include a Client Status Review 7 AAC 135.100. Discharge planning is required under the “Standards of service” section of the interim standards for operation7 AAC 70.220. (7) Discharge planning includes making appropriate referrals, providing appropriate information, and coordinating services with other service providers to ensure continuity of care when a recipient transfers to another provider or is discharged from services. 53 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 9.0 CIVIL COMMITMENT 9.1 Requirements for Civil Commitment 9.1.1 Judicial Orders A judge may order a local mental health professional designated as evaluation personnel to conduct a mental health evaluation of a person allegedly to be mentally ill. If that mental health evaluation determines a person to be gravely disabled or to present a likelihood of serious harm to self or others, a judge may issue an ex parte order (orally or in writing), stating that there is probable cause to believe the person is mentally ill and that condition causes the person to be gravely disabled or to present a likelihood of serious harm to self or others. Within 48 hours, the court will appoint an attorney to represent the person alleged to be mentally ill, and may direct that a peace officer take that person into custody and deliver the person to the nearest appropriate facility for emergency examination or treatment. In an area in which no designated evaluation facility exists, a mental health professional designated as evaluation personnel may conduct a mental health evaluation of a person to determine whether the person being evaluated requires hospitalization on an emergency basis. The mental health professional that performs the emergency examination must have reason to believe that the person is: – mentally ill and that condition causes the person to be gravely disabled or to present a likelihood of serious harm to self or others and – is in need of care or treatment The mental health professional may hospitalize the person or arrange for hospitalization, on an emergency basis. If a judicial order has not been obtained, the mental health professional applies for an ex parte order authorizing hospitalization for evaluation. 9.1.2 Mental Health Evaluations A mental health professional conducts the mental health evaluation required for the purposes of determining the specific mental health problems and needs of the patient. The mental health evaluation must document: – involuntary commitment criteria: that the person is mentally ill and is likely to cause harm to self or others, or is gravely disabled that the evaluator has considered less restrictive alternatives available to treat the person and protect others or, if a less restrictive involuntary form of treatment is sought, specify the treatment and the basis for supporting it there is reason to believe that the person’s mental condition could be improved by the course of treatment recommended that treatment facility recommended, or a less restrictive alternative is appropriate to the person’s condition and that treatment program has agreed to accept the recipient that the person has been advised of the need for treatment, but will not accept voluntarily, and request that the court commit the person to the specified treatment facility or less restrictive alternative for a period not to exceed 30 days the evaluator must identify prospective witnesses who will testify in support of commitment 54 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 the evaluator must document facts and specific behavior the person exhibited that supports the need for involuntary commitment an interview with the peace officers who brought the patient to the facility for the examination a brief history of the patient, including observations or information obtained by other persons relating to the background, development, and circumstances of the patient's current problems a brief evaluation of the patient's mental status a history of the patient's previous treatment and medication a diagnosis a determination of whether the recipient meets the involuntary commitment criteria – If the mental health professional determines that the patient meets the involuntary commitment criteria and will not accept treatment on a voluntary basis, the mental health professional shall develop a treatment plan for the patient's care in the least restrictive setting (which may be hospitalization). – If the mental health professional determines that the person being evaluated is mentally ill, gravely disabled, or presents a likelihood of serious harm to themselves or others, and that person is in need of hospital care or treatment, mental health professional may initiate involuntary commitment by arranging hospitalization of that person in an appropriate local facility for a period not to exceed 72 hours for evaluation. If the mental health professional conducting the mental health evaluation determines that the patient does not meet the involuntary commitment criteria the mental health professional will develop an appropriate outpatient referral plan for the purpose of follow-up and continuing care if the recipient is in need of services. 9.1.3 Definitions Designated Treatment Facility-Means a hospital, clinic, institution, center, or other health care facility that has been designated by the department for the treatment or rehabilitation of mentally ill persons but does not include correctional institutions. Ex Parte Order- The term "ex parte" in the law means that something is done with regard to another party without that party present. Gravely Disabled- Means a condition in which a person as a result of mental illness is in danger of physical harm arising from such complete neglect of basic needs for food, clothing, shelter, or personal safety as to render serious accident, illness, or death highly probable if care by another is not taken; or will, if not treated, suffer or continue to suffer severe and abnormal mental, emotional, or physical distress, and this distress is associated with significant impairment of judgment, reason, or behavior causing a substantial deterioration of the person's previous ability to function independently. Mental Health Professional- Means a psychiatrist or physician who is licensed by the State Medical Board to practice in this state or is employed by the federal government; a clinical psychologist licensed by the state Board of Psychologist and Psychological Associate Examiners; a psychological associate trained in clinical psychology and licensed by the Board of Psychologist and Psychological Associate Examiners; a registered nurse with a master's 55 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 degree in psychiatric nursing, licensed by the State Board of Nursing; a marital and family therapist licensed by the Board of Marital and Family Therapy; a professional counselor licensed by the Board of Professional Counselors; a clinical social worker licensed by the Board of Social Work Examiners; and a person who – has a master's degree in the field of mental health – has at least 12 months of post-masters working experience in the field of mental illness and – is working under the supervision of a type of licensee listed above Minor- Means an individual who is under 18 years of age. Peace Officer- Means: – an officer of the state troopers – a member of the police force of a municipality – a village public safety officer – a regional public safety officer – a United States marshal or deputy marshal – an officer whose duty it is to enforce and preserve the public peace 10.0 INFORMATION RESOURCES 10.1 State of Alaska Division of Behavioral Health 10.1.1. New Integrated Behavioral Health Regulations 10.1.2 Division Grantee Providers Current list of behavioral health providers that are receiving a grant from the State of Alaska Division of Behavioral Health 10.1.3 Review On-Site Provider Training Trainings that have been provided by the State of Alaska Division of Behavioral Health and their designees 10.1.4 Regulation Clarification Process “The Regulations Clarification Process” is designed to help providers get answers to questions regarding to the behavioral health regulations. The Dept. has established a formal internal mechanism to research and develop responses to provider inquiries. This internal review may result in a simple explanation of the meaning and intent of the regulations, or it could result in a formal interpretation of the regulations which provides greater direction. O Simple or common answers and explanations will typically result in an addition to the “Frequently Asked Questions” document. Formal interpretations become published Regulation Clarifications that have operational authority, and will be included in subsequent versions of the billing manual. – Clarification Request form - Word – Clarification Request form - PDF 10.1.5 Standardized Instrument Resources 56 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Alaska Screening Tool Client Status Review Alaska Screening Tool Guide Crisis Intervention/Stabilization Form Service Authorization Form 10.1.6 Provider Communications Correspondence to providers is updated routinely and agency clinical staff should periodically review on DBH website at: http://dhss.alaska.gov/dbh/Pages/Resources/Regulations.aspx 10.1.7 Medical Assistance Billing & Payment Services, Policies and Procedures ( Includes revision history) Professional Claims Management General Program Information 10.1.8 Alaska Department of Health and Social Services Frequently Asked Questions (FAQs) The Division of Behavioral Health has scheduled a weekly teleconference for provider agencies. The intent is to lend ongoing support and technical assistance specific to the implementation of the new Integrated Behavioral Health Regulations. Submitted questions are vetted through this process. The submitted questions may have been received during Integrated Regulation Training events, provider submissions through the “Regulation Clarification Process”, or as a result of contact with the Division. No formal sign-up is required. However, providers are encouraged to designate staff to participate in order to reduce the number of obligated telephone lines. Day: Every Wednesday Time: 8:30 – 9:30 a.m. Call-in Number: 1-800-315-6338 access code: 3408 # Staff Contact: 907-269-3617 10.1.9 Division of Behavioral Health Responses to Provider Questions Provider Technical Assistance Training Introduction & Objectives Regulations Transition, Applicability and Scope Provider Agency Requirements Information Resources for Recipients, Client Rights & Eligibility Department Approval National Accreditation & Interim Standards Requirements for Program Staff Clinical Documentation Requirements Covered Services, Billing, Payment & Post Payment Activities Service Authorization Training Detoxification Services Residential SUD Treatment 10.1.10 Regional Providers 57 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Anchorage Regional Providers Northern Regional Providers Southcentral Regional Providers Southeast Regional Providers 10.1.11 Programs AKAIMS https://akaims-support.dhss.alaska.gov/training.htm Alaska Psychiatric Institute Policy & Planning Prevention & Early Intervention Medicaid and Quality Section Treatment & Recovery 10.1.12 Statewide Resources (including Statewide Directory for All State Programs) Advisory, Advocacy, & Planning Boards Clinical Documentation Division Initiatives Documents & Publications Treatment & Recovery Forms Frequently Asked Questions (FAQ's) Division of Behavioral Health GAFTREE HIPPA Lending Library Motivational Interviewing Power Point National Accreditation Performance Management System Policies & Procedures Licensing Professionals – AS 08.29.010 Professional Counselors – AS 08.64.010 State Medical Board – AS 08.63.010 Marital and Family Therapists – AS 08.95.010 Board of Social Work Examiners – AS 08.68.010 Board of Nursing – AS 08.84.010 Physical Therapy and Occupational Therapists – AS 08.86.010. Psychologists and Psychological Associates Regional Provider Websites Training & Conferences 10.2 Alaska Automated Information System (AKAIMS) 10.2.1 https://akaims-support.dhss.alaska.gov/training.htm 58 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 10.3 All Statutes and Regulations www.legis.state.ak.us/folhome.htm Alaska Administrative Code The following Citations identify regulations that pertain to Behavioral Health Services – AAC 70 -- Behavioral Health Services – AAC 100 - 130 -- Medicaid Coverage (conforming amendments) – AAC 135 -- Medicaid Coverage; Behavioral Health Services – AAC 140 - 160 -- Medicaid Coverage/Payment (conforming amendments) 10.4 Medicaid Related Community Behavioral Health Clinic Policy and procedures Billing Manual – Services, Policies and Procedures (includes changes, service limits and descriptions) – Professional Claims Management – General Program Information Provider Announcement – Service Authorizations (11.18.2011) Community Behavioral Health Clinic Service Authorization Request 10.4.1 XEROX (Affiliated Computer Services, Inc.) Fiscal Agent -Contracted with the Department of Health and Social Services Xerox-Affiliated Computer Services, Inc (ACS) 1835 South Bragaw Street, Suite 200 Anchorage, Alaska 99508-3438 Anchorage: (907) 644-6800 Outside Anchorage: (800) 770-5650 (In State Toll Free) 10.4.2 “Forms" Provider Enrollment Application forms You will find form information under the Provider tab at the top of the web page 10.4.3 “Updates” for Behavioral Health Billing Manual Providers and medical billers should check the Provider Updates(Revision History) page regularly for revisions, clarifications and new information pertaining to their practice. We strongly recommend that you print the relevant updates and keep them with your billing manual. 10.4.4 “Training" View the Training Schedule You will find training information under the training tab at the top of the web page 10.4.5 “Contact Us” For Designated Work Units, Staff, Mailing Addresses, etc.You will find this information under the contact tab at the top of the web page 10.4.6 Keys for Achieving Success in Billing/Payment Read and maintain your billing manual Verify recipient eligibility 59 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Verify eligibility code Verify dates of eligibility Verify Third Party Liability Verify the services you are eligible to provide Verify procedure codes Obtain Service Authorization, if applicable File your license renewals and/or certification/permits timely (keep your enrollment current) Ensure completion of claim forms (reference provider manual) Document Third Party Liability payment on claim, if applicable Include attachments as required File timely Reconcile payments (Remittance Advice (RA) Statements) Read and distribute RA messages Address problems/issues promptly Call Provider Inquiry with questions NOTE: The clinical record must document the problems identified during the professional behavioral health assessment and client status review processes, including functional deficits that require behavioral health treatment in order to be a reimbursable service. 11.0 POLICIES AND PROCEDURES 11.1 Rural Tribal Providers Boiler Plate Policies and Procedures 11.1.1 Policies and Procedures List The following Information may be reviewed at http://behavioralhealthcompliancesolutions.com/documents-ruralprovider Alternative Accreditation Process Behavioral Health Clinic Services Behavioral Health Rehabilitation Services Excluding Residential Substance Abuse And Detoxification Services Behavioral Health Services Clinical Documentation Processes Choosing A National Accreditation Organization Civil Commitment Emergency Transportation And Accommodations Services Initial Services/Screening Interim Standards Non-Emergency Transportation And Accommodations Services Non-Emergency Transportation And Accommodations Services Requiring The Division Of Behavioral Health Approval–Substance Abuse Detoxification And Residential Treatment Programs 60 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Non-Emergency Transportation And Accommodations Services Requiring The Division Of Behavioral Health Approval–For Children’s Residential Treatment Services Professional Behavioral Health Assessments Progress Notes Recipient Eligibility Service Authorization And Limitations Excluding Residential Substance Abuse And Detoxification Services Staff Qualifications Telemedicine Treatment Planning DBH guidelines used to document the above regulations – DHSS / Behavioral Health “Guidelines for Writing Policies & Procedures” – Policy & Procedure template Attachments/Forms documented in Boiler Plate Regulations – Accreditation Presentation-Ceils – AKAIMS User Manual Minimal Data Set 101107 v2.0 base – Alaska Medical Assistance Program Policies and Claims Billing Procedures for Community – Alaska Screening Tool – Client Release of Confidential Information for Substance Abuse Treatment Travel – Client Status Review – COA CARF comparison – COA Process Brochure – Community Behavioral Health Clinic Service Authorization Request 7112 – Crisis Intervention/Crisis Stabilization Form – DBH Request for Substance Abuse Supported Travel Assistance 2012 – DBH Request for Substance Abuse Supported Travel Assistance Instructions 2012 – FAQs-Integrated Regulation Training questions – Get Started (CARF) – Joint Commission Accreditation Redefined – NATIONAL ACCREDITATION AGENCIES Crosswalk – Readiness Checklist for Joint Commission Behavioral Health Care Accreditation – Service Authorization Form for Community Behavioral Health – SBIRT INTEGRATED SCREENING TOOL FORM EXAMPLE – SBIRT Whitepaper SAMSHA – The Medical Assistant Transportation Authorization And Invoice (AK-04) – Value of BH Accreditation 12.0 MEDICAID ENROLLMENT 12.1 Medicaid Description http://dhss.alaska.gov/dhcs/Pages/medicaid_medicare/default.aspx Medicaid is an “entitlement program” created by the federal government, but administered by the state, to provide payment for medical services for low-income citizens. People qualify for 61 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Medicaid by meeting federal income and asset standards and by fitting into a specified eligibility. Under federal rules, DHSS has authority to limit services as long as the services provided are adequate in “amount, duration, and scope” to satisfy the recipient’s medical needs. Medicaid began as a program to pay for health care for poor people who were unable to work. It covered the aged, the blind, and the disabled and single parent families. Over the years, Medicaid has expanded to cover more people. For instance, children and pregnant women may qualify under higher income limits and without asset limits. Families with unemployed parents may qualify, and families who lose regular Family Medicaid because a parent returns to work may continue to be covered for up to one year. There have also been changes in the eligibility rules for people who need the level of care provided in an institution, such as a nursing home. Now, most Alaskans who need — but cannot afford — this expensive care may qualify for Medicaid. In addition, recent changes within the Alaska Medicaid program give some people who need an institutional level of care the opportunity to stay at home to receive that care. 12.2 How to Apply for Medicaid There should be an internal process for signing up clients and tracking their eligibility while they are in service. All agencies should have applications on hand. 12.2.1 Offices for getting help with Medicaid To apply for Medicaid services please contact the Division of Public Assistance. – Applications, office locations, and useful information can be found on this web site. Eligibility Requirements: Current Medical Assistance Income Standards Denali Kid Care - Health insurance for low-income pregnant women and children/teens 12.2.2 Electronic tracking system All agencies should verify recipient eligibility for new clients and have a process to routinely track eligibility while client is in service. – Eligibility Verification System (EVS) (Detailed instructions) – Providers may use EVS 24 hours a day, 7 days a week – To access the Alaska EVS, dial: •800.884.3223 (Toll-free) Recipient Eligibility Fax form 907.644.8126 Eligibility for up to 30 individuals or dates of service can be verified per telephone call – EVS contains the most recent 12 months of eligibility history 13.0 BILLING 13.1 General Information for Billing 13.1.1 Tracking Billing Information Suggestions The following information may be useful to verify that an agency’s billing process is covering needed areas or to assist an agency in developing a billing process. This information may be modified to accommodate agency needs. 62 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Your agency Medicaid Service Authorization form may be used to develop a billing sheet or verify that your billing sheet reflects the most current services code information. Community Behavioral Health Clinic Service Authorization Request Your agency’s appointment calendar could be used to determine that all appointments with clients result in an encounter note. This could be verified by matching the appointment calendar information to your electronic data entry system entry reports. Alaska Medical Assistance provides an electronic claim submission software program called Payerpath. This software is available at no cost to the provider. For more information refer to Index at http://medicaidalaska.com/dnld/PBM_Prof_Claim_Mgmt.pdf Many agencies use an employee timesheet or log. The following is an extract from an example of a time log. This log format or a similar one could be used as a time management tool for employees and as a tool to verify that all billable services delivered are accounted for during billing process. EMPLOYEE DAILY TIME LOG DEPARTMENT: _____________________________ DATE: ________________________ EMPLOYEE NAME: ______________________ SIGNATURE: _______________________ SUPERVISOR NAME: ____________________ SIGNATURE: ________________________ Client Time Start/Stop Time (clock (Use service name on Other Time Include brief description- a hours) billing sheet) few words) NonStart Stop Total Billable Billable Administrative Time Time time Service Service Duties Travel Other Print one copy for each day of work, for each employee. A description of fields to be filled in the work log sheet are: 1. Date: The date for which the work log sheet is being prepared. 2. Department: The department in which the employee works. 3. Employee Name/Signature: The employee who is recording his work activities on the log sheet. 4. Supervisor Name/Signature: The supervisor or manager to whom the employee reports. 5. Start/Stop Time: Employee is required to fill in the work activity times for entire daily shift (in clock hours). (Add as many lines to log as necessary to accommodate number of start/stops time changes) 6. Client Time: Name of service delivered. The allowable services are listed on the agency billing sheet. 7. Other Time: Include brief description (a few words) Helpful Tips for Billing/Payment Steps: 63 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – Read and maintain your provider billing manual. This step is essential to having a successful billing system. The Provider Billing Manual is divided into 3 Sections i. ii. iii. Services, Policies and Procedures (includes service limits and descriptions) Professional Claims Management General Program Information – Xerox, Inc. offers training on how to bill claims in a timely manner. Medicaid related Training information is available at http://www.medicaidalaska.com/providers/Training/materials.shtml – File your license renewals and/or certification/permits timely (keep your enrollment current) – All agencies should verify recipient eligibility for new clients and have a process to routinely track eligibility while client is in service. You may access the User Guide at Eligibility Verification System (EVS) Verify recipient eligibility Verify eligibility code (Designates the services that client is eligible to receive through Medicaid) Verify dates of eligibility Verify Third Party Liability (Any additional insurance other than Medicaid) – Verify the services you are eligible to provide (Use your current billing sheet or the information on the current Medicaid Service Authorization form Community Behavioral Health Clinic Service Authorization Request ) – Verify procedure codes (Use your current billing sheet or the information on the current Medicaid Service Authorization form Community Behavioral Health Clinic Service Authorization Request – Have a formal documented process to ensure that claims are submitted i.e. if your agency uses an employee time log you can verify that there is a billable note for each billable entry on log. – Ensure completion of claim forms Refer to the Professional Claims Management section in your Provider Billing Manual Document Third Party Liability payment on claim, if applicable Include attachments as required All the current forms, fax coversheets, and attachments are available on the Alaska Medicaid website at http://medicaidalaska.com/providers/forms.shtml – File timely. All claims must be filed within 12 months of the date services were provided to the patient. The 12 month timely filing limit applies to all claims, including those that must first be filed with a third-party carrier. In these cases, providers must bill Alaska Medical Assistance within 12 months of the service date and attach explanation of benefits documentation from the third-party carrier to the Alaska Medical Assistance claim. The timely filing limit may be extended under some conditions. Please refer to your Provider Billing Manual/ Claims Submission for further details. (Use index for exact location): http://medicaidalaska.com/dnld/PBM_Prof_Claim_Mgmt.pdf 64 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – Reconcile payments. Read and distribute RA messages. Verify that the claims submitted are accurately paid by matching the remittance advice to the information submitted for payment. If your agency has a printout of the claims submitted you can use the printout or you could use the billing sheets. (Due to the confidential information in the actual encounter notes they should not be used by accounting for payment verification. Please refer to your Provider Billing Manual/ Claims Submission for further details. (Use index for exact location): http://medicaidalaska.com/dnld/PBM_Prof_Claim_Mgmt.pdf – Remittance Advice. The remittance advice (RA) is a claim status report. It is produced weekly for any Alaska Medical Assistance enrolled provider when there is claim activity to report, such as payment, denial, adjustment, pended claim, or claim requiring additional information. It tells the provider the status of each claim submitted for processing. Following the cover page, an RA is organized into the following sections: i. Remittance advice messages ii. Paid and denied claims iii. Explanation of benefits (EOB) status codes (denial/error codes) iv. Remittance summary v. Resubmission turnaround documents (RTD), if any vi. ClaimCheck® edits, if any NOTE: NOTE: The Adjustment Claims, Voided Claims, and In-Process Claims sections are repeated as necessary to report all the types of claims a provider files; for example, primary service, Medicare crossover claims, etc. – It is important for providers to read the RA each week to stay informed of provider news and events; providers should also reconcile the RA each week in order to keep up with adjusted or denied claims and any RTDs needing attention. Providers can use their RA to i. Review submitted claims status ii. Identify claims which require further action iii. Learn about changes in Alaska Medical Assistance policy, reimbursement, and other guidelines – If a provider requests, Xerox will transmit the RA electronically as a data file that many practice management software systems can recognize and manipulate. It can be used to post payments or to create or post to an aging report. Xerox will also continue to send the RA in paper form. Providers must submit HIPAA compliant 837 transactions in order to receive an 835 transaction response. – To receive the RA electronically each week, complete an Electronic Remittance (835) Authorization Form, found at http://medicaidalaska.com/providers/forms.shtml. – Address problems/issues promptly – Have a written procedure for turnaround time on all Claims and Adjustments submitted for payment 65 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 – Call Provider Inquiry with questions Provider Inquiry/Provider Services (8:00AM – 5:00PM, Monday – Friday) (907) 644-6800 (option 1) (In Anchorage) (800) 770-5650 (option 1, 1) (Outside Anchorage) 14.0 QUALITY ASSURANCE 14.1 Evaluation Tool Use of an Evaluation Tool is helpful when reviewing your clinical chart to ensure compliance with Medicaid regulations. A copy of an Evaluation Tool with Regulation Citations may be downloaded from http://behavioralhealthcompliancesolutions.com/documents-ruralprovider You may also cut and paste the following copy and modify it to fit your agency needs. CLINICAL EVALUATION TOOL Provider Name: Reviewer Name & Date: Ye ALASA SCREENING TOOL # No s REQUIREMENTS A Is the AST Present & Complete? B. Was the AST completed before the assessment was conducted for the recipient? C.C. Is there documented evidence that the results of the AST was reviewed and considered during the assessment? # Ye N CLIENT STATUS REVIEW s o REQUIREMENTS A 135.130(a)(2) Is the CSR present as part of the clinical . record? B Was the initial CSR completed with the . recipient physically present and administered using the department’s current CSR form? C Was the CSR used by the directing clinician . in making treatment decisions? D Was the CSR administered and reviewed . every 90 to 135 days? Recipient Initials: Medicaid Recipient: (Circle) Yes Comment or No Regulation Enter Date: 135.130(a)(1) 135.100(a) 135.110(h) Comment Regulation Enter Date: 135.100(c)(1) 135.100(c)(4) 135.100(c)(6)( A)&(B) 66 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 E . F . G . Was the CSR used by the directing clinician to assist in measuring the outcomes of the behavioral health treatment provided? Was the CSR used by the directing clinician to revise the recipient’s behavioral health treatment plan? Was the CSR used to assist in determining a recipient’s functioning in the life areas identified on the form? # Yes No TREATMENT PLAN REQUIREMENTS A. Is there a date that TX plan implementation will begin? B. Does the TX plan document the recipient’s identifying information? C. D. E. F. G. H. I. J. Are the TX goals directly related to the findings of the behavioral health assessment? Are the services and interventions that will be employed to address the written goals documented? Does the TX plan identify the goals, objectives, services, and interventions selected to address a recipient's behavioral health needs identified by a professional behavioral health assessment under 7 AAC 135.110? Do the selected services and interventions detail the frequency and duration? If the recipient is under 18 years of age, did the TX plan document the treatment team members and their ability to participate in the TX planning session? Is the TX plan remaining current based upon the periodic client status review? Are the name, signature, and credentials of the directing clinician present on the TX plan? Is the name and signature of the recipient or the recipient’s representative present on the TX plan? 135.100(c)(3) 135.100(c)(5) 135.100(c)(2) Comment Regulation Enter Date: 135.130(a)(7)( B) 105.230(b); & 135.130(a)(7)( A) 135.130(a)(7)( C) 135.130(a)(7)( D) 135.990(7)(A)( i) 135.990(7)(A)( ii) 135.120(a)(5); & 135.120(c) 135.120(a)(6) 135.130(a)(7)( E) 135.130(a)(7)( F) 67 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 # A. B. C. D. E. F. Yes No MENTAL HEALTH ASSESSMENT REQUIREMENTS Was the assessment conducted upon admission? Does the assessment document the recipient’s mental status, social and medical history? Does the assessment document functional impairments? (that substantially interferes with or prevents them from achieving or maintaining one or more developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills) Is there a complete DSM diagnosis consistent with multi-axial classification? (If a diagnosis exists) Does the written report document the problems identified during the professional behavioral health assessment and client status review processes, including functional deficits that require mental health treatment? Does the assessment document the nature and severity of any identified mental health disorder? G. Are treatment recommendations that include services identified as treatment needs, which form the basis of a subsequent behavioral health treatment plan documented within the assessment? H. Does the assessment document recipient’s eligibility for the recommended services? Comment Regulation Enter Date: 135.110(b)(3) 135.110(b)(3)( A) 135.110(b)(3)( E); & 135.990(92). 135.110(b)(3)( C); 135.130(a)(3)( A); & 105.230(d)(1) 135.130(a)(3)( B) 135.110(b)(3)( B) 135.110(b)(3)( D); & 135.130(a)(3)( C) 135.010(a)(3)( A) 70.050; & 135.020 68 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 I. J. K. If, during the assessment, evaluation, or treatment of a child experiencing an emotional disturbance, a provider determines that the recipient may have a severe behavioral health disorder and that the recipient is in need of behavioral health rehabilitation services, did the provider refer the recipient to a provider that provides behavioral health rehabilitation services in the community? Was the assessment conducted by a mental health professional clinician? Was the assessment updated as new information became available? Yes No SUBSTANCE USE ASSESSMENT REQUIREMENTS Was the assessment conducted upon admission? B. Does the assessment document functional impairments? (that substantially interferes with or prevents them from achieving or maintaining one or more developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills) C. Does the written report document the problems identified during the professional behavioral health assessment and client status review processes? D. Does it document the recipient has a substance use disorder? E. Does it identify the correct diagnosis? # A. F. Does it document the nature and severity of any identified substance use disorder? 135.020(c) 135.010(b)(1) 135.110(b)(4) Comment Regulation Enter Date: 135.110(c)(3) 135.110(c)(3)( E); & 135.990(92) 135.130(a)(4)( B) 135.110(c)(3)( A) 135.110(c)(3)( C); 135.130(a)(4)( A); & 105.230(d)(1) 135.110(c)(3)( B) 69 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 G. Are treatment recommendations that include services identified as treatment needs, which form the basis of a subsequent behavioral health treatment plan documented within the assessment? H. Does the assessment document recipient’s eligibility for the recommended services? If, during the assessment, evaluation, or treatment of a child experiencing an emotional disturbance, a provider determines that the recipient may have a severe behavioral health disorder and that the recipient is in need of behavioral health rehabilitation services, did the provider refer the recipient to a provider that provides behavioral health rehabilitation services in the community? Was the assessment conducted by a substance use disorder counselor, social worker, or other qualified program staff member performing duties regularly within the scope of the individuals authority, training and job description; however, if substance use intake assessment is conducted as part of detoxification services subject to 7AAC 70.110 and 7AAC 135.190, the assessment must be conducted by an individual identified in 7AAC 70.110 for the type of detoxification service provided. Was the assessment updated as new information became available? I. J. K. # Yes No INTEGRATED BH ASSESSMENT REQUIREMENTS A. Was the assessment conducted upon admission? B. Does the assessment document the recipient’s mental status, social and medical history? 135.110(c)(3)( D); & 135.130(a)(4)( C) 135.010(a)(3)( A) 70.050; 135.020 135.020(c) 135.110(c)(2) 135.110(c)(4) Comment Regulation Enter Date: 135.110(b)(3); & 135.110(c)(3) 135.110(b)(3)( A) 70 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 C. D. E. F. G. Does the assessment document functional impairments? (that substantially interferes with or prevents them from achieving or maintaining one or more developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills) Does the written report document the problems identified during the professional behavioral health assessment and client status review processes, including functional deficits that require mental health treatment? Is there a complete DSM diagnosis consistent with multi-axial classification? (If a diagnosis exists) (both mental health & substance use diagnoses if applicable) Does the assessment document the nature and severity of any identified mental health disorder and/or substance use disorder? Are treatment recommendations that include services identified as treatment needs, which form the basis of a subsequent behavioral health treatment plan documented within the assessment? (In relation to both mental health and substance use) H. Does the assessment document recipient’s eligibility for the recommended services? I. If, during the assessment, evaluation, or treatment of a child experiencing an emotional disturbance, a provider determines that the recipient may have a severe behavioral health disorder and that the recipient is in need of behavioral health rehabilitation services, did the provider refer the recipient to a provider that provides behavioral health rehabilitation services in the community? 135.110(b)(3)( E); 135.110(c)(3)( E); & 135.990(92) 135.130(a)(3)( B) 135.110(b)(3)( C); 135.130(a)(3)( A); & 105.230(d)(1) 135.110(b)(3)( B); 135.110(c)(3)( B) 135.110(b)(3)( D); 135.130(a)(3)( C); 135.110(c)(3)( D); & 135.130(a)(4)( C) 135.010(a)(3)( A) 70.050; & 135.020 135.020(c) 71 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 J. K. # A. B. C. D. E. F. G. H. I. J. K. Yes N o Was the assessment conducted by a mental health professional clinician? Was the assessment updated as new information became available? 135.010(b)(1) PSYCHIATRIC ASSESSMENT Comment REQUIRMENTS Does the assessment include a date that Enter Date: the assessment was conducted? Does the assessment document the recipient’s identifying information? Does the assessment include a description of the symptoms that need medical care? Does the assessment include a description of how the symptoms established the medical necessity for, and clinical appropriateness of, treatment? If medication is prescribed, a description of the symptoms that the medication is intended to target? Does the assessment include relevant recipient history? Did the assessment include a review of any general medical and psychiatric history or problem(s) the recipient is presenting? Was a mental status examination completed? During the mental status examination, was the recipient’s: thoughts, moods, selfidentity, insight, judgment, memory, speech, intellectual functioning, time-andplace orientation, and reasoning or problem-solving ability to assist in establishing a diagnosis and case formulation, assessed? Does the assessment document functional impairments? (that substantially interferes with or prevents them from achieving or maintaining one or more developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills) Does the assessment include a list of psychiatric problems? Regulation 135.110(d)(4); & 135.110(c)(4) 135.130(a)(6)( B) 135.130(a)(6)( A) 135.130(a)(6)( C)(i) 135.130(a)(6)( C)(ii) 135.130(a)(6)( D) 135.110(e)(3) 135.110(e)(2) 135.110(e)(4) 135.990(18) 135.110(e)(6); & 135.990(92) 135.110(e)(6) 72 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 L. Is a complete diagnosis present and consistent with multi-axial classification used in the DSM? M. Are treatment recommendations that include services identified as treatment needs, which form the basis of a subsequent behavioral health treatment plan documented within the assessment? Does the assessment document recipient’s eligibility for the recommended services? If, during the assessment, evaluation, or treatment of a child experiencing an emotional disturbance, a provider determines that the recipient may have a severe behavioral health disorder and that the recipient is in need of behavioral health rehabilitation services, did the provider refer the recipient to a provider that provides behavioral health rehabilitation services in the community? Was the assessment completed by a licensed physician, licensed physician assistant, or licensed ANP who is enrolled as a dispensing provider and who has prescription authority? Does the assessment include the name, signature, and credentials of the medical professional conducting the assessment? N. O. P. Q. # Yes No PROGRESS NOTE REQUIREMENTS A. Is the date of service included in the note? B. C. Does the note identify the service rendered? Is the duration of the service expressed correctly in either units or clock time? 135.110(e)(5); & 135.130(a)(6)( E) 135.110(e)(6) 135.010(a)(3)( A) 70.050; 135.020 135.020(c) 135.010(b)(2) 135.130(a)(6)( F) Comment Regulation Enter Date: 105.230(d)(6); & 135.130(a)(8)( B) 105.230(d)(6) Circle: Clinic or Enter Service Type: Enter # of units: or Enter Start Time: & Rehab 105.230(d)(5); & 135.130(a)(8)( C) 73 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Enter Stop Time: D. Does the note document a description or listing of the active TX provided? To document active treatment, the provider must set out a description or a listing of the active pre-planned specific interventions that the provider provides to, or on behalf of, the recipient to assist them in achieving the goals documented in the treatment plan. Are the treatment goals that the service is targeted for documented? 135.130(a)(8)( A); 135.130(b); & 135.990 F. Is a description provided for the recipient’s progress toward the TX goals? 135.130(a)(8)( E) G. Are the name, signature, and credentials of the individual who rendered the service present? 105.230(d)(6); & 135.130(a)(8)( F) E. 135.130(a)(8)( D) Comments: _____________________________________________________________________________________ 14.2 AKAIMS Reports for Tracking Compliance AKAIMS provides multiple reports for assisting providers with ensuring documentation compliance https://akaims-support.dhss.alaska.gov/files/training/0705/AKAIMS%20Report%20Menu.pdf Service Delivery Model Chart and table that illustrate the service category counts, proportions of clinical vs., rehab, and frequency of use for service codes within a date range. Admission AST and Initial CSR Count Provides a count of Admission profiles completed, count of ASTs completed, and a count of Intake CSRs in a given date range. AK Screening Results by Provider Report for agencies that gives the number of Alaska Screening Tool Results for a specified date range. The report also offers the number that screened positive for Substance Abuse, Mental health, TBI, FASD and Dual Diagnosis. AKAIMS Production Totals 74 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 Counts the number of Client profiles, Intake transactions, ASTs, Admission Profiles, Program Enrollments, Discharges, and CSRs by type, in a given time period. AKAIMS Client Status Review Findings A CSR report that is date range controlled and provides client ID, Intake date, Subsequent date, Intake CSR average, Subsequent CSR average. This report also matches and then reports on those client IDs that have an intake CSR that is associated with a follow-up CSR. AST CSR Year to Year Counts This report give a totals number of CSRs and ASTs in a given time period, it then compares those numbers to the same period of time in the previous year, providing a % of change over the two time periods. Compared Substances at admission Chart This chart illustrates the count of admissions in a time period and graphically displays the differences in the counts of two compared substances that clients indicated as abused substances at time of admission. Agency Productivity This report provides a detailed count of client services rendered and the medicade costing for those services. There are five levels to this report; Agency, program, rendering staff, client, and service details. Minimal Data Set Lists the clients in a agency that have had an intake transaction completed and then notes all activities that the client record has, included is a status of those activities relevant to minimal data set completion. 14.3 Internal Quality Assurance Process Each agency develops their internal quality assurance policy A Quality Assurance and Improvement process should provide continuous monitoring, evaluation, and implementation of improvement. The process should include the following components. – Develop, evaluate, and monitor processes that are in compliance with Division of Behavioral Health regulations – Have written process to analyze data and interpret findings – Have written process to implement corrective action 14.4 Policy & Procedures Required by Regulation for Quality Assurance AAC 70.220. Standards of service. A behavioral health services provider must (1) use appropriate and comprehensive standardized assessments to evaluate the needs of each recipient entering and receiving ongoing treatment by the provider; (2) develop written comprehensive treatment plans based upon the assessed needs of the recipient; 75 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (3) document new recipient orientation to services and all recipient participation in the development and implementation of treatment plans; (4) render only those services that are documented in the treatment plan as medically necessary, clinically appropriate, and based on the assessed needs of the recipient; (5) document all clinical services in a timely manner; (6) provide services in a way that is culturally sensitive to the state's diverse population; and (7) make appropriate referrals, provide appropriate information, and coordinate services with other service providers to ensure continuity of care when a recipient transfers to another provider or is discharged from services. AAC 70.225. Internal service structure. For each category of service provided by a behavioral health services provider, that provider must (1) have in writing (A) a service description; (B) a service philosophy; and (C) service goals; (2) establish procedures for crisis intervention, including screening recipients for risk to self or others; (3) provide clinical supervision to all personnel providing clinical or direct services to a recipient; and (4) conduct regular quality assurance reviews that (A) monitor the quality of the service; (B) monitor the appropriateness of service; and (C) are used to identify training needs and improve the quality of the service. AAC 70.230. Medication management. A behavioral health services provider must 76 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (1) have comprehensive written policies and procedures that cover all aspects of medication management; and (2) conduct a periodic review and evaluation of the provider's compliance with its own medication management policies and procedures. (Eff. ___/___/2011, Register _____) AAC 70.235. Infection control. A behavioral health services provider must implement an infection control program that reduces a staff member's or recipient's risk of infection. The provider must periodically evaluate the infection control program for effectiveness and make any changes that are needed AAC 70.240. Performance measures and quality improvement. A behavioral health services provider must (1) promote a culture within its own organization that promotes excellence and continual quality improvement; (2) establish policies and procedures for identifying and analyzing critical incidents and sentinel events; (3) collect data for the purpose of monitoring performance, managing risk, and improving service delivery; and (4) be able to show how the data collected under this section is used to implement changes that increase quality of care, manage risk, and decrease the number of critical incidents or sentinel events AAC 70.245. Leadership. A behavioral health services provider must (1) establish policies and procedures for organizational governance and responsibility; (2) have an active governing body empowered to guide, plan, and support the provider in achieving its mission and goals; (3) have a written description of the provider's leadership structure, including a description of the roles and responsibilities of each level of leadership; (4) demonstrate effective leadership within all areas of the provider's organization by having leaders who 77 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (A) engage in both short- and long-term strategic planning; (B) communicate effectively with staff and recipients; (C) develop and implement policies and procedures that guide the business and clinical operations of the provider; (D) establish the mission and direction of the organization; (E) are responsible for ongoing performance improvement and achievement of established outcomes; and (F) solicit and value feedback from recipients, personnel, and other stakeholders to create services that meet or exceed the expectations of recipients; (5) comply with all federal, state, and local laws; and (6) be financially solvent and adhere to established accounting practices. AAC 70.250. Physical environment. A behavioral health services provider must (1) maintain a safe, healthy, and therapeutic physical environment for providing services; (2) monitor the provider's environment and make any necessary changes; (3) develop and implement an emergency management plan, including the conduct of practice drills; and (4) develop and implement a risk management plan designed to reduce the risk of harm to a person, property, or the ability of the provider to meet the requirements of this chapter. (Eff. ___/___/2011, Register _____) AAC 70.255. Human resources. A behavioral health services provider must (1) have a sufficient number of qualified staff to meet recipient needs and the performance expectations of the provider; (2) hire only those individuals who are qualified to perform the duties assigned; (3) provide initial orientation to new staff members; 78 2/8/2016 TRIBAL RURAL BEHAVIORAL HEALTH CLINICAL HANDBOOK DESK GUIDE Provided by the State of Alaska, Department of Health &Social Services, Division of Behavioral Health DRAFT VERSION February 2013 (4) establish minimum qualifications for each job classification; (5) perform and document an annual evaluation for each staff member; (6) require personal accountability from each staff member for that staff member's work performance; and (7) implement a system for managing staff caseloads to support high quality care AAC 70.260. Information system management. A behavioral health services provider must (1) ensure that the provider's management information system is secure and protects the privacy and confidentiality rights of the recipients; and (2) maintain a complete and accurate clinical record system. (Eff. ___/___/2011, Register _____) AAC 70.900. Voluntary surrender; disciplinary actions (a) If the department determines that a behavioral health services provider is not in compliance with this chapter or the provider's action or inaction is placing the health, safety, or well-being of a recipient in jeopardy, the department may (1) request voluntary surrender of an approval; (2) impose a temporary or permanent special condition on the provider's approval; (3) impose a specific probationary period during which the provider must correct the deficiencies that the department has identified; (4) suspend the provider's approval for a specific period of time; (5) revoke the provider's approval. (b) The department will suspend or revoke a provider's approval if, during a probationary period imposed under (a)(3) of this section, a provider fails to correct the deficiencies that the department has identified. (c) The department will notify a provider of its intention to impose a special condition, impose a probationary period, suspend an approval, or revoke an approval under (a)(2) - (5) of this section in accordance with AS 44.62.330 - 44.62.630, including a provider's right to appeal that action. 79 2/8/2016